1 Workshop Expectations Behave in a professional manner
1
Workshop Expectations Behave in a professional manner! Demonstrate respect for others Be considerate Be on time for workshop and from breaks Turn cell phones and other electronics off Respect confidentiality! Participate in group discussions 2
Preface to The Oregon Intervention System In 1989 a task force was assigned to develop a behavior intervention system that would be effective in keeping vulnerable individuals safe when they engaged in dangerous behaviors. The Department of Human Services (DHS) wanted a system that would utilize non-aversive techniques, avoid the use of punishment, and maintain the dignity of all individuals. 3
Preface to The Oregon Intervention System After evaluating scores of different systems from across the United States, DHS determined that the system that most closely embraced Oregon’s values was Professional Assault Response Training (PART©). Dr. Paul Smith, founder of PART©, worked with professionals in Oregon to adapt his training curriculum to meet the specific Oregon Administrative Rules (OARs) for the populations which the new system would serve. 4
Preface to The Oregon Intervention System Oregon’s original adaptation of the curriculum, PART-Revised (PART-R©) eventually evolved into PART-Oregon (PART-OR), which then evolved into Oregon Intervention System (OIS) and became the official system delivering positive behavioral support to adults and children with Intellectual/Developmental Disabilities. 5
Preface to The Oregon Intervention System Over the years, OIS became stereotyped as a system or a training where participants would learn how to do “restraints” or “holds” Although this was never an accurate representation of the philosophy of OIS, the stereotype affected the culture of OIS. Participants would come to the workshops with this preconceived stereotype which affected their First Impressions of the OIS system. 6
Preface to The Oregon Intervention System First Impressions First impressions are based upon a appearance and any knowledge we have about an individual. We make judgments and assign stereotypes based upon our first impressions. Our first impressions can change the way we and others interact with others. 7
Preface to The Oregon Intervention System https: //www. youtube. com/watch? v=w. T 9 Pd. S 9 h. PFs 8

Preface to The Oregon Intervention System Stereotypes What are some of your stereotypes of OIS? How do you believe they were formed? Would you agree that in the absence of reliable information, we tend to: Make judgments based upon our previous experiences Repeat responses that we have used in the past 9
Oregon Intervention System (O. I. S. ) OIS is an evidenced based system designed for Direct Support Professionals, Families, Foster Care Providers, and Personal Support Workers in understanding, preventing, and responding to challenging behavior, through Positive Behavioral Intervention Support. 10
OIS: The “System” Includes Organizational structure Implementation Support Philosophy 11
This Workshop will include: Module 1: Values and OIS Module 2: Understanding How We Develop Module 3: Trauma Module 4: Mental Health Disorders Module 5: The Biopsychosocial Approach Module 6: Positive Behavioral Intervention Support Basic Behavior Management Module 7: Models for Changing Challenging Behavior Module 8: Communication & Power Struggles Module 9: Stress and Self-Control Module 10: Crisis Management 12
13 MODULE 1 Values and OIS
Values 14 What are values? How are they formed? Are they static or dynamic? Exercise List 10 of your values
Values 15 Values are shaped by our worldview and drive our behavior. Values guide us when we make choices about what we think is right or wrong. Values are principles for living that we take seriously enough to practice.
Values 16 What do you believe are the values of OIS? Who do you believe determines the values of OIS? Do your personal values fit together with the OIS values?
Values of OIS 17 Respecting rights, treating others with dignity, and acknowledging their citizenship. Person Centered: Behavioral challenges are approached on an individual basis. Although similarities may occur, each behavioral challenge is unique to the person. Behavioral challenges are complex and require a team-based collaborative decision-making process.
Values of OIS 18 Challenging behaviors are approached from the evidenced based framework of Positive Behavioral Intervention Support. The core principles of OIS emphasize the importance of proactive and preventative strategies rather than “reactive” strategies.
Values of OIS 19 Professional Integrity To take responsibility for one’s behavior and do what is right when no one is observing. To not disregard the well being, dignity, or safety of those who depend on our support. To not misuse the resources of the individual or the supporting network. To honor the directive to be a Mandatory Reporter of abuse and neglect.
Integrity 20 Beliefs Actions Words
Values: Class Discussion 21 How will your personal values influence the quality of your work? What challenges your personal values in the workplace?
If our actions are congruent with our values then there would be no more. . . 22
23 ABUSE AND NEGLECT
Abuse Definition 24 Financial Exploitation Physical Abuse Sexual Abuse Verbal Abuse Involuntary Seclusion
Neglect Definition 25 Failing to provide care or supervision to maintain physical and mental health that may result in physical harm or significant emotional harm. Willfully withdrawing or neglecting duties and obligations as a Direct Support Professional or Personal Support Worker.
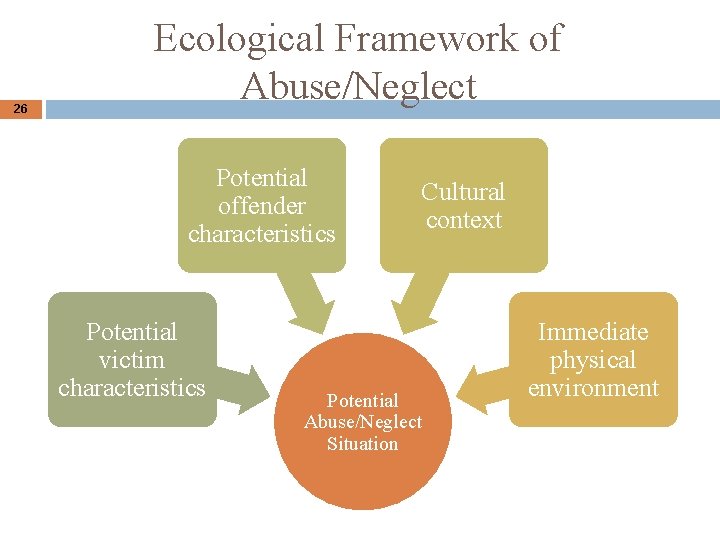
26 Ecological Framework of Abuse/Neglect Potential offender characteristics Potential victim characteristics Cultural context Potential Abuse/Neglect Situation Immediate physical environment
Abuse/Neglect Prevention 27 Have a personal Self-Control Plan Hold your fellow teammates accountable Create a work culture that values the person you support. Manage your stress both at home and at work.
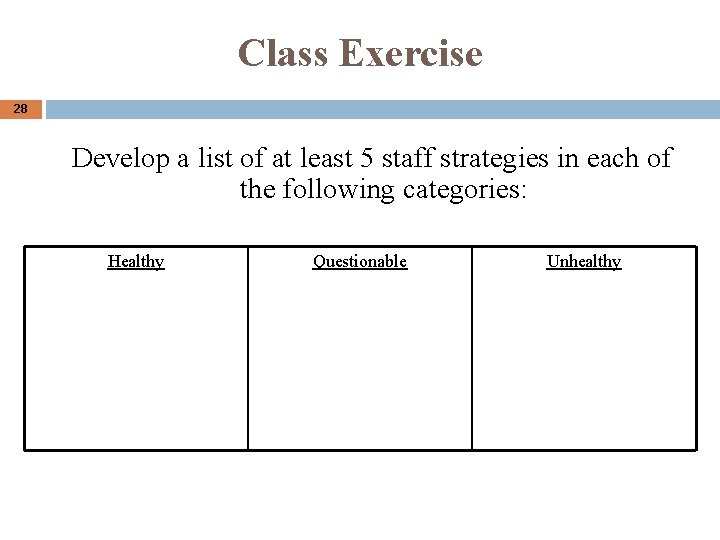
Class Exercise 28 Develop a list of at least 5 staff strategies in each of the following categories: Healthy Questionable Unhealthy
Understanding How We Develop Module 2 Factors Influencing the Development of Our Brains �(Preset) 29
Challenging Behaviors are a result of thinking (a cognitive process). Therefore, we must understand how our brains develop and work. 30
Understanding How We Develop Common known factors influencing our development: �Environment �Premature Birth �Genetics 31
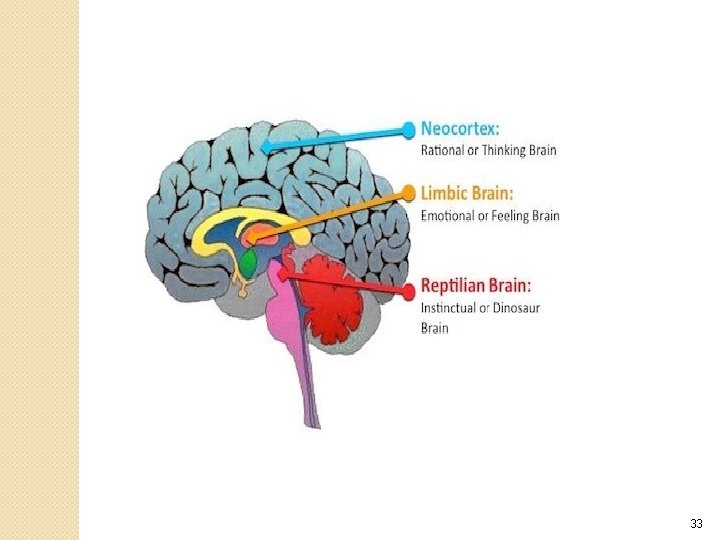
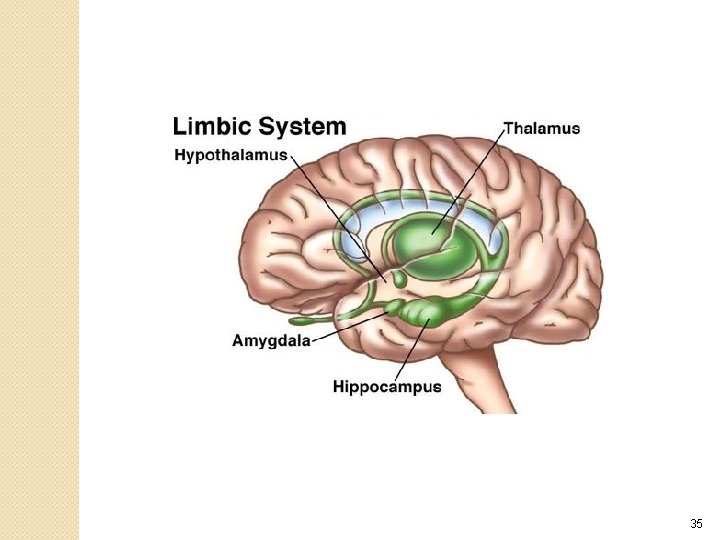
