1 Running Head HUMAN PAPILLOMA VIRUS Human Papilloma

- Slides: 18

1 Running Head: HUMAN PAPILLOMA VIRUS Human Papilloma Virus, causing Cervical Cancer in Women Taylor Rose Conway
2 HUMAN PAPILLOMA VIRUS Abstract The human papillomavirus is an STD that is being spread widely throughout the world. There are vaccinations that can help to prevent it but prevalence and incidence rates still seem to be in somewhat high numbers. The human papillomavirus is contagious through contact with bodily secretions. Which is why using prevention such as condoms and other items are suggested. There is also a vaccination that has come out in the past few years. Men can contract HPV and are known as silent carriers because they show no signs or symptoms most the time. HPV can then cause cervical cancer in women but not in men because they do not have a cervix. This virus is sadly very common and spread from lack of knowledge and prevention. I am hoping in reading this essay you will educate yourself on prevention, as well as the cause and effect of the HPV virus.
3 HUMAN PAPILLOMA VIRUS Part 1: Person, Place, Time Inside the U. S. Disease/Condition Topic Selection Human Papilloma Virus (HPV)- infectious. Are you sexually active or ever have been? Did you know that you now have a 1 in 2 chance of contracting HPV, which is if you don’t already have it? The Human Papilloma Virus is the most common Sexually Transmitted Disease. There are over 150 strains of the virus. There are now vaccines to help prevent most strains of the virus, but must be administered before being sexually active, around the age of 11 -14. There are so many ways to transmit this virus but the most common is through sexual intercourse, vaginal, and oral. Ways of preventing this is abstaining, avoiding fluid transmission, and using protection when sexually active. (Ahmed, HPV) The CDC estimates that there are over 6. 2 million new cases of infection each year in the United States. This trend illustrates that HPV is the highest rate of sexually transmitted disease compared to any others. Currently, there are over 20 million women that are infected. Transmission mainly happens in the first 2 to 3 years of sexual contact a person has and is found to be most common in women and men in their teens and early twenties. Sadly, this is not an age specific virus so there is no way to fully specify who it effects the most, all that can be said is that people who have unprotected sex are most susceptible as well as those who are active before the age of 21. (Yu Y, Vaccine) People affected before the age of 21 most likely will not know until later in there 20’s because gynecologists are beginning not give PAP smears until the age of 21. So it can come and go before then or linger until their first test.
HUMAN PAPILLOMA VIRUS 4 Disease condition specifics: A person is most susceptible to HPV when they are having unprotected sex before the age of 21 when there still going through changes in their hormones. This is why prevention is so crucial to for anyone, but especially young individuals. There are symptoms that hit before all the main symptoms and this is called presymptomatic stages. With HPV these things are a change in odor or an increase in infections. These things are not necessarily a giveaway for having HPV. But once diagnosed people can realize that was what was leading to the more severe conditions. But some have said to have a mildew smell that is unusual, as well as a frequency in yeast infections and bacterial vaginosis. Things that can make a person realize they might need to get checked is when they start getting genital warts. Usually though people are unaware until they get their routine pap smear. (Lagos, screening) Because this is a virus with very minimal symptoms it is not very common for people to know they even have it before their routine Pap smear. A lot of people do not even see their gynecologist on a yearly basis for a well women check, so the virus can come and go already before the next pap smear, or they can have it for years straight. From the point of finding out it is usually suggested to abstain or at least use protection. A person will either recover form it, or get worse and it will turn to cervical cancer. HPV can act like a flu virus and go away and the virus leave your body or it can stay lead to cervical cancer. Cervical cancer is nothing to joke about, it can completely corrupt your cervix, fallopian tubes, and ability to have children.
