1 Scientific Office DISORDERS OF LIPID METABOLISM DISEASES
1 Scientific Office DISORDERS OF LIPID METABOLISM & DISEASES RELATED By : Hossam Erian
SECTION I DYSLIPIDAEMIA 2
DYSLIPIDAEMIA What is The Meaning of Dyslipidemia? * Dyslipidemia expresses the broadest term explaining any lipid disorder (any abnormally high levels lipoproteins in blood). * It explains also any abnormal ratio between different types of lipoproteins ( HDL , LDL , VLDL ). 3
* Dyslipidaemia includes also another term HYPERLIPIDAEMIA What Is Hyperlipidaemia ? Hyperlipidemia is a more specific term , it explains elevated blood cholesterol OR elevated triglycerides OR both of them 4
Terminology of Lipid Disorders : * Hypercholesterolemia → Elevated blood cholesterol level. * Hypertriglyceridemia → Elevated triglyceride levels in blood * Hypolipoproteinemia → Decreased levels of lipoproteins (HDL) * Hypoalphalipoproteinemia → Decreased level of HDL. 5
Classification of Hyperlipidaemia * Classification of hyperlipidemia … ( hypercholesterolemia & hypertriglyceridemia) is usually according to cause or etiology. * Hyperlipidaemia is classified as : Primary hyperlipidemia → Caused by genetic factors. Secondary hyperlipidemia →Caused by ( diet / disease / drug). 6
Primary Hypercholesterolemia Familial Hypercholesterolemia (F H) * (FH) is the example of primary hypercholesterolemia It is due to genetic defects in LDL receptors → ↑ blood cholesterol. 7
Primary Hypertriglyceridaemia : * It is a form of hyperlipidaemia due to elevated level of chylomicrons which is called Hyperchylomicronemia. 8
Familial Combined Hyperlipidaemia (genetic): * In that type , the family members are suffering from : * Primary hypercholesterolemia → ↑ cholesterol level. * Hypertriglyceridemia → ↑ triglycerides & chylomicrons. * Elevated LDL , VLDL. 9
Secondary Causes of Hyperlipidaemia 1 – Diet (high fat & cholesterol intake). 2 – Diabetes mellitus. 3 – Pregnancy. 4 – Obesity. 5 – Drugs like (Beta blockers , thiazide diuretics). 10
6 – Nephrotic syndrome. 7 – Systemic lupus erythromatosus (an auto-immune disease). 8 – Hypothyroidism (decreased activity of the thyroid gland). N. B : Saturated fats in the diet raise levels of LDL by suppressing the activity of LDL receptors and increasing liver production of cholesterol. 11
SECTION 2 ATHEROSCLEROSIS 12
ATHEROSCLEROSIS What Is Atherosclerosis ? * Atherosclerosis is a disease in which fatty substances are gradually formed in the inner layer of the coronary arteries → narrowing (stenosis) → occlusion of coronary arteries → reduction of blood flow to heart tissue →myocardial infarction 13
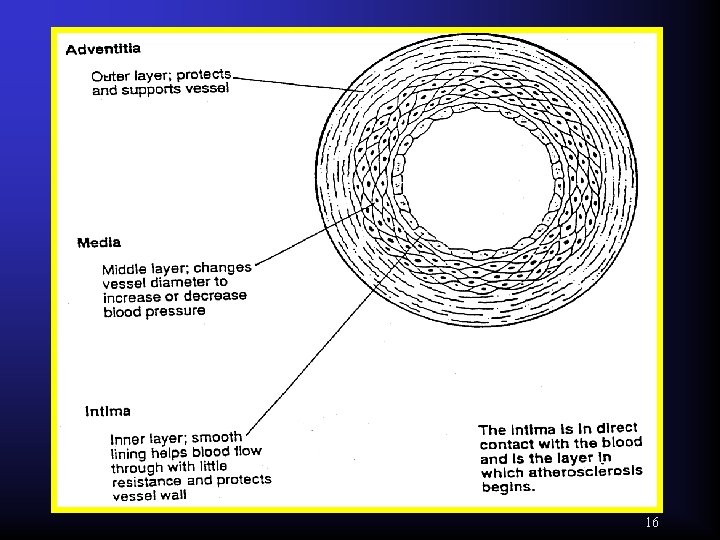
General View on Anatomical Structure of The Artery Wall * The artery wall consists of 3 layers : 1 – The Adventitia Layer : * The outer layer , composed of connective tissue, it supports and protects the vessel. 14
2 – The Media Layer : * The middle layer , composed of smooth muscles and elastic tissue (elastic fibers). 3 – The interna Layer : * The inner layer , composed of a thin endothelial cells which form a smooth lining to help the blood to flow through the artery with the minimal resistance. 15
16
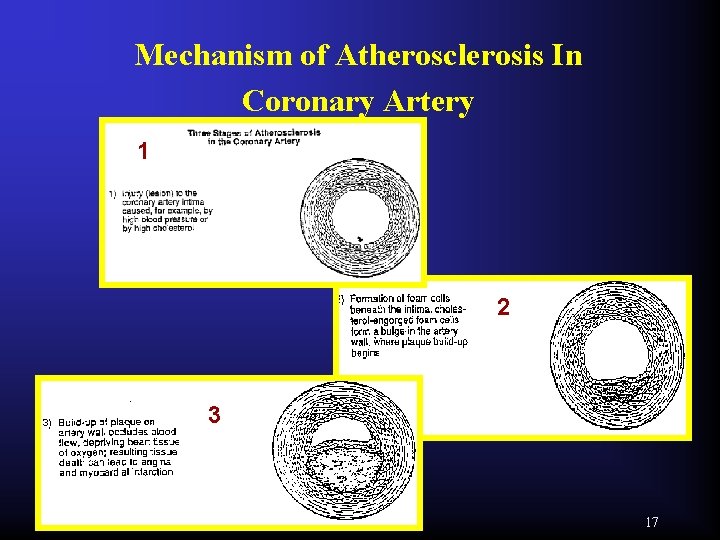
Mechanism of Atherosclerosis In Coronary Artery 1 2 3 17
Mechanism of Atherosclerosis In Coronary Artery Factors Affecting Atherosclerosis : 1 - Age 2 – Hypertension 3– Diabetes 4 – Smoking 5 – Stress 6– Obesity 7 – High Cholesterol levels. 8 - Atherosclerosis of the coronary artery develops within 3 stages 18