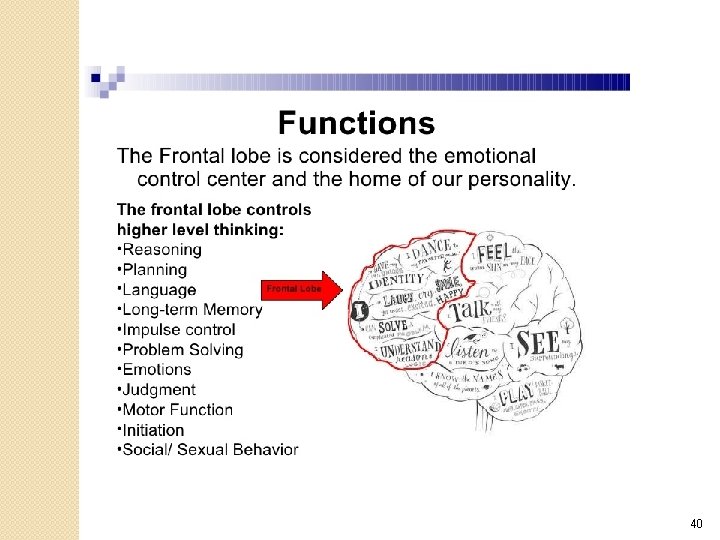
Understanding How We Develop Our brain forms from the “bottom up”, that is the primitive sections to the more sophisticated sections (Perry, 2000). v First to develop are the brainstem and midbrain that govern necessary bodily functions for life. v The higher regions of the brain develop more thoroughly after birth which regulate emotions, language, and abstract thought. 32
33
The Emotional Brain 34
35
The Emotional Brain and Regulation �The capability to respond, to manage, and maintain daily emotions that may make us feel uncomfortable is difficult for many individuals. �To interpret how our emotions are demonstrated through our actions (behaviors) and perceived by others, then adjust accordingly, takes time to learn. 36
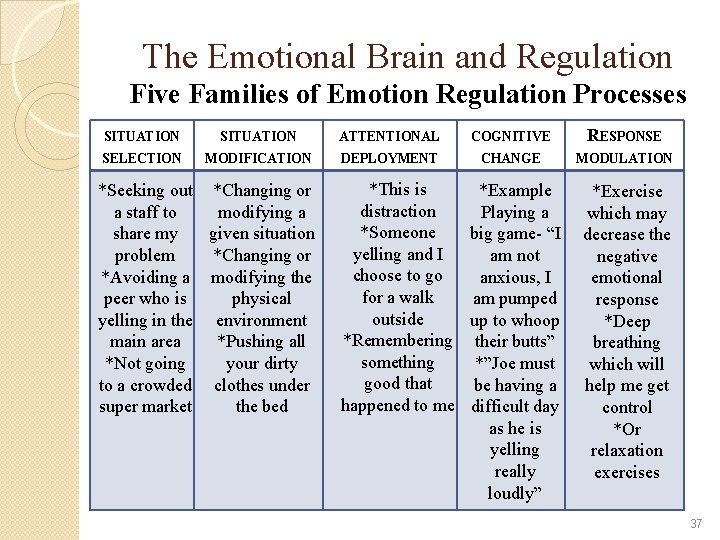
The Emotional Brain and Regulation Five Families of Emotion Regulation Processes SITUATION ATTENTIONAL COGNITIVE RESPONSE SELECTION MODIFICATION DEPLOYMENT CHANGE MODULATION *Seeking out *Changing or a staff to modifying a share my given situation problem *Changing or *Avoiding a modifying the peer who is physical yelling in the environment main area *Pushing all *Not going your dirty to a crowded clothes under super market the bed *This is *Example distraction Playing a *Someone big game- “I yelling and I am not choose to go anxious, I for a walk am pumped outside up to whoop *Remembering their butts” something *”Joe must good that be having a happened to me difficult day as he is yelling really loudly” *Exercise which may decrease the negative emotional response *Deep breathing which will help me get control *Or relaxation exercises 37
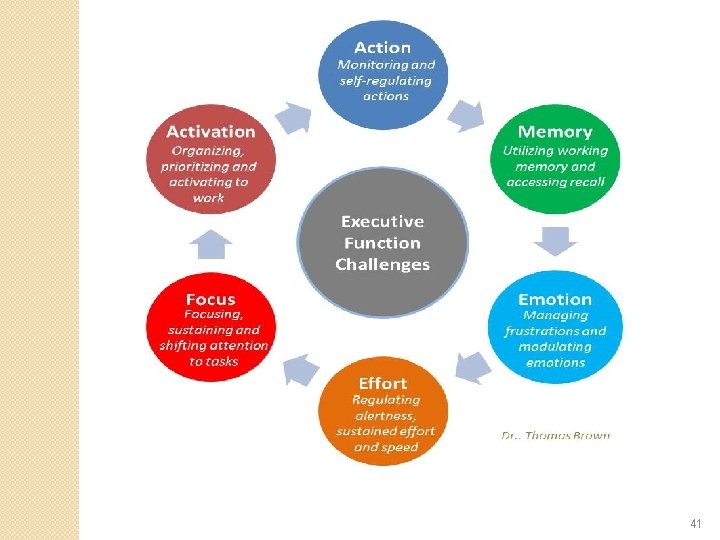
Understanding How We Develop Emotional Regulation is one component in our development. � Our next regulatory system involved in our development is… � Executive Functioning 38
Executive Functioning https: //www. youtube. com/watch? v=q. UIr. Wmwg 4 Kg 39
40
41
Understanding How We Develop �Emotional strengths and weaknesses… �Cognitive strengths and weaknesses… Are unique to every individual �In addition to these developmental factors, we also have Trauma and Mental Health to consider. 42
43 MODULE 3 TRAUMA (Preset)
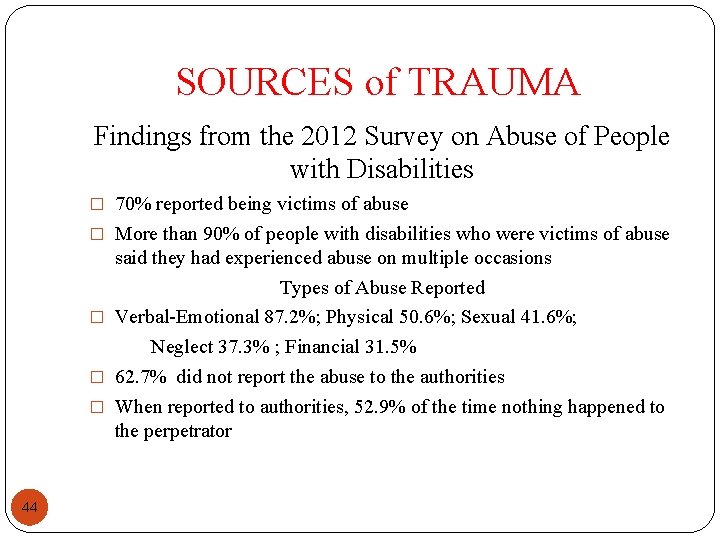
SOURCES of TRAUMA Findings from the 2012 Survey on Abuse of People with Disabilities � 70% reported being victims of abuse � More than 90% of people with disabilities who were victims of abuse said they had experienced abuse on multiple occasions Types of Abuse Reported � Verbal-Emotional 87. 2%; Physical 50. 6%; Sexual 41. 6%; Neglect 37. 3% ; Financial 31. 5% � 62. 7% did not report the abuse to the authorities � When reported to authorities, 52. 9% of the time nothing happened to the perpetrator 44
TRAUMA �People with developmental disabilities suffer 2. 5 to 10 times the abuse and neglect of non-disabled peers. �More than 90% of adults reported sexual abuse within their lifetime. Jacobstein, 2015 All of these facts are significant in the often forgotten development of trauma with those we support. 45
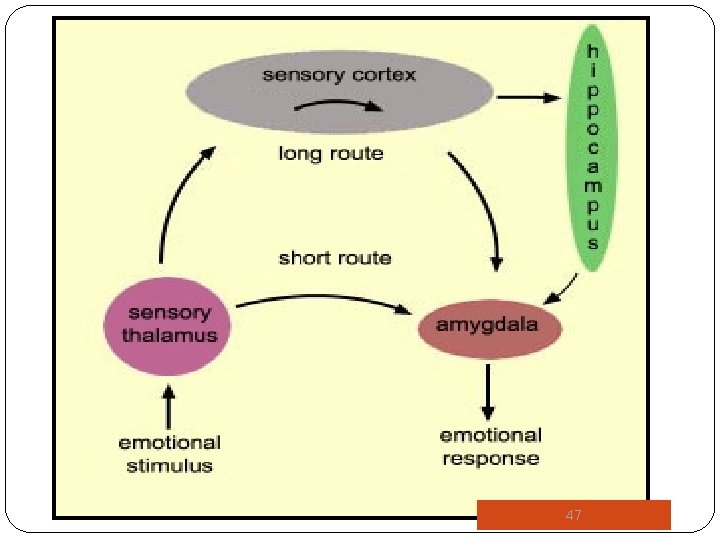
TRAUMA �The brain does not differentiate between physical, emotional, or observatory trauma. All are interpreted by the brain as trauma. (Palay, 2013) �Trauma in childhood can permanently alter neuron response and cognitive pathways in the brain. �Trauma may be associated with abnormal activation of the amygdala, abnormal levels of cortisol, epinephrine, and norepinephrine, and structural changes to the hippocampus. 46
47
TRAUMA �As we know, all of these brain structures and neurochemicals play key roles in regulating our emotional, behavioral, physical, and mental health. �Individuals who have experienced trauma within their lives may respond in one of two ways when a perceived threat presents itself: 48 v Disassociation- detached, numb, compliant, mini-psychoses v Hyperarousal- anxious, reactive, alarm response, hypervigilant
TRAUMA �The impact of different traumatic events is not independent of each other; in other words, the events build upon one another, and the stress from the trauma becomes cumulative. �The ability to process traumatic experiences decreases with repeated exposure. This decrease may then express itself through behavioral or mental health disorders. 49
Module 4 Mental Health Disorder (Preset) 50
A Few Mental Health Disorders First, we must recognize that it is possible for an individual with intellectual/developmental disability to • Display a challenging behavior, such as aggression, in the absence of a mental health disorder; • Display a diagnosable mental health disorder in the absence of any significant challenging behavior; and, • Have a mental health disorder and a challenging behavior coexist and exert mutual influence over each other. (Allen, 2008) 51
Mental Health • There is a belief that individuals with Intellectual Developmental Disabilities (I/DD) cannot have a co-occurring mental health disorder. • Individuals with I/DD may suffer the full range of mental health disorders similar to the general population. • Fact: 30 -35% of individuals with I/DD have a psychiatric disorder (NADD, 2013). 52
Mental Health • Research suggests that 10 -20% have challenging behaviors (aggression, self-injury, destructive behavior) that interferes with their Quality of Life. • The inter-relationship between mental health disorders and challenging behavior is complex and is complicated by one’s communication abilities. • The complexity, however, does not suggest that all challenging behaviors are a result of an undiagnosed mental health disorder. 53
Mental Health Treating challenging behavioral symptoms from a mental health disorder requires and integrated approach involving treatments which may be written in a PBIS plan, such as … • Interventions such as increasing alternative skills (deep breathing exercises, recognizing the specific emotions); environmental restructuring; social stories. • Counseling • Accurate and meaningful behavior data of the behavioral symptoms associated with the mental health disorder • Person-Centered, strategies specific to the person 54
A Few Mental Health Disorders Five common mental health disorders with possible behavioral factors associated with them: • Reactive Attachment Disorder • Posttraumatic Stress Disorder • Depression • Anxiety Disorders • Neurocognitive Disorder-Dementia 55
Reactive Attachment Disorder A clinical syndrome characterized by a severe disruption in the development and expression of emotional attachments. The diagnostic criteria for age of onset is before the age of five (5). (DM-ID) 56
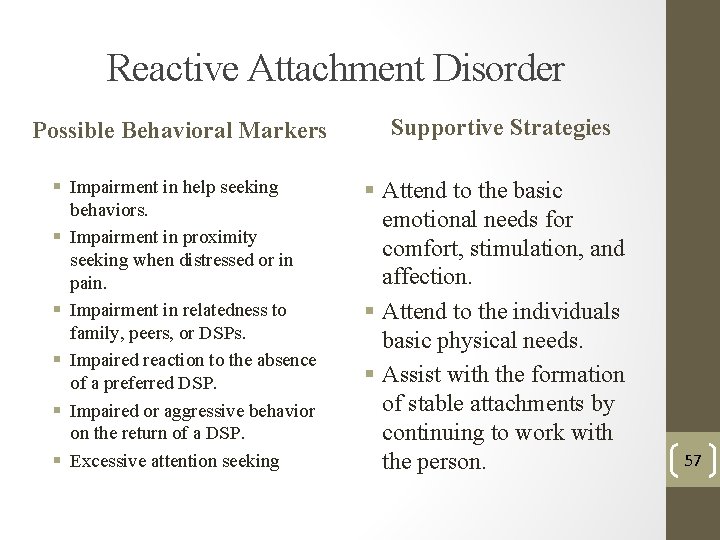