HUMAN PAPILLOMA VIRUS 5 Data & Measures Used Epidemiological observation on HPV and how cervical cancer is a result is measured by cases. The tools used is case series, control studies, and prevalence surveys. Some epidemiological measures used for tracking HPV and cervical cancer are once again using case studies. One being controlled studies, another cohort studies, and intervention studies. By producing these studies, they are able to see where it is worse, what seems to help, and which strains cause cancer. Without these epidemiological studies we would not be to deal with the control of the virus. The incidence rate is hard to determine because a lot of people are unaware they have HPV and sometimes do not get it diagnosed before it is out of there body or when it turns to cervical cancer. (Bosch, relation) When it turns to cervical cancer is when things begin getting reported and there is more data to support that. As stated earlier, there is estimated well over 6 million new cases by the CDC. Human Papilloma Virus is the largest most common STD than any other, because of how easily it is transmitted. But it is not a precise number because the CDC does not require positive HPV tests to be reported. (La Vincente, implementation) As for a mortality rate, HPV itself does not cause mortalities, but it turns to cervical cancer which does. Back in 2005 the mortality rate was 67. 8% and currently it is 64%, so it has slightly gone down. (surveillance). This is due to catching dysplagic cells before they turn to cancer as well as the Gardasil vaccination has come out since 2005 and been preventing the two main strains of HPV that cause cancer.
HUMAN PAPILLOMA VIRUS 6 Patterns of Disease in the United States Human Papilloma Virus is sadly a very common sexually transmitted infection among people. Not very many people get checked for it or even know they have it. People in the united states don’t really even know much on it until they or someone they know has been told they have it. Sometimes it is even too late for them and it turns into cervical