Stage 1 : * An injury occurs in endothelial cells of the intema layer , due to long term stress (as high blood pressure) N. B : The coronary arteries are susceptible to such injuries because they are small sized and highly narrow branched. * This injury (lesion) in the intema either heal without damage OR → stage 2 19
Stage 2 (The Atheroma Stage) : An atherosclerotic plaque develops through the following steps 1 – Fatty streaks (thin yellowish lines of fats) are precipitated on the endothelial surface of the artery , & accumulated at the area of the injury. 20
2 – Macrophages come to the injury as a defense mechanism 3 – Macrophages engulf any debris at the injury. 4 – Due to ↑ cholesterol in blood , macrophages engulf also LDL particles containing that cholesterol. 21
5 – After macrophages ingest cholesterol , they are transformed to what is called Foam Cells which are filled with cholesterol. (they are also called cholesterol engorged foam cells) 6 – After that the foam cells are embedded under the endothelial cells forming a bulge in the artery wall , this bulge is called Atherosclerotic Plaque 22
7 – The fatty streaks reaccumulate on the atherosclerotic plaque in the artery wall and become thicker and fibrous , & become larger in size and occlude the artery lumen This is called … ATHEROMA Atheroma = Fatty streaks + Atherosclerotic plaque 23
Summary of stage 2 : Injury to intema → fatty streaks precipitation macrophages come to injury → macrophages engulf LDL cholesterol → transformed to foam cells → embedded under endothelial cells → atherosclerotic plaque which is combined with fatty streaks and fibrosis → atheroma → Occlusion of coronary 24
Stage 3 : * Atheroma occludes blood flow → the heart tissue is deprived of oxygen and nutrients → ischemia (lack of blood flow to the heart tissue) → the prolonged ischemia → cell death and tissue damage which is called Myocardial Infarction (MI) 25
Myocardial Infarction → symptoms of acute Angina Pectoris → may lead to sudden death Heart tissue becomes weak → Ventricular arrhythmia , Shock &Congestive heart failure 26
SECTION 3 RELATION BETWEEN CHOLESTEROL & CORONARY ARTERY DISEASE ( CAD ) 27
Relationship between Cholesterol & Coronary Artery Disease (CAD) There are many evidences which prove that the elevated blood cholesterol increases the risk of coronary artery diseases (CAD) 28
These evidences are : 1 – Genetic Evidence 2 – Epidemiologic Evidence 3 – Intervention Study Evidence 29
1 – Genetic Evidence : * Genetic familial hypercholesterolemia (FH) is the link between cholesterol and CAD. * Individuals with this condition Lack LDL receptors that are responsible for the removal of LDL from blood. 30
* The lack of LDL receptors → elevated LDL cholesterol in blood → LDL deposit excess cholesterol in the walls of blood vessels → Atherosclerosis and CAD. 31
The lack of LDL receptors → may be : Partial Lack of LDL receptors (Heterozygous FH): * Individuals who inherit a gene for this disease from one parent → decreased or deficient number of LDL receptors (This is called Heterozygous FH). 32
* Total cholesterol levels exceed 300 mg / dl (twice the normal). * CAD usually developed by age 45 years. * Incidence of heterozygous FH is about 1 in 500 people. 33
Complete lack (Homozygous FH) : * Individuals who inherit genes from both parents → complete lack of LDL receptors (this is called Homozygous FH). * Total cholesterol levels range from 600 – 1000 mg / dl (4 times that of normal) Incidence is extremely rare 1 in 1000, 000 people 34
2 – Epidemiologic Evidence : * Epidemiologic (population) studies examined the relationship between disease , patient and environment. Aim of these studies : To explain the link between cholesterol and CAD. 35