Reactive Attachment Disorder Possible Behavioral Markers § Impairment in help seeking behaviors. § Impairment in proximity seeking when distressed or in pain. § Impairment in relatedness to family, peers, or DSPs. § Impaired reaction to the absence of a preferred DSP. § Impaired or aggressive behavior on the return of a DSP. § Excessive attention seeking Supportive Strategies § Attend to the basic emotional needs for comfort, stimulation, and affection. § Attend to the individuals basic physical needs. § Assist with the formation of stable attachments by continuing to work with the person. 57
Posttraumatic Stress Disorder (PTSD) is considered to be a chronic anxiety disorder. It is often cyclic and progressive. The traumatic event can compromise functioning at every level; biological, psychological, social, and spiritual. (DM-ID) 58
Posttraumatic Stress Disorder Possible Behavioral Markers § Fear § Helplessness § Behavioral acting out of traumatic experiences § Recurrent distress § Frightening dreams § Avoidance of activities § Difficulty falling or staying asleep § Irritability or outbursts of anger Supportive Strategies § Avoid wearing scents that may trigger an emotional memory. § Be aware your tone of voice when speaking. Confrontational tones often trigger emotional responses. § Ensure the environment feels safe to the person. 59
DEPRESSION 60
Depressive Disorder • Natural losses, such as death of a family member or a family moving away may be experienced more deeply for someone diagnosed with I/DD than the general population. • Individuals with I/DD have many more experiences outside of their “external locus of control” such as making decisions, or what activities they may participate in either through guardianship or through structure and supervision. 61
Depressive Disorder The prevalence of depression among adults with intellectual/developmental disability is estimated to be 2. 2% (Deb, Thomas, and Bright, 2001) 62
Depressive Disorder Presentation in Someone with I/DD • • Frequent unexplained crying Decrease in laughter and smiling General irritability and subsequent aggression or self-injury Sad facial expression No longer participates in favorite activities Reinforcers no longer valued Increased time spent alone Refusals of most work/social activities 63
Depressive Disorder Presentation in Someone with I/DD • • • Measured weight changes Increased refusals to come to table to eat Unusually disruptive at meal times Constant food seeking behaviors Disruptive at bed time Repeatedly gets up at night Difficulty falling asleep No longer gets up for work/activities Early morning awakening Over 12 hours of sleep per day Naps frequently 64
Depressive Disorder Supportive Strategies • Recognize the gradual decrease in the person’s overall demeanor or interest in activities as a possible disorder. It may not just be “who they are”. • Assist the person to increase their quality of life by engaging in activities. Exercise (even walking) can help with symptoms of depression. • Support the person to keep a healthy routine. 65
Anxiety Disorders 66
Anxiety Disorders • The prevalence of anxiety disorders in children with I/DD is 11. 4 -39% (Oeseburg et al. , 2011). • The adult prevalence is 2 -17%. Adults with no day program or a history of recent life events were more likely to have anxiety disorder (Reid, Smiley, & Cooper, 2011). • Anxiety Disorders and Autism Spectrum Disorder often co-occur (Buck et al. , 2014). 67
Anxiety Disorders include a large number of conditions characterized by: • Sense of apprehension • Physiological symptoms – sweating, increased heart rate, increased rate of respiration • Restlessness, fatigue, irritability, sleep disturbances, difficulty concentrating, muscle tension, personality changes. • Lack of cause or situation does not warrant the extent of the reaction. 68
Anxiety Disorders • Accumulation of life events, especially negative ones results in higher frequency of depressive and anxiety symptoms. • The following life events were most often perceived as negative. • Change in DSPs • Minor illness or injury • Problems with housemate • People with mild or moderate ID experience more total life events than those with severe or profound ID. (Hermans & Evenhuis, 2012) 69
Anxiety (General) Possible Behavioral Markers § Difficulty in managing the worrying § Restlessness § On edge § Difficulty concentrating § Irritability § Sleep disturbance § Physically ill from worrying § Tense Supportive Strategies § Build a rapport with the person prior to providing personal hygiene care. § Provide structure and consistency. § Explain transitions from one event to the other. § Provide reassurance during new activities. 70
Dementia 71
Dementia is a general (umbrella) term for: v A decline from baseline in cognitive ability, and v That is severe enough to interfere with daily functioning (Sanderson, 2013) There is disturbance of multiple higher cortical functions, including memory, thinking, orientation, comprehension, learning, and judgment. Impairments of cognitive function are commonly accompanied, and occasionally preceded by deterioration in emotional control, social behavioral, or motivation. (DM-ID) 72
Dementia Possible Behavioral Markers § Change in level of care for ADLs § Excessive sleep § Appear confused with simple tasks § Confusion worsens at night § Wakes earlier than usual § Begins needing assistance with eating § Begins not recognizing familiar people Supportive Strategies § Remember the person may seem confrontational or refuse to complete a task because they are unable. § Recognize and report the signs/symptoms of the behavioral markers to a doctor. § Recognize the difference between other Mental Health Disorders and Dementia. 73
74 WHAT ABOUT…
75 AUTISM SPECTRUM DISORDER (PRESET)
76 Autism is a very broad spectrum and diagnosis is not precise. It is a behavioral profile. (Grandin, 2014) Although there are no general known causes, it is believed to be a neurobiological disorder. In addition, current research is finding some genetic commonalities. (Grandin, 2014)
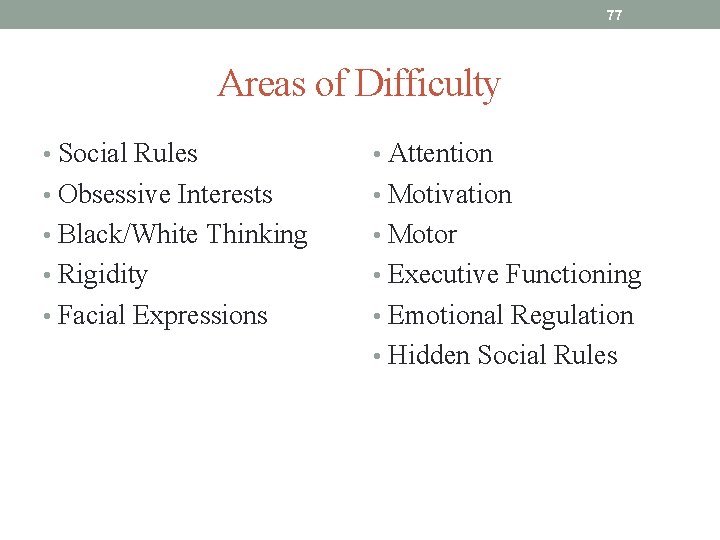
77 Areas of Difficulty • Social Rules • Attention • Obsessive Interests • Motivation • Black/White Thinking • Motor • Rigidity • Executive Functioning • Facial Expressions • Emotional Regulation • Hidden Social Rules
78 Sensory Processing Difficulties • Each of us have various sensory systems which process information and assist us in making sense of the world. • People with autism spectrum disorders have difficulty processing and using sensory input in a meaningful and relevant way. • Some individuals are over sensitive and others are under sensitive to sensory input.