cancer. Human Papilloma Virus causes other cancers (prostate, anal, etc) but cervical is the most common. Most men do not even know they have HPV they are called silent carriers. (Cunningham) They usually do not present symptoms as women do. Therefor they are not able to know or tell a sexual partner they have it and to use protection. That is why using protection is such an important thing to do with every person you are with. Unfortunately, condoms do not cover all areas of the body you may use in sexual intercourse. This not protecting you from a different source of the spread of HPV. Any person who has ever had sexual or genital contact with another person, intercourse is not necessary is at great risk of getting HPV.
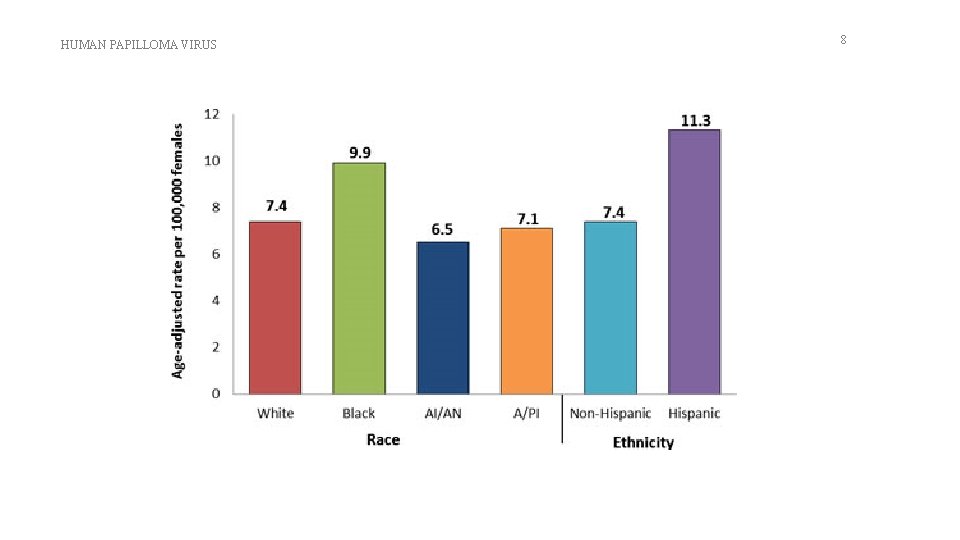
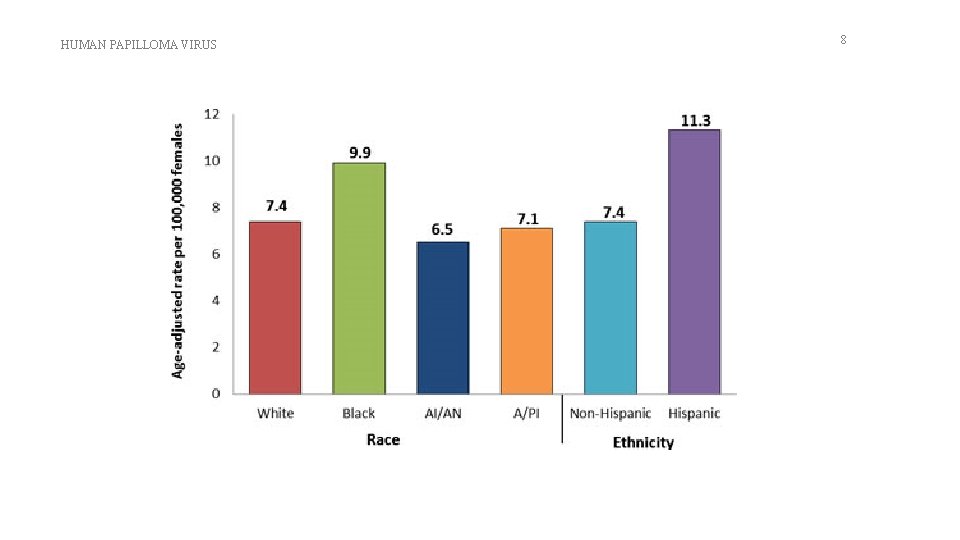
7 HUMAN PAPILLOMA VIRUS The CDC does not require results to be reported, as well as herpes. So I am not able to get prevalence rates are as precise as other diseases and such. So this makes it inconclusive when getting certain exact rates. HPV is more common among women, but men don’t usually know they have it because they are known as silent carriers. As for cervical cancer that is solely women who contract that. When it comes to race for Blacks and Hispanics had a higher rate of HPV associated cancer then white women. AS for Asians have a lower rate than white women and men. The rate pf HPV is determined by which races are more likely to have unprotected sex. (Lili, comparative) also refer to graph on slide 8. (HPVA, 2014) The overall median age throughout the years for cervical cancer is 48 years, as for the age for contraction of HPV is before the age of 30. The HPV virus can stay dormant in your body, then later in life cause your cells to turn dysplagic, which then turns to cancer. There a broad range of ages because contraction and turning to cancer happen at two completely different times. HPV can be contracted young but not arise as cancer until later in life.
HUMAN PAPILLOMA VIRUS 8
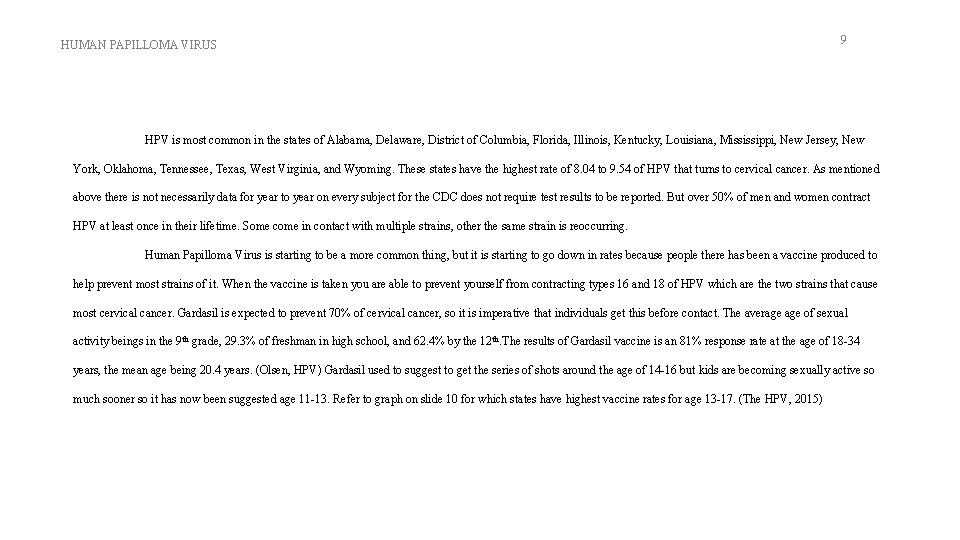