The Framingham Heart Study ( FHS ) * The aim of Framingham heart study is to determine the most serious risk factors associated with cardiovascular disease. * The study has followed 5000 men and women of the residents of Framingham city of Massachusetts state in USA. 36
* The study started in 1948 , the 5000 case were medically tested to record : Blood pressure , weight , age , life style and ECG (electro-cardiogram) * The medical examination is repeated every 2 years looking for signs of CAD with complete analysis of all factors associated with the incidence of CAD as… 37
Smoking , Obesity , Male sex , Age , High total blood cholesterol , Hypertension , Stress , ECG abnormalities and family history. 38
* The study has provided an important evidence linking heart disease with : 1 – Smoking. 2 – Hypertension. 3 – High blood cholesterol. * The risk of CAD increases significantly when cholesterol rises above 200 mg / d. L The following Diagram explains the Framingham Heart Study …. 39
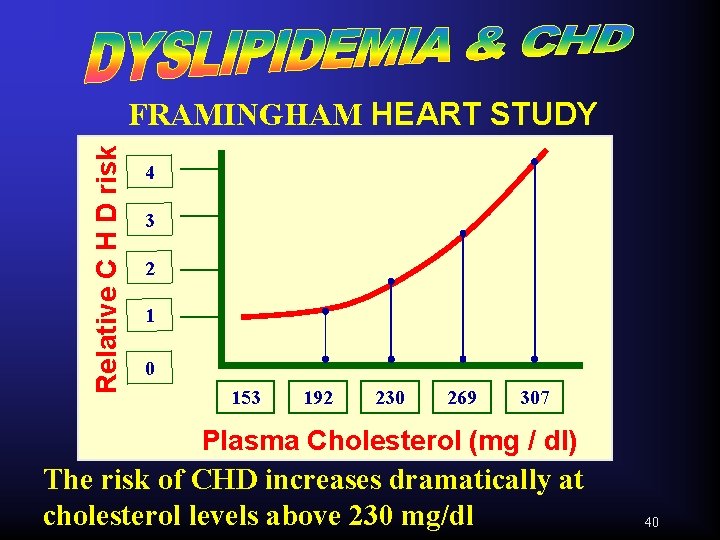
Relative C H D risk FRAMINGHAM HEART STUDY 4 3 2 1 0 153 192 230 269 307 Plasma Cholesterol (mg / dl) The risk of CHD increases dramatically at cholesterol levels above 230 mg/dl 40
Is Low Total Blood Cholesterol Sufficient to Confirm Low Risk of CAD ? * All studies suggest that reducing total blood cholesterol below 200 mg / d. L Does not reduce the risk of CAD too much … Even if the total cholesterol is low, there may be an increased risk of CAD 41
WHY ? * The Framingham heart study also confirmed that : The normal total cholesterol does not mean that the patient is at low risk of CAD , The more important factor is the HDL cholesterol ( HDL-C ) level. 42
If total cholesterol is normal and HDL is low → high risk of CAD. If total cholesterol is normal and HDL is high → low risk of CAD. As the HDL are considered as protection against CAD So …. their low level → increases the risk of high cholesterol → high risk of CAD. 43
3 – Intervention Study Evidence : * The intervention study evidence have proved the risk between blood cholesterol and the risk of CAD through different ways: Decreasing blood cholesterol → decreases the risk of CAD. 44
Coronary Intervention Study : - This study gave a physical proof through Angiography … It is a technique through which an image of the atherosclerotic plaque on coronary artery walls is obtained through injecting a radio-opaque substance into the vessels and take X- ray photos 45
- The patients were taking special diet regimen and a lipid – lowering drug. Results : 17 % decrease in the rate of progression of atherosclerotic plaque as followed by photos. 46
General Conclusion about Intervention Study 1 % reduction in cholesterol → about 2 % reduction in CAD ↑ LDL → ↑ risk of CAD And ↑ HDL → ↓ risk of CAD The Helsinki Study : This study was published in 1987 to clarify the link between cholesterol & CAD. 47
Study : Large 5 years study on about 4000 patients (men) with high cholesterol levels but no symptoms of heart disease were divided to 2 groups : 1 st group : Were given a drug that decreases triglycerides and increases HDL levels (Gemfibrozil - or Lopid). 48
2 nd group : Were given placebo Results : In patients who received drug therapy : - HDL was increased. - LDL was moderately reduced. - 34 % decrease in the risk of CAD. 49
Management & Control of Dyslipidemia 1 – Diet Therapy 2 – Exercise 3 – Excessive Weight Reduction 4 – Drug Therapy … That will be Discussed Later …. Good Luck 50
- Slides: 50