79 Common Stressors at Home • Sensory • Completing routines • food • getting ready for school • haircuts • doing homework • dentists • chores • medical • clothing • showers • Family activities • Adjusting “their” agenda/interests with family plans
Module 5 The Biopsychosocial Approach to Our Behavior 80
The Biopsychosocial Approach • The biopsychosocial approach acknowledges the complexity of underlying determinants that may contribute to a challenging behavior. • It draws attention from previous approaches that have been used to explain challenging behavior (that is, medical condition, health problems, behavioral phenotypes, and mental health disorders). • It recognizes the individual is part of a broader system that includes the person and their community. (Koritsas and Lacono, 2012) 81
The Biopsychosocial Approach • This approach encourages consideration of these systems when as they are the “presets” to possible challenging behavior: Ø Biological (that is, physical health/ill health and mental health disorders) Ø Psychological (that is, learning, coping, thoughts) Ø Sociological (that is, environments and relationships) 82 (Engel, 1979)
The Biopsychosocial Approach Biological (Ill Health) Ø Fatal Four (Aspiration, Dehydration, Constipation, Seizure) Ø Weight Management Ø Diabetes Ø Tooth pain Ø Heart conditions Ø Medication side-effects (headaches, nausea, dizziness, agitation, etc. ) Ø Allergies Ø Skeletal maladies Ø Artificial skeletal supports/replacements Ø Muscle or joint pain Ø Menses 83
The Biopsychosocial Approach • Biological- Mental Health Disorders Ø Post Traumatic Stress Disorder Ø Depression Ø Anxiety Ø Bipolar Disorder Ø OCD Ø ADHD Ø Sleep Disorders Ø Pica Ø Dementia 84
The Biopsychosocial Approach Psychological • • • Emotional turmoil Negative thinking Rejection by others Loneliness Uncertainty Fearful 85
The Biopsychosocial Approach • Sociological � Relationships Ø Living Environment Ø Family Ø Friends Ø Community � Community Inclusion Ø Clubs Ø Sports Ø Volunteer organizations Ø Favorite activities 86
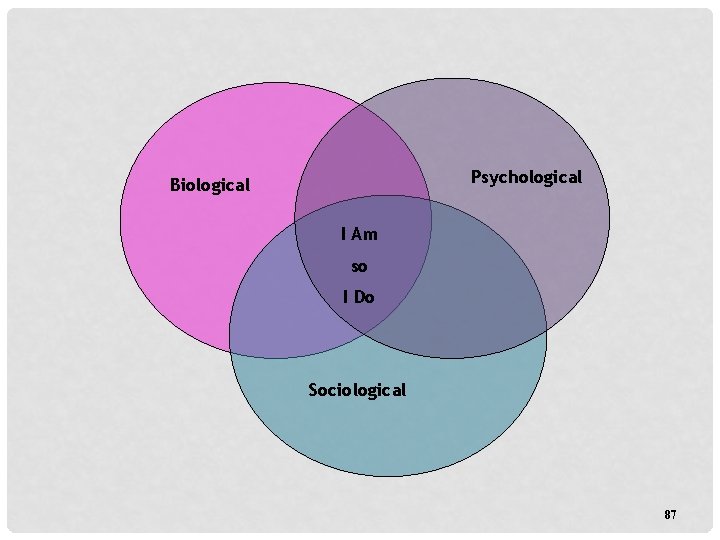
Psychological Biological I Am so I Do Sociological 87
Module 6 Positive Behavior Intervention Support Basic Behavior Management 88
Levels of Supervision • Routine • Close • Constant 89
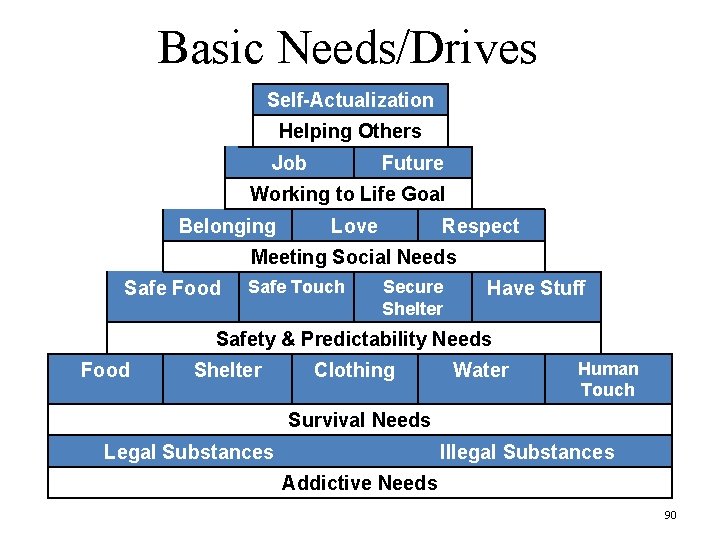
Basic Needs/Drives Self-Actualization Helping Others Job Future Working to Life Goal Belonging Love Respect Meeting Social Needs Safe Food Safe Touch Secure Shelter Have Stuff Safety & Predictability Needs Food Shelter Clothing Water Human Touch Survival Needs Legal Substances Illegal Substances Addictive Needs 90
Environment • The environment has a substantial impact on behavior. • Assessing how we can modify the environment may have an immediate and positive effect on behavior. 91
Appearance and Dress • • • How do we dress? Safe, modest & comfortable Leave items home if they interfere What does grooming say about us? Awareness of our scents & smells Individual considerations 92
Routines and Rhythms § Having routines and rhythms of our day, week, month, and year is an important aspect of environment. § Routines and rhythms can decrease anxiety and stress. § Everyone relies on routines to a certain degree. Routine activities and rhythm enable us to function effectively and comfortably. § Exercise: Now let’s examine your routine 93
Presets to Challenging Behavior Our first response to a challenging behavior is to remember the presets involved with the person. Presets are the biological, psychological, and sociological conditions that affect the person. These presets are the internal events for the person that, at times, may not be well managed. 94
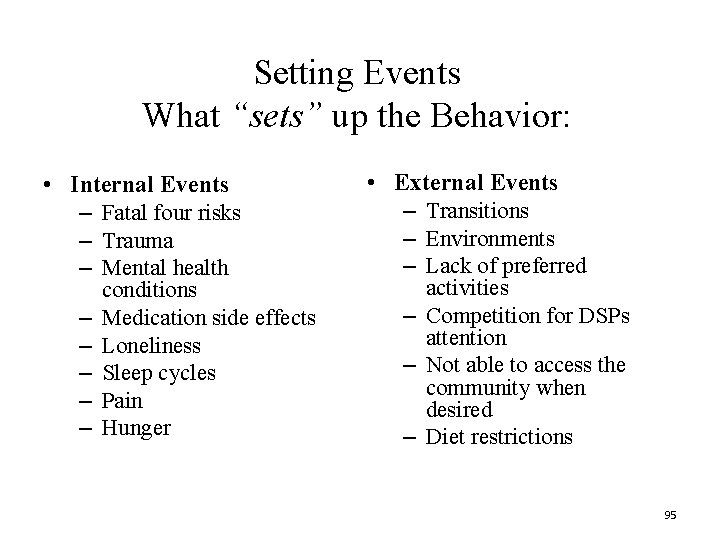
Setting Events What “sets” up the Behavior: • Internal Events – Fatal four risks – Trauma – Mental health – – – conditions Medication side effects Loneliness Sleep cycles Pain Hunger • External Events – Transitions – Environments – Lack of preferred activities – Competition for DSPs attention – Not able to access the community when desired – Diet restrictions 95
Setting Events Choices • People with intellectual disabilities often have limited choices. • A lack of choice diminishes one’s sense of control and dignity. • It is important that we think about where we can provide choice in people’s lives. Class activity 96
Antecedents • Any noticeable event that happens immediately before the particular behavior. • Antecedents are behavioral “Cues” • Antecedents are the “triggers” of the behavioral chain 97
Behavior What is a Challenging Behavior? “A behavior can be describe as challenging when it is of such an intensity, severity, frequency, and duration as to threaten the Quality of Life and/or the physical safety of the individual or others; AND is likely to lead to responses that are restrictive, aversive or result in exclusion” (Emerson, 2001) 98
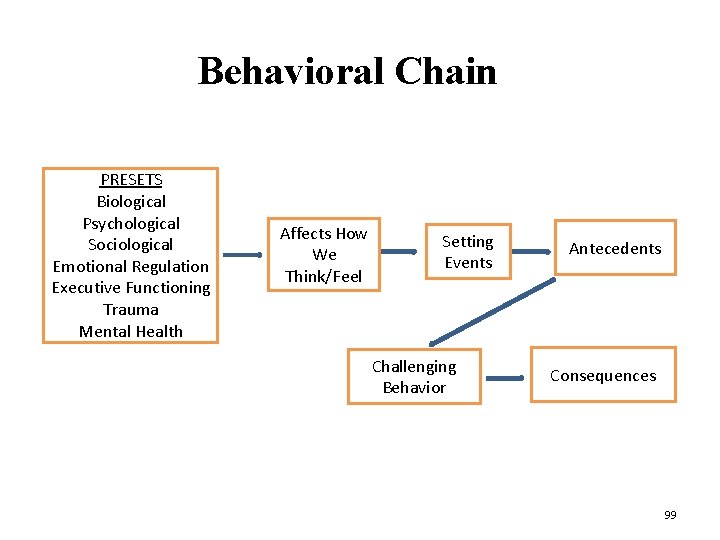