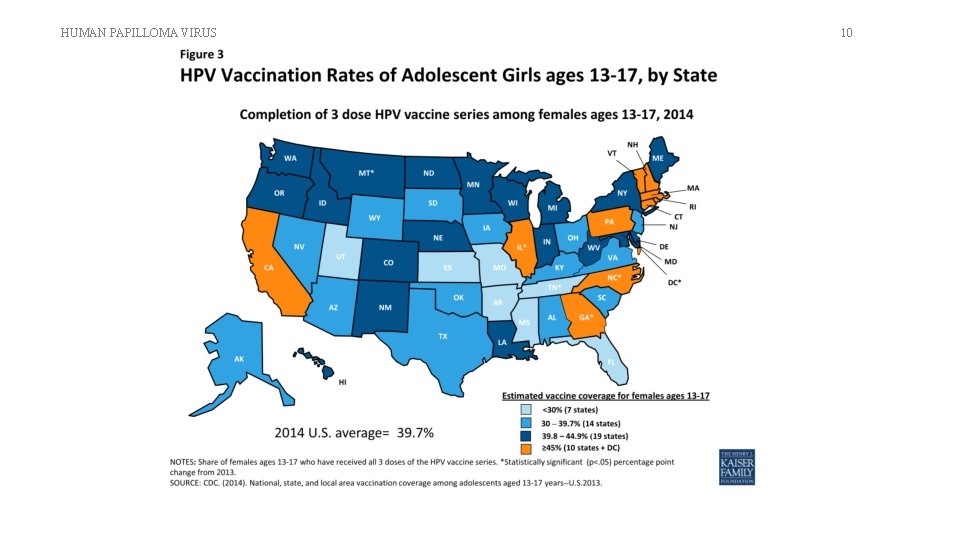
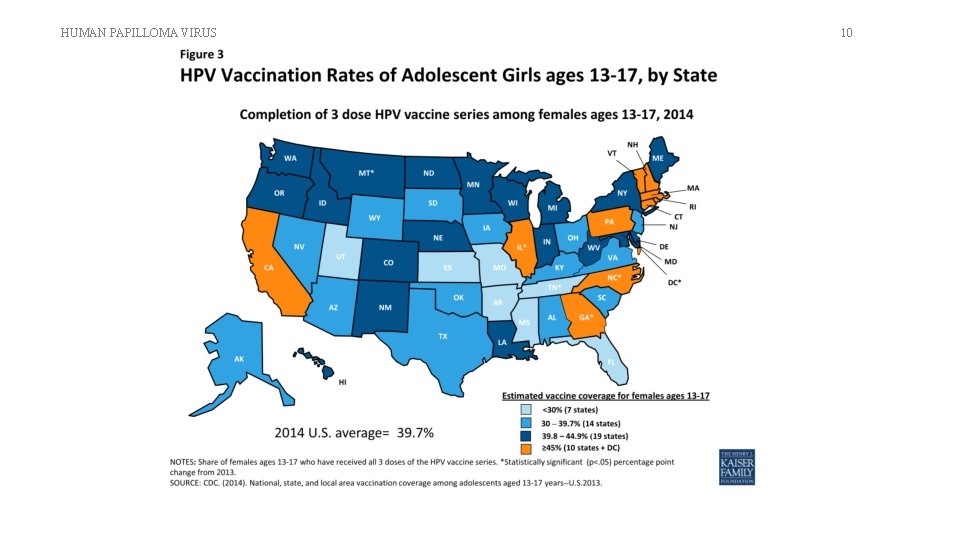
HUMAN PAPILLOMA VIRUS 9 HPV is most common in the states of Alabama, Delaware, District of Columbia, Florida, Illinois, Kentucky, Louisiana, Mississippi, New Jersey, New York, Oklahoma, Tennessee, Texas, West Virginia, and Wyoming. These states have the highest rate of 8. 04 to 9. 54 of HPV that turns to cervical cancer. As mentioned above there is not necessarily data for year to year on every subject for the CDC does not require test results to be reported. But over 50% of men and women contract HPV at least once in their lifetime. Some come in contact with multiple strains, other the same strain is reoccurring. Human Papilloma Virus is starting to be a more common thing, but it is starting to go down in rates because people there has been a vaccine produced to help prevent most strains of it. When the vaccine is taken you are able to prevent yourself from contracting types 16 and 18 of HPV which are the two strains that cause most cervical cancer. Gardasil is expected to prevent 70% of cervical cancer, so it is imperative that individuals get this before contact. The average of sexual activity beings in the 9 th grade, 29. 3% of freshman in high school, and 62. 4% by the 12 th. The results of Gardasil vaccine is an 81% response rate at the age of 18 -34 years, the mean age being 20. 4 years. (Olsen, HPV) Gardasil used to suggest to get the series of shots around the age of 14 -16 but kids are becoming sexually active so much sooner so it has now been suggested age 11 -13. Refer to graph on slide 10 for which states have highest vaccine rates for age 13 -17. (The HPV, 2015)
HUMAN PAPILLOMA VIRUS 10
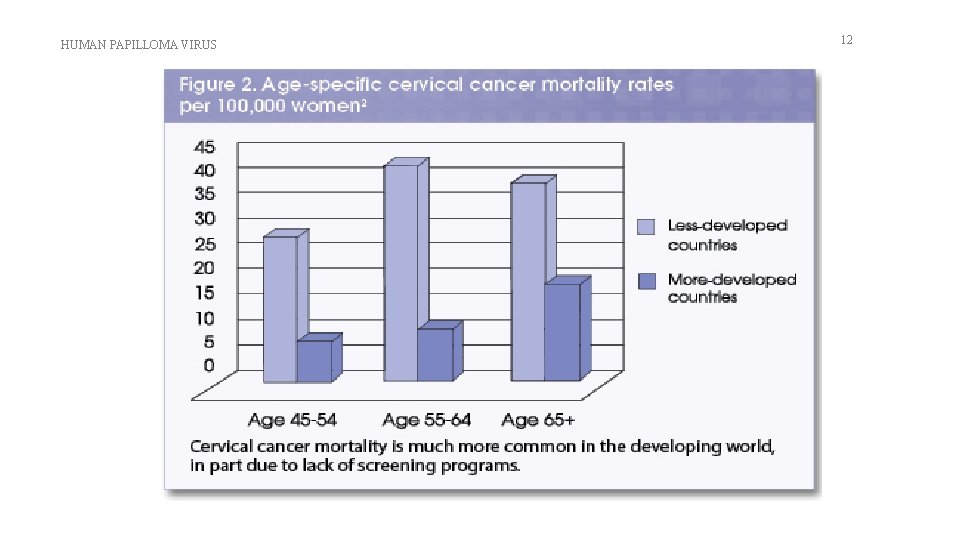
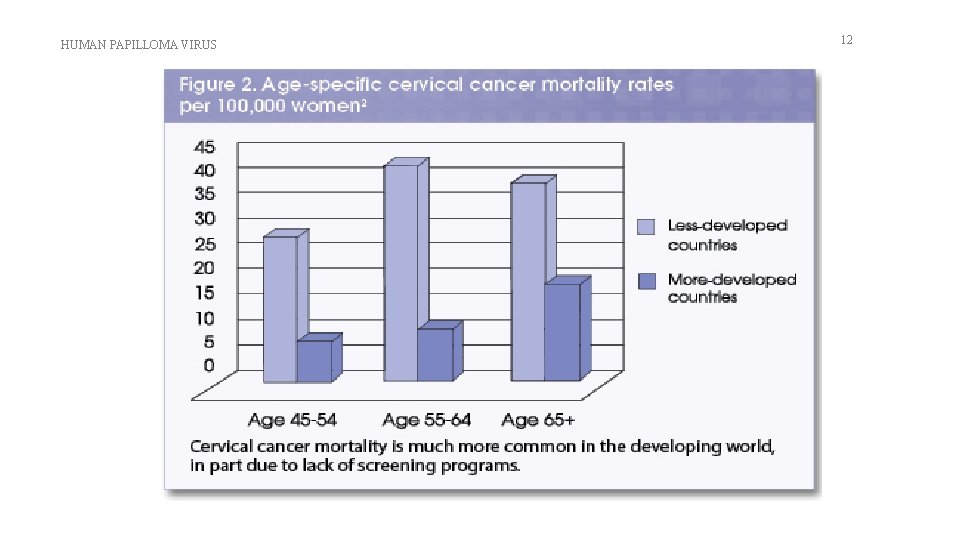
HUMAN PAPILLOMA VIRUS 11 Part 2: Person, Place, Time Outside the U. S. Patterns of Disease outside the United States HPV is something that hinders the medical community not only in the US but in other countries as well. The countries that I will be referencing the most in this portion of the essay is going to be the United Kingdom and Africa. I chose the United Kingdom because they have a lot of medical resources to where they can document cases very well, and Africa I chose because it is an underdeveloped country and they tend to be more affected by things like this. There are many factors that affect cervical cancer as well as many different regions that suffer from cervical cancer. Things like gender, race, age, and location all have different data. See graph on slide 12 for statistics on underdeveloped countries. (HPV, 2010) When it comes to the United Kingdom cervical cancer is the 6 th most common carrier in Europe for women and overall the 16 th most common cancer. This giving over 58, 000 new cases a year in the United Kingdom. As for comparing that to worldwide numbers cervical cancer is the 4 th most common cancer for women worldwide, and the 7 th most common cancer overall. Over 527, 000 new cases are found each year worldwide. ( Elfström, 2015). By learning statistics based on location, gender, age, and race you are able to figure which areas are more affected and who in those areas are affected the most as well.
HUMAN PAPILLOMA VIRUS 12
HUMAN PAPILLOMA VIRUS 13 When it comes to gender, that is fairly easy to answer because HPV does affect both men and women but cervical cancer only affects women because they contain a cervix. That is why it is known that men affect whether or not a woman get cervical cancer sometimes. Another thing that affects incidence and prevalence rates is the race or ethnicity of a person. In the UK back in 2010, Hispanic women had the highest rate of getting cervical cancer, then followed by black and then whites. In 2010, 10 women per every 100, 000 were affected, and in 2016 that was lowered to 9. For black women in 2010 the number was 11 for every 100, 000 and in 2016 this went down to 7. Lastly for white women the number was eight and every 100, 000 in 2010 and this went down to 7 in 2016. This showing less women we're beginning to be affected by cervical cancer. In my opinion this could be because vaccinations are becoming more easily accessible. The above statistics are for the incidence rate for cervical cancer in the UK. The next set of results is the death rate. In 2010 Hispanic women had 2. 