Behavioral Chain PRESETS Biological Psychological Sociological Emotional Regulation Executive Functioning Trauma Mental Health Affects How We Think/Feel Setting Events Challenging Behavior Antecedents Consequences 99
It’s important to find a replacement behavior that meets the same needs for the individual in a more acceptable or appropriate way. If YOU can’t think of an alternative to difficult behaviors, chances are good the person will have trouble learning one! -David Pitonyak 100
Consequences What happens immediately after the behavior occurs (what the person gets or avoids as a result of the behavior). There are 2 kinds of Consequences: 1. Reinforcers: increase the likelihood of behavior happening again 2. Punishers: decrease the likelihood of behavior happening again (in theory) 101
Reinforcement • Purpose – Building positive relationships – Creates positive, inviting environments – Encourages desired behaviors • Starts new behaviors (rookies) • Maintains mastered behaviors (veterans) 102
Reinforcement • Reinforcement must meet the same function as the problem OR is larger and more reinforcing than the function of challenging behavior. 103
Reinforcement Positive Reinforcement: The addition of something pleasant* Negative Reinforcement: The removal of something unpleasant* *Note: Based on individual’s perception of what is pleasant/unpleasant 104
Reinforcement https: //www. youtube. com/watch? v=imkbu. Kom. P XI 105
Behavior Management 101 Reinforcement is the best practice and most effective way to alter challenging behavior Utilizing punishment is the least effective. 106
Punishment • The application of punishment (in theory) reduces the chances of a particular behavior’s reoccurrence. • By this definition, punishment will reduce problem behavior. But at a cost. . . 107
Punishment • Effective in the presence of the punisher. Increase covertness. • Requires greater resources to be effective. Increasing severity, constant vigilance • Produces unintended consequences: Damages relationships, anger & aggression, changes worldview. • You get more of what you pay attention to! 108
Punishment • If the behavior continues to occur, then it is not working to decrease the behavior. • Often times we think punishment is the only way to reduce problem behavior but after looking at the actual result it may reinforce the behavior (by definition). 109

Punishment N ME SH NI PU T 110
MODULE 7 Models For Approaching Challenging Behavior v Relationship Model v Trauma Model v Quality of Life Model 111
Relationships (or lack of) “Loneliness may be the number one cause of challenging behavior. ” -David Pitonyak 112
Relationships • Many of the people we support have few relationships outside of family or paid providers. • Often this lack of true friendships causes unhappiness which sometimes manifests itself as “challenging behaviors”. 113
Relationships: Class Exercise Family Work Self Home 114 Friends
RELATIONSHIPS • https: //www. youtube. com/watch? v=sc 5 rz. CGK 20 115
Building Rapport • • • Individuals who do not feel a connection with those who support them are less likely to trust and work willing with the DSP/PSW. Building rapport is especially important for individuals who have experienced multiple disruptions in relationships. It can show individuals they can trust relationships after repeated experiences of loss. 116
Building Rapport • Ways to build rapport • Begin your relationship by getting to know the person, not jumping into the personal care part of your job immediately. • Relate to the individual through hobbies and interests. • Be interested in the individuals hobbies and interests even if you don’t share the same passion. • Understand that you can also learn from the individual, this should be a mutual relationship. 117
Enhance Community Friendships and Relationships • Expand connections within the community allows for opportunities to make friendships. • Teach and practice social skills when in the community. Encourage individuals to be respectful with fellow community members. • Model respectful behavior with others. • Engage the individual in community activities that includes their interests and hobbies. 118
“If you get relationships right. . . everything else will fall into place. -D. Pitonyak 119
Trauma Model “Trauma is any experience or series of experiences that make the individual feel that he or she is in danger of dying, or of being emotionally ‘wiped out’ or annihilated. ” (Palay, 2013) 120
TRAUMA MODEL 121 https: //vimeo. com/100518405
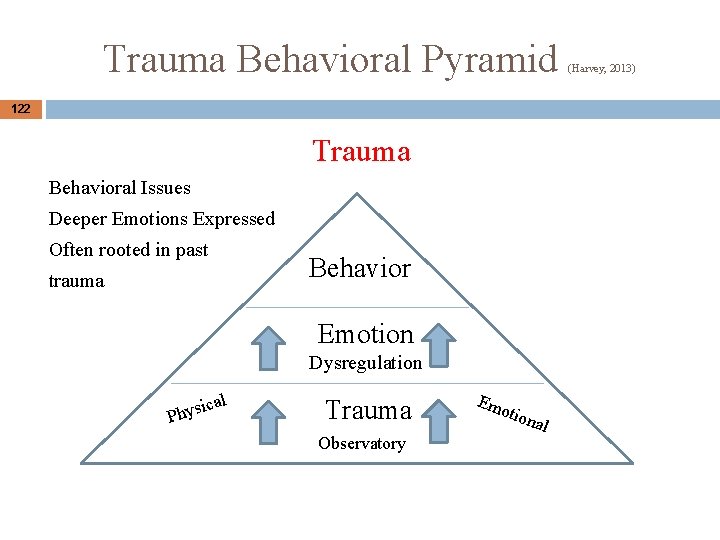
Trauma Behavioral Pyramid 122 Trauma Behavioral Issues Deeper Emotions Expressed Often rooted in past Behavior trauma Emotion Dysregulation al ic Phys Trauma Observatory Em otio nal (Harvey, 2013)
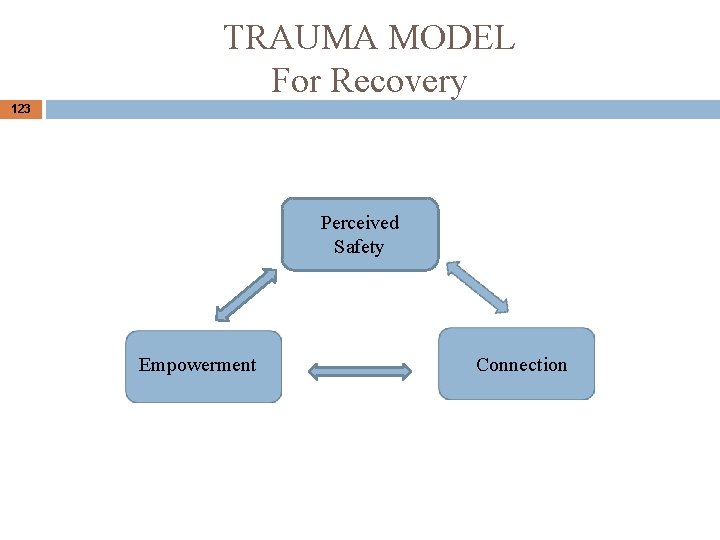
TRAUMA MODEL For Recovery 123 Perceived Safety Empowerment Connection
124 Quality of Life Model
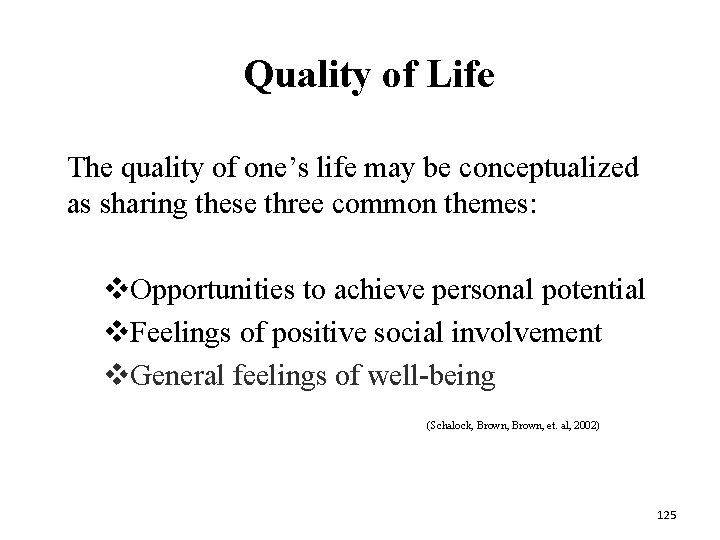