5 deaths per 100, 000 and in 2016 this change to 3. 5. For black women it was 5 for every 100, 000 in 2010, and went down to 4. 5 in 2016. And last, it was 2. 5 in 2010 for white women and remain the same in 2016. This showing that the death rates or very inconclusive in whether or not it was raised, went down, or stayed the same. (Worldwide date)
HUMAN PAPILLOMA VIRUS 14 A factor that I find that affects the rate of cervical cancer the most would be age. In the UK back in 2010 the highest rate of an age when cervical cancer was found was age 25 years to 40 years. In 2016 that number is now 20 years to 35 years over 52% of cases are found to be from age is less than 45 years old. The data begins at the age of 15 years to 19 years, usually peeking from 25 to 29 years with the highest rate, and then it drops back down to zero at the age of 60 years to 64 years. Cervical cancer can also have different rates in different locations and regions. As for the UK as a whole 3, 207 women are affected in every 100, 000 back in 2010. This can also be broken up into areas, such as England has 2, 639 affected, whales had 146, Scotland had 318, and North Ireland was 104. (Arbyn, 2009). But as for places like Africa they had much higher rates with death. Around 190, 000 deaths each year are in developing countries such as Africa. Also, if you look into statistics roughly 84% of cervical cancers worldwide occurred in less developed countries such as Africa. Things that affect these places having much higher rates is mainly because of the lack of effective screening programs. In underdeveloped countries only 5% of women are screened for cervical cancer as compared to in the UK 40 to 50% of women are. This just goes to show that resources, vaccinations, and screening processes are vital to statistics when it comes to preventing, touching, and treating cervical cancer.
HUMAN PAPILLOMA VIRUS 15 Summary & Conclusion Since the 1970 s the cervical cancer incidence rate in females has drastically increased by more than 44% in the United Kingdom. But in the last decade incidence rates in females have remained stable. (Paolo, 2013). Something that I learned that was very common in all of the data was that areas in poverty do affect incidence rates. As in Africa, in England rates are higher in the more deprived and underdeveloped areas. Information cervical cancer is something that affects the entire world. HPV is a very common sexually transmitted infection that both men and women can spread as read in earlier parts of my essay. That is why I'm hoping all this information raises Awareness on protection, prevention, screenings, and treatment.
HUMAN PAPILLOMA VIRUS 16 References Ahmed H, Bensumaidea S, Ashankyty I. (2015) Frequency of Human Papilloma Virus (HPV). Infectious Agents & Cancer. February 19, 2016 Arbyn, M. (2009) European Guidelines for Quality Assurance in Cervical Cancer Screening. Oxford Journals. 21 (3): 448 -458 Bosch, F. X. , Lorincz, A. , Muñoz, N. , Meijer, C. J. L. M. , & Shah, K. V. (2002). The causal relation between human papillomavirus and cervical cancer. Journal of Clinical Pathology, 55(4), 244– 265 Cervical cancer statistics. (2015). Retrieved April 16, 2016. Cunningham-Erves, J. (2015) HPV Vaccination of College Males. College Student Journal. February 19, 2016
HUMAN PAPILLOMA VIRUS 17 References continued Elfström, Miriam. (2015) Cervical cancer screening in Europe: Quality assurance and organisation of programmes. European Journal of Cancer, 51(8), 950 – 968 Grue, S. (2013). Surveillance, Epidemiology, and End Results Program. Retrieved March 16, 2016. HPV-Associated Cervical Cancer Rates by Race and Ethnicity. (2014). May 01, 2016 HPV in United states graph - Google Search. (2010). May 01, 2016 La Vincente S, Mielnik D, Mulholland El. (2015) Implementation of Human Papillomavirus (HPV) vaccine. BMC Public Health February 19, 2016. Lagos M, Van De Wyngard V, Ferreccio C. (2015) HPV 16/18 genotyping for the triage of HPV. Infectious Agents & Cancer. February 19, 2016 Lili H, Tuerxunayi M, Mayinuer N. (2015) Comparative study of HPV. Experimental & Therapeutic Medicine. February 19, 2016
HUMAN PAPILLOMA VIRUS References continued Olsen J, Jørgensen T. (2015) Revisiting the cost of universal HPV-vaccination. Cost Effectiveness & Resource Allocation. February 19, 2016. Paolo, Rossi (2013) New Cervical Cancer Screening Guidelines on Both Sides of the Atlantic. European Medical Journal. 43(4) 36 -65 Rock, C. (2016). Genital HPV Infection - Fact Sheet. Retrieved April 16, 2016. Smock, Tanner. (2010) Worldwide data | World Cancer Research Fund International. (n. d. ). Retrieved April 16, 2016. The HPV Vaccine: Access and Use in the U. S. (2015). May 01, 2016. Yu Y, Xu M, Xu A. (2016) Human Papillomavirus Infection and Vaccination. Plos ONE. February 19, 2016 18