Quality of Life The quality of one’s life may be conceptualized as sharing these three common themes: v. Opportunities to achieve personal potential v. Feelings of positive social involvement v. General feelings of well-being (Schalock, Brown, et. al, 2002) 125
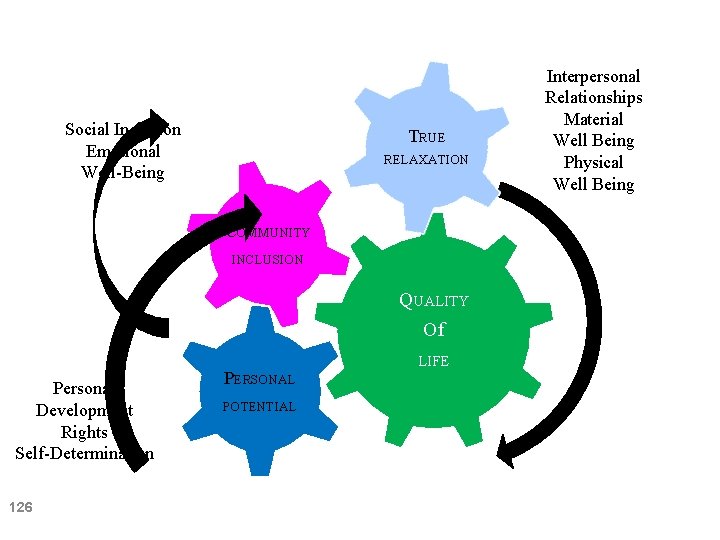
Social Inclusion Emotional Well-Being TRUE RELAXATION COMMUNITY INCLUSION QUALITY Of Personal Development Rights Self-Determination 126 PERSONAL POTENTIAL LIFE Interpersonal Relationships Material Well Being Physical Well Being
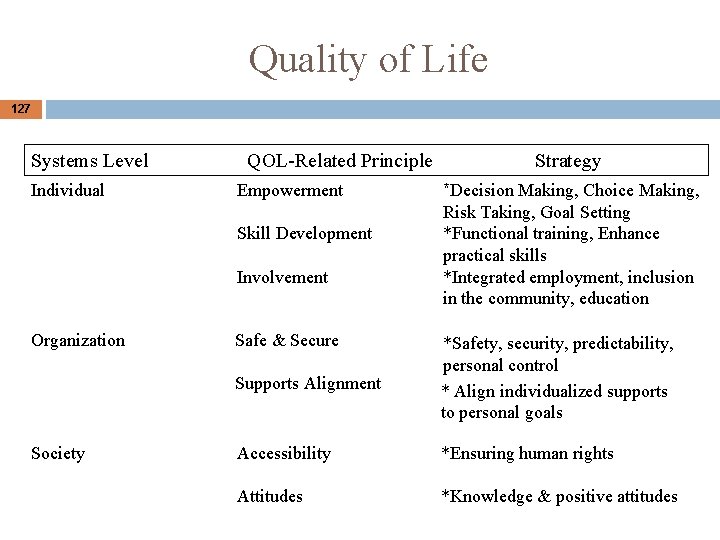
Quality of Life 127 Systems Level Individual QOL-Related Principle Empowerment Skill Development Involvement Organization Society Safe & Secure Strategy *Decision Making, Choice Making, Risk Taking, Goal Setting *Functional training, Enhance practical skills *Integrated employment, inclusion in the community, education Supports Alignment *Safety, security, predictability, personal control * Align individualized supports to personal goals Accessibility *Ensuring human rights Attitudes *Knowledge & positive attitudes
128 MODULE 8 COMMUNICATION & POWER STRUGGLES Elements of communication Communication problems
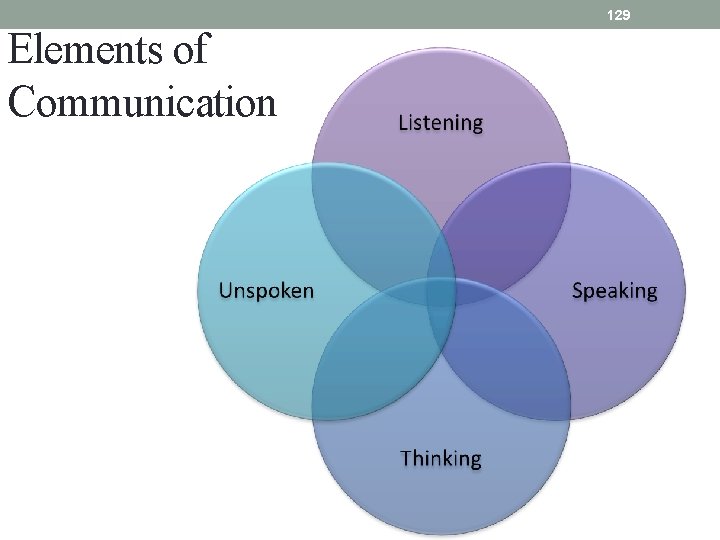
129 Elements of Communication
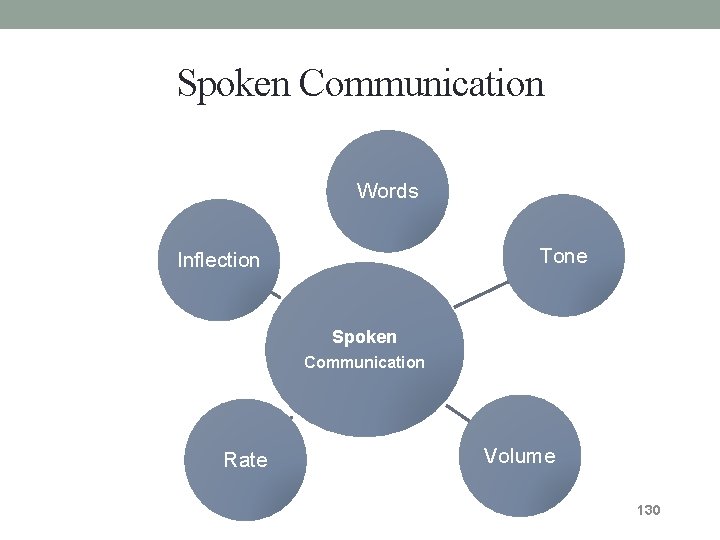
Spoken Communication Words Tone Inflection Spoken Communication Rate Volume 130
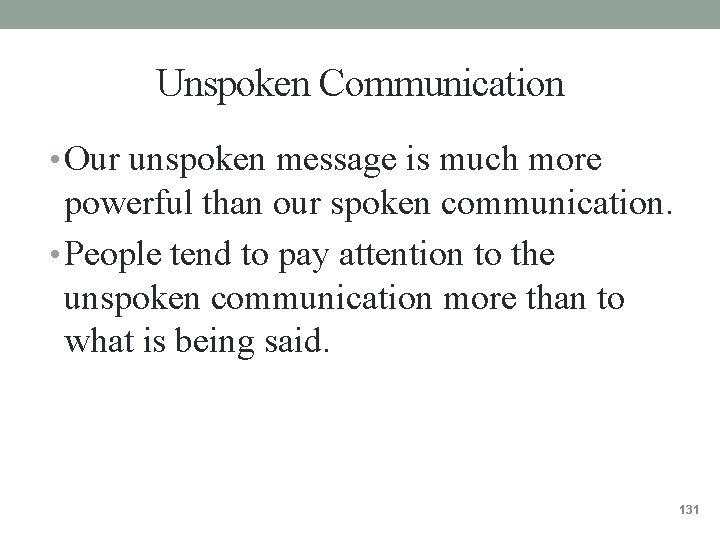
Unspoken Communication • Our unspoken message is much more powerful than our spoken communication. • People tend to pay attention to the unspoken communication more than to what is being said. 131
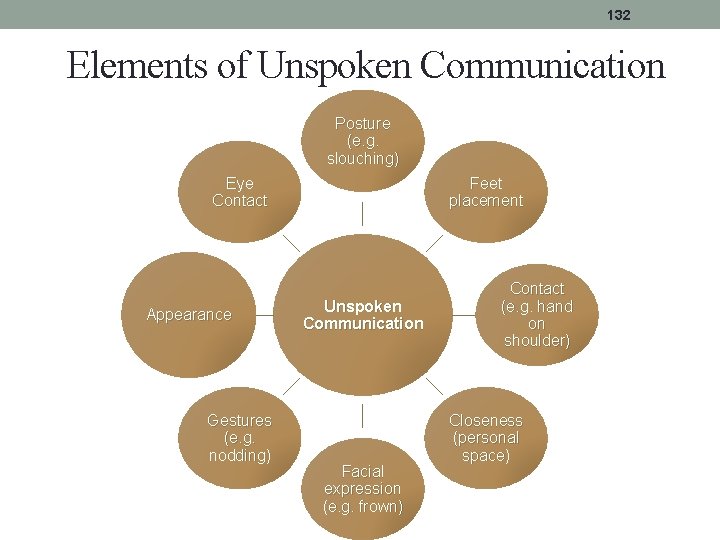
132 Elements of Unspoken Communication Posture (e. g. slouching) Eye Contact Appearance Gestures (e. g. nodding) Feet placement Unspoken Communication Facial expression (e. g. frown) Contact (e. g. hand on shoulder) Closeness (personal space)
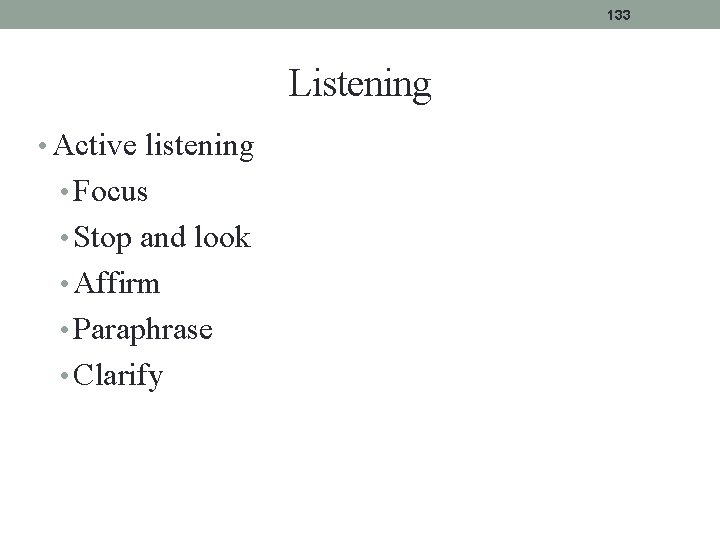
133 Listening • Active listening • Focus • Stop and look • Affirm • Paraphrase • Clarify
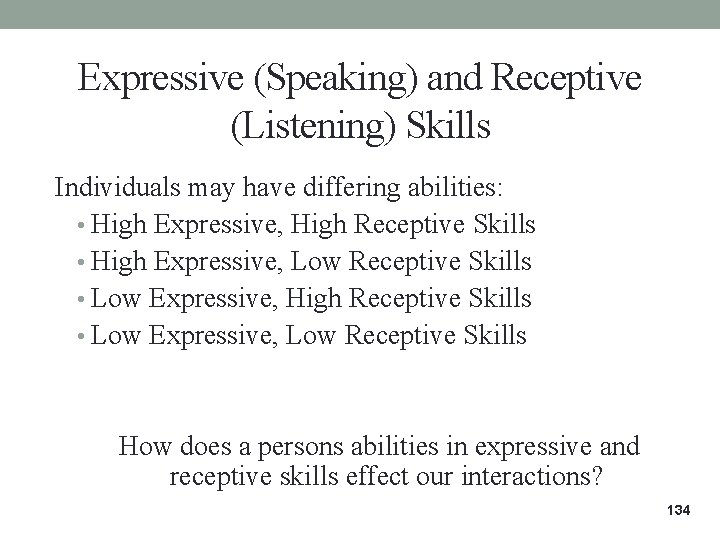
Expressive (Speaking) and Receptive (Listening) Skills Individuals may have differing abilities: • High Expressive, High Receptive Skills • High Expressive, Low Receptive Skills • Low Expressive, High Receptive Skills • Low Expressive, Low Receptive Skills How does a persons abilities in expressive and receptive skills effect our interactions? 134
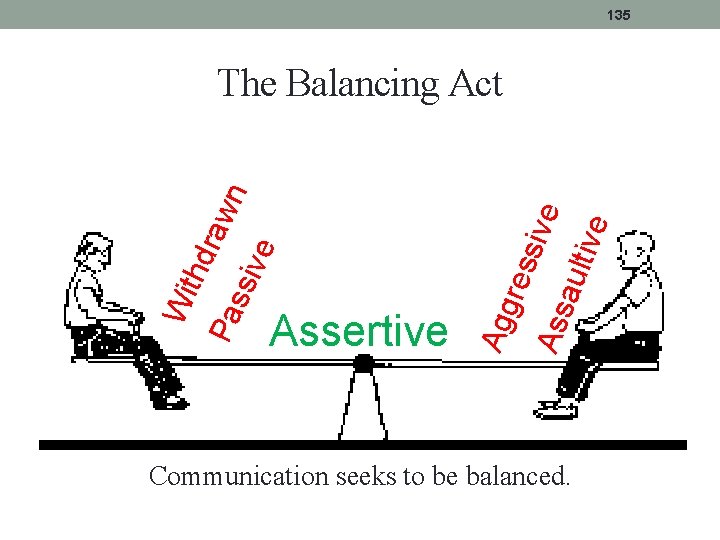
135 ive ault sive res Assertive Agg ve ssi Pa Wi thd raw n The Balancing Act Communication seeks to be balanced.
136 Assertive Communication • Uses Objectivity • Creates Ownership • Makes Clear, Direct Requests
137 Assertive Communication “I” messages are crucial to effective assertive communication. “I understand _____ (empathy/validation)” “I feel or I see _____ (state the problem)” “I want _____ (state what I want)”
138 Common Communication Problems • Misinterpretation • Differing Perspective • Misinterpreted Motives • Failure to actually listen • Using Inflammatory Statements
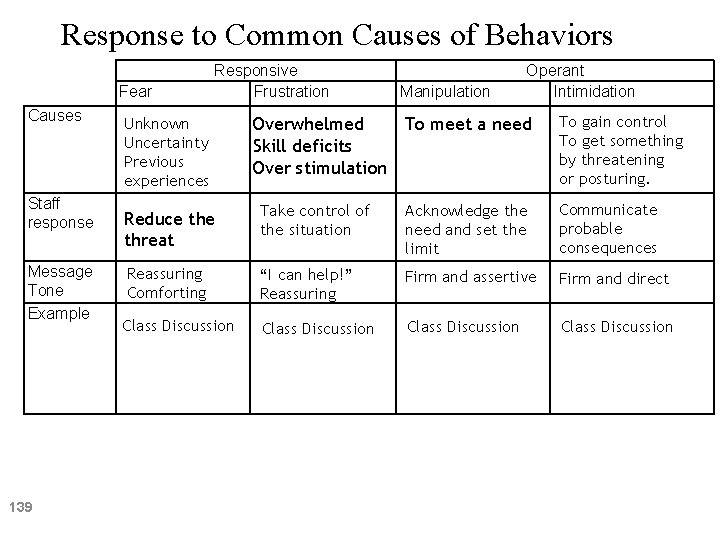
Response to Common Causes of Behaviors Fear Causes Staff response Message Tone Example 139 Responsive Frustration Unknown Uncertainty Previous experiences Manipulation Operant Intimidation To meet a need Overwhelmed Skill deficits Over stimulation To gain control To get something by threatening or posturing. Reduce threat Take control of the situation Acknowledge the need and set the limit Communicate probable consequences Reassuring Comforting “I can help!” Reassuring Firm and assertive Firm and direct Class Discussion
140 Power Struggles • Power Struggles are when two or more people are attempting to have power over one another. • A consumer wants to leave the store without paying for their soda. You try to make the person pay or try to keep them from leaving. • A consumer doesn’t want to do the assigned chore. You try to force them by an, “or else. . . ” statement.
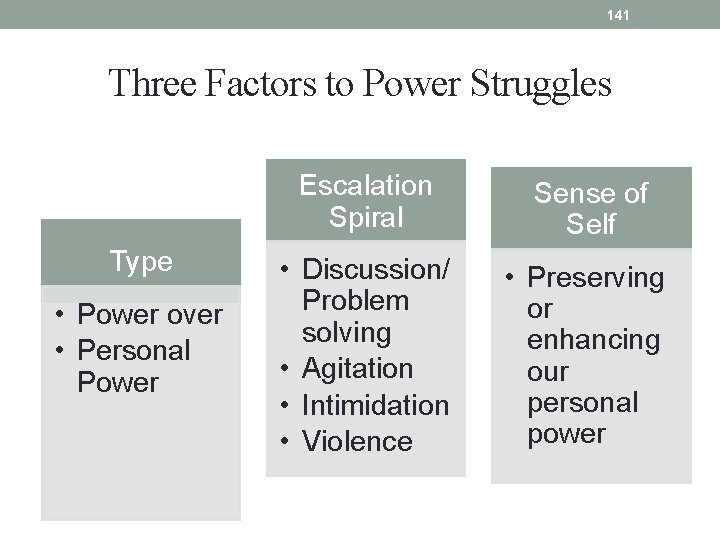
141 Three Factors to Power Struggles Type • Power over • Personal Power Escalation Spiral Sense of Self • Discussion/ Problem solving • Agitation • Intimidation • Violence • Preserving or enhancing our personal power
142 Who Engages in Power Struggles? Anyone! Everyone engages in a power struggle at some point. • However, the following staff tend to engage in power struggles most often: • “Perfectionists” • Those with “unrealistic expectations” • “Inexperienced” staff •
143 Behaviors that may Contribute to Power Struggles • Arguing • Demanding • Being disrespectful (based upon the person’s perception) • Being inflexible
144 Minimizing the Power Struggle • Choose your battles • Walk away • Consider the volume of your voice • Set limits, avoid ultimatums • Keep your cool
145 Resolving Power Struggles • Power struggles tend to escalate as they cause both parties to become stressed. • It is not always easy to stop the escalation • Recognizing that you are in a power struggle is the first step. • Then, you must choose a resolution strategy: Power-based, rights-based, or interest-based.
146 De-escalation Tool: Silence • Remaining silent can be powerful. 1. It allows for time to listen to the escalated person and assess the situation. 2. Silence does not add fuel to the fire. If there is nothing to argue with, then the power struggle does not exist. As with any tool, this may not work in all situations. Your continual assessment of the situation will help you decide if it is working.
147 MODULE 9 STRESS AND SELF-CONTROL
Stress Management 148 • • • This profession is stressful! It is important to proactively and reactively manage your stress. Our support of the consumer is limited by our stress level. Stress can be managed with activities that require physical and mental energy. Physical exercise Gardening Journaling Meditating Deep Breathing
Stress 149 A feeling that’s created when we react to particular events that have a high probability to affect our lives. It’s the body’s way of rising to the challenge and preparing to meet a tough situation with focus, strength, stamina and heightened alertness.
Stress Response 150 Our brains assess a threat in terms of whether or not we can handle it. We can’t always differentiate between real and perceived threats. You don’t have to be directly involved in the event to experience stress.
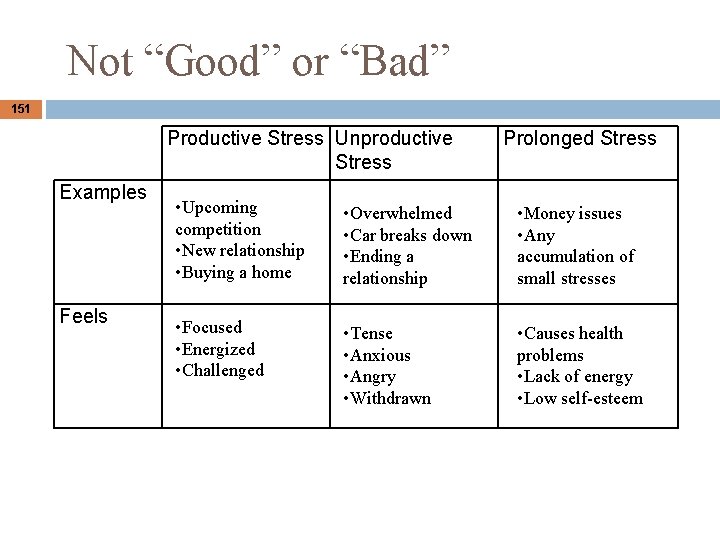
Not “Good” or “Bad” 151 Productive Stress Unproductive Stress Examples Feels Prolonged Stress • Upcoming competition • New relationship • Buying a home • Overwhelmed • Car breaks down • Ending a relationship • Money issues • Any accumulation of small stresses • Focused • Energized • Challenged • Tense • Anxious • Angry • Withdrawn • Causes health problems • Lack of energy • Low self-esteem
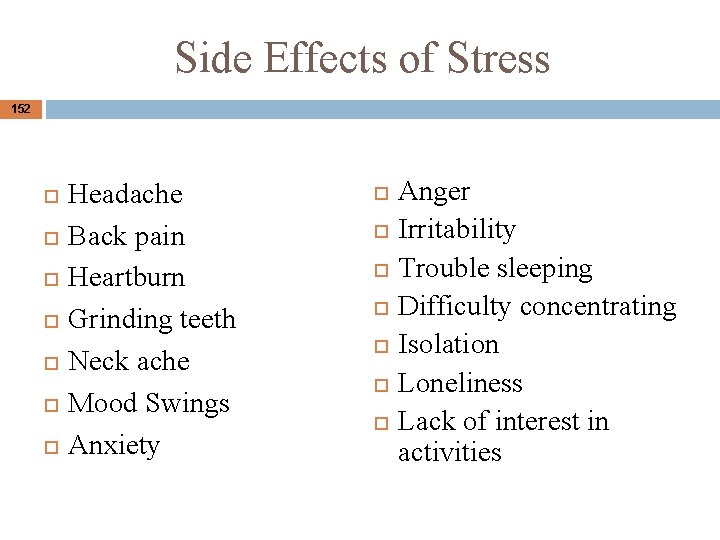
Side Effects of Stress 152 Headache Back pain Heartburn Grinding teeth Neck ache Mood Swings Anxiety Anger Irritability Trouble sleeping Difficulty concentrating Isolation Loneliness Lack of interest in activities
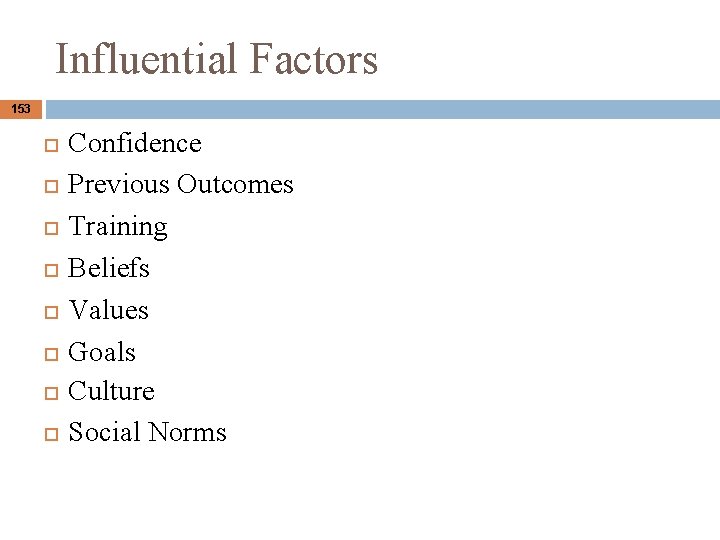
Influential Factors 153 Confidence Previous Outcomes Training Beliefs Values Goals Culture Social Norms
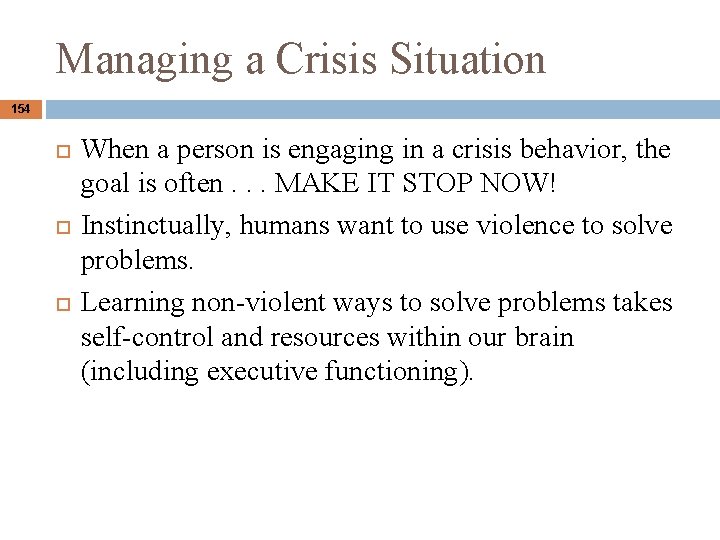
Managing a Crisis Situation 154 When a person is engaging in a crisis behavior, the goal is often. . . MAKE IT STOP NOW! Instinctually, humans want to use violence to solve problems. Learning non-violent ways to solve problems takes self-control and resources within our brain (including executive functioning).
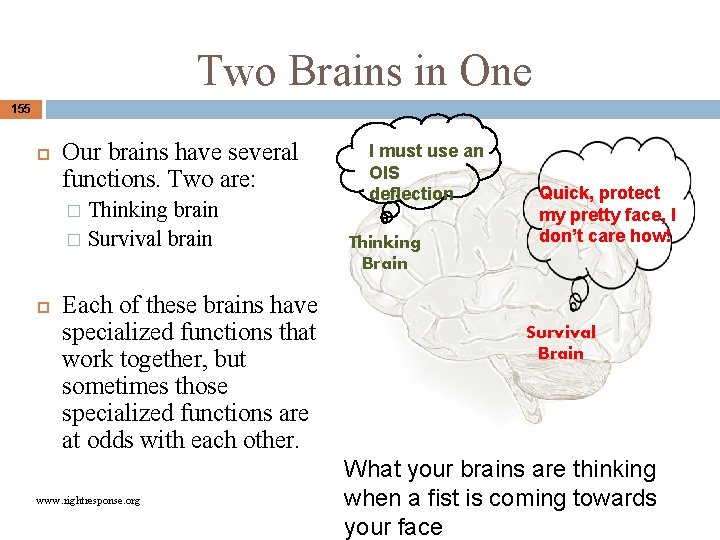
Two Brains in One 155 Our brains have several functions. Two are: Thinking brain � Survival brain � Each of these brains have specialized functions that work together, but sometimes those specialized functions are at odds with each other. www. rightresponse. org I must use an OIS deflection Thinking Brain Quick, protect my pretty face, I don’t care how! Survival Brain What your brains are thinking when a fist is coming towards your face
Alarm Reaction 156 An alarm reaction occurs when your safety is threatened. This causes your survival brain to take charge, shutting down your thinking brain. Alarm reactions are NOT useful when responding to a challenging issue!
Alarm Reaction Process 157 • • • Everyone freezes at the first sight of danger. Most of us progress to flight or fight. Some people get stuck in freeze or progress to freeze when hope of survival is diminished. All of these responses shut down the thinking brain.
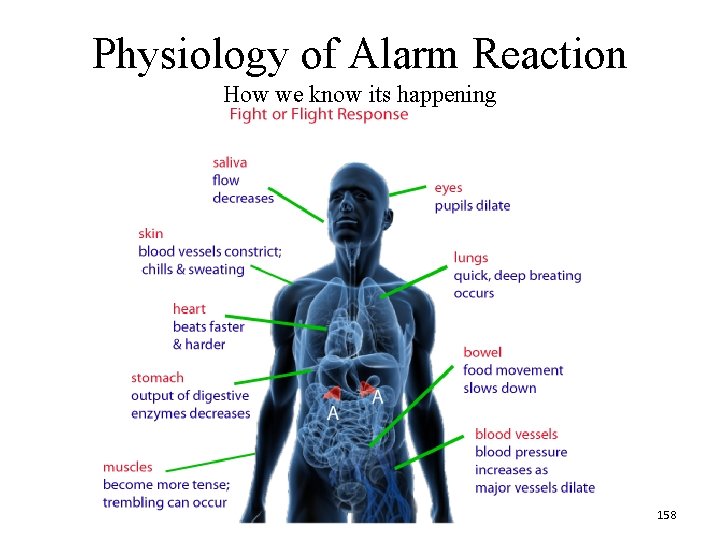
Physiology of Alarm Reaction How we know its happening 158
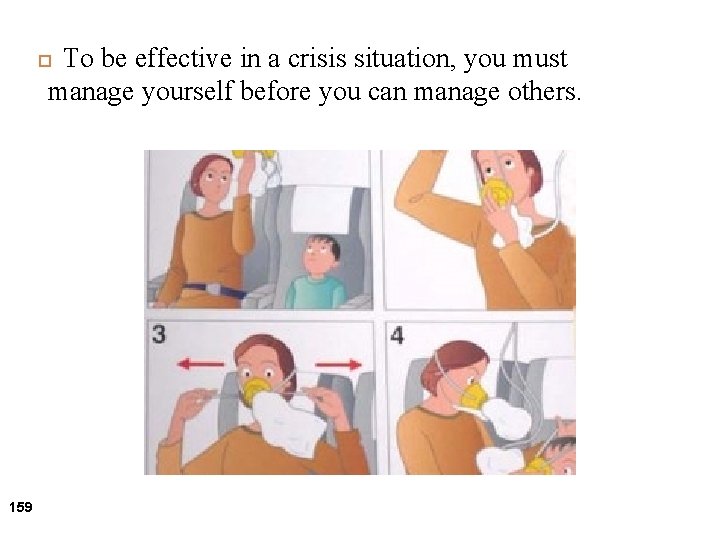
To be effective in a crisis situation, you must manage yourself before you can manage others. 159
Shut down the Alarm Reaction 160 When anyone is faced with a threatening situation, your brain wants to respond with an This when you need to protect the person who is threatening you. Instead, you must Maintain Self-Control.
Developing a Self-Control Plan 161 Mandatory Individual Exercise: � Identify what you may do if the alarm reaction is activated. � Identify potential triggers � Identify physical warning signs � Pay attention to your thinking � List techniques that may help you stay in control during a crisis situation.
Self-control must be developed, practiced, and revised throughout your career and personal development. 162 It is the mechanism that we use to minimize the likelihood that we will have an Alarm Reaction.
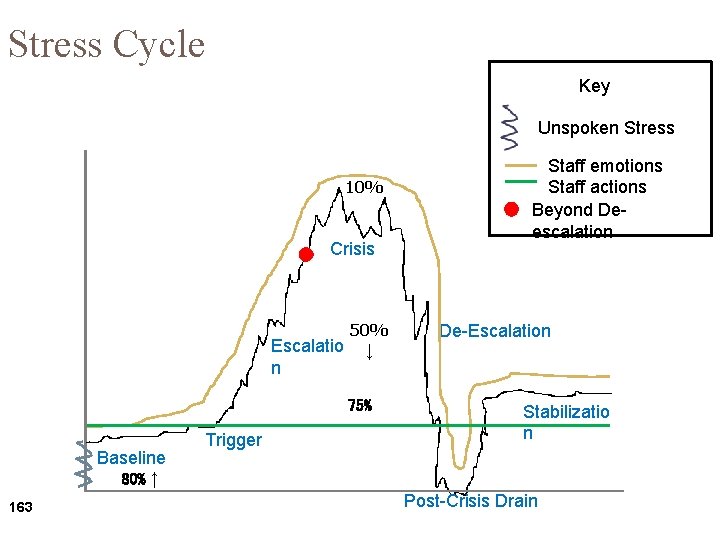
Stress Cycle Key Unspoken Stress 10% Crisis Escalatio n 50% ↓ 75% Baseline 80% ↑ 163 Trigger Staff emotions Staff actions Beyond Deescalation De-Escalation Stabilizatio n Post-Crisis Drain
De-escalation May Include: 164 Breathing slows to a more normal rate Muscle tension decreases Facial expressions change Fewer threats or attempts to hurt self or others Responds to verbal cues
MODULE 10 CRISIS MANAGEMENT REASONABLE RESPONSE PPI DEFINITIONS 165
PERSONAL SPACE • Personal space is an approximate area surrounding an individual in which other people should not physically violate in order for them to feel comfortable and secure. • It is the zone around individuals which they regard as psychologically theirs. Class Exercise 166
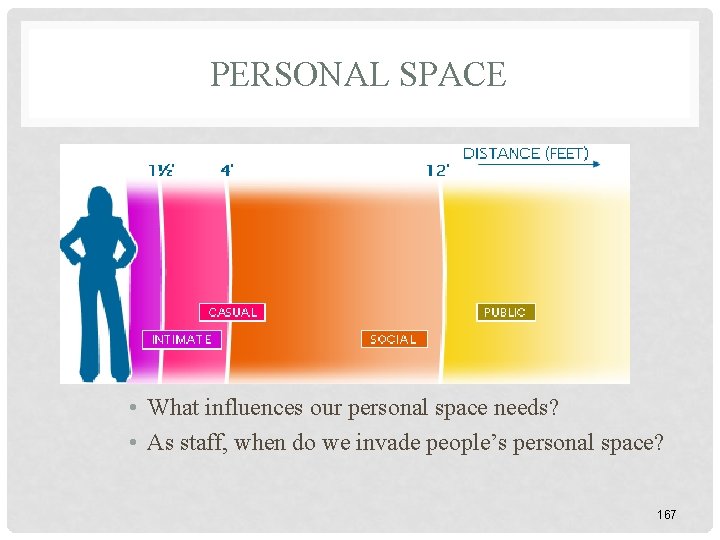
PERSONAL SPACE • What influences our personal space needs? • As staff, when do we invade people’s personal space? 167
168
RESPONDING TO ESCALATION • Remember: • The “thinking brain” of all escalated people is turned off • Managing the escalating person means we have to appeal to their survival brain • At this point in the stress cycle the goal is to keep everyone safe! 169
ASSESSING THE SITUATION • Teaching and negotiating during escalation is non-productive • However, a person’s response to your negotiation is a good indication of their escalation. • Their response is feedback for you on how you should respond. 170
ASSESSING THE SITUATION • Constantly ask yourself, “What is going on? ” • What is the consumer’s executive functioning deficits? • Assumption, the enemy of Assessment! • Use grounding/directive statements to the person • State their name • “Stop” • “Calm Down!” 171
POWERS OF OBSERVATIONUSE ALL OF YOUR SENSES: • Changes in frequency, duration, and intensity of behavior • Changes in facial color, expressions, or moods 172
CHOOSING OUR RESPONSE When responding to a person who is trying to injure him/herself or others, match the response to the level of injury threatened. 173
CONCEPT OF REASONABLE RESPONSE Just enough intervention (physical or nonphysical) for protection from injury and no more than is absolutely necessary. Less risk of injury by the intervention than what is threatened by the assault. 174
WHAT TO CONSIDER • Likelihood of injury • Intensity of the situation • Severity of injury • Possible outcomes of the situation • Established Protocols 175
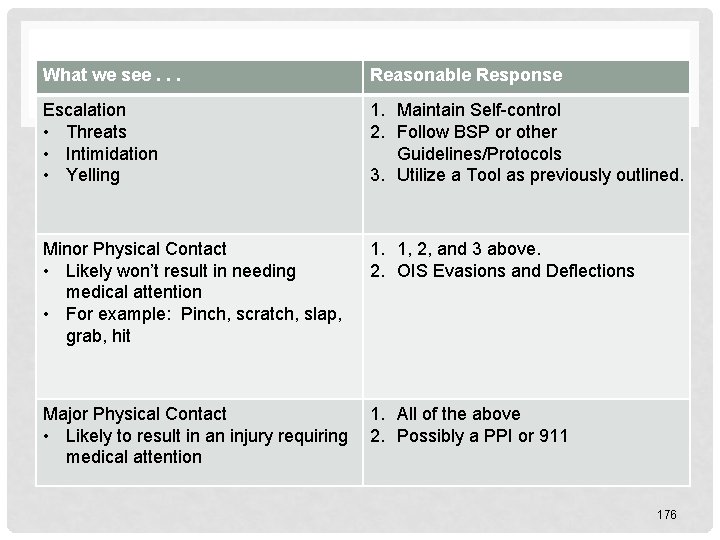
What we see. . . Reasonable Response Escalation • Threats • Intimidation • Yelling 1. Maintain Self-control 2. Follow BSP or other Guidelines/Protocols 3. Utilize a Tool as previously outlined. Minor Physical Contact • Likely won’t result in needing medical attention • For example: Pinch, scratch, slap, grab, hit 1. 1, 2, and 3 above. 2. OIS Evasions and Deflections Major Physical Contact • Likely to result in an injury requiring medical attention 1. All of the above 2. Possibly a PPI or 911 176
Despite our best efforts to prevent a crisis through proactive and deescalation strategies… Crises may occur. 177
RESPONDING WITH DIGNITY & RESPECT Dignity - quality or state of being worthy, honored, or esteemed Respect - an act of giving particular attention; high or special regard 178
REMEMBER • Maintain Self-Control • The Person’s Plan • Direct/Simple Communication • Timing/Patience • Stop and Think • Spontaneity 179
PROTECTIVE PHYSICAL INTERVENTION (PPI) Protective Physical Interventions are safety procedures utilized with an individual that assists in keeping the person protected from harming themselves or others through supportive measures, as taught in the Oregon Intervention System. 180
USE OF PROTECTIVE PHYSICAL INTERVENTION • As a last resort • According to OAR • Never deliberately causes pain • Fully documented and reported 181
WHEN IS A PPI APPROPRIATE? • We are responding to a very challenging and potentially injurious behavior. • The behavior can be safely controlled with a protective physical intervention. • The intervening people providing support are sufficiently trained and can reasonably expect to achieve safe control. 182
WHEN IS A PPI AUTHORIZED? 1. During an EMERGENCY and/or CRISIS situation 2. As part of a plan to maintain health and safety • PBIS Plan/IEP process • Physician’s order 183
THE USE OF PROTECTIVE PHYSICAL INTERVENTION WITHOUT AUTHORIZATION MAY REPRESENT “WRONGFUL RESTRAINT” AND WILL MOST LIKELY RESULT IN REVIEW. 184
REMEMBER The use of Protective Physical Intervention is our LAST RESORT to PREVENT INJURY to the person we support, others when faced with an IMMEDIATE THREAT. 185
PHYSICAL INTERVENTION GUIDELINES • Is there a protocol/plan for safe intervention? • Allow the individual to save face • Start with least intrusive intervention • Talk to/Redirect the person • Evade and assist others to evade • Who should respond? • Has everyone been trained? 186
DISCLAIMER The processes outlined in the OIS workshop have been proven safe and effective when applied correctly. However, proper implementation is the responsibility of the persons involved. Instruction cannot be substituted for good judgment. 187

All training in OIS techniques must be conducted by an approved and certified OIS instructor. There are no exceptions. 188
PHYSICAL PRACTICE Follow the Standards of Physical Skills Training Manual 189
- Slides: 189