1 persistent diarrhea PERSISTENT DIARRHOEA AMER YAZDANPARAST MD








- Slides: 62

1 persistent diarrhea
PERSISTENT DIARRHOEA AMER YAZDANPARAST, MD BOOSHEHR UNIVERSITY OF MEDICAL SCIENCES 2 persistent diarrhea
Abstract o o o 3 Definition: persistent diarrhea is defined as an episode that lasts more than 14 days. Introduction: persistent diarrhea has high impact on infantile morbidity and mortality rates in developing countries. Several studies have shown that 3 to 20% of acute diarrheal episodes in children under 5 years of age become persistent. Etiology: the most important agents isolated in persistent diarrhea are: Enteropathogenic E. coli (EPEC), Salmonella, Enteroaggregative E. coli (EAEC), Klebisiella and Cryptosporidium. Clinical aspects: in general, the clinical characteristics of patients with persistent diarrhea do not change with the pathogenic agent. Persistent diarrhea seems to represent the final result of a several insults a infant suffers that predisposes to a more severe episode of diarrhea due to a combination of host factors and high rates of environmental contamination. Therefore, efforts should be made to promptly treat all episodes of diarrhea with appropriate follow-up. Therapy: the aim of the treatment is to restore hydro-electrolytic deficits and to replace losses until the diarrheal ceases. It is possible in the majority of the cases, using oral rehydration therapy and early an appropriate type of diet. Prevention: it is imperative that management strategies also focus on preventive aspects. The most effective diarrheal prevention strategy in young infants worldwide is promotion of exclusive breast feeding. persistent diarrhea
Definition o o o o 4 It is estimated that 3 to 20% of the acute diarrhea episodes among children younger than 5 years old become persistent, and that over 50% of the deaths provoked by diarrhea are associated to persistent episodes. Acute and persistent diarrhoea are not two separate diseases but form a continuum. In 1987, a meeting sponsored by WHO defined persistent diarrhoea as an episode which starts acutely but which lasts at least 14 days. Persistent diarrhoea almost never occurs in infants who are exclusively breastfed. The child's history should be carefully reviewed to be certain there is diarrhoea, rather than several soft or pasty stools each day, which is normal for breastfed infants. In 1987, the World Health Organization (WHO) defined persistent diarrhea as “a diarrheal episode with a presumably infectious cause that starts as an acute episode and lasts in an unusual way, causing the aggravation of the nutritional state and a high life risk condition”. The term does not include chronic or recurrent forms of diarrhea, such as tropical sprue, celiac disease, cystic fibrosis, and other hereditary disorders with diarrheal manifestations. In the bulletin published by WHO, persistent diarrhea was established as the diarrheal episode lasting 14 days or more. persistent diarrhea
Introduction o o o 5 Persistent diarrhea is responsible for high morbidity and mortality rates among infants of low socioeconomic level in developing countries. It appears as cause and effect of malnutrition and it increases the risk of death when associated with latter. Persistent diarrhoea is becoming recognized as an important child health problem in developing countries, although its control and prevention have received less attention than acute diarrhoea. Persistent diarrhoea is an important cause of illness and death in children in developing countries. Moreover, as acute diarrhoea is more widely and successfully treated with oral rehydration therapy (ORT), the proportion of diarrhoea deaths associated with persistent diarrhoea will probably increase. This is diarrhoea, with or without blood, that begins acutely and lasts at least 14 days. It is usually associated with weight loss and, often, with serious non-intestinal infections. Many children who develop persistent diarrhoea are malnourished before the diarrhoea starts. persistent diarrhea
Etiology o o o 6 The excretion of pathogens in the feces of children with persistent diarrhea is common, with isolation rates higher than 40%. In 1998, Andrade et al. had 57. 1% of positivity in the etiologic research. The excretion of pathogens in the feces of asymptomatic children in developing countries is common, what makes the interpretation of epidemiological studies become difficult. The agents most frequently isolated in the feces of children with persistent diarrhea are classic enteropathogenic E. coli (EPEC), Salmonella, enteroaggregative E. coli (EAEC), Klebisiella and Cryptosporidium. Some species of EPEC constitute an important predisposing factor to persistent diarrhea factor. Several researches have studied infants with acute and persistent diarrhea, showing a high concomitance of isolation of EPEC serum groups in the feces and in the jejunal juice. Cruz et al. concluded that EPEC favors the bacterial proliferation in the small intestine. Black, in 1993, evaluated 4 studies carried out in India, Nepal and Bangladesh about persistent diarrhea, and did not find any association of rotavirus with persistent diarrhea. Besides, in this geographic regions, EPEC, Aeromonas, Campylobacter and Shigella did not seem to be particularly associated with persistent episodes of the diarrhea. persistent diarrhea
o o o o o 7 Risk factors malnutrition lactation shorter than 1 month use of antibiotics early episodes of acute diarrhea identification of enteropathogens infections pneumonia sever dehydration artificial suckling treatment with antibiotics younger than 1 year old (63%) uneducated mother previous case of diarrhea within 3 months before hospitalization shorter time of exclusive motherly suckling low birth weight infection by Cryptosporidium a prolonged pause in alimentation duration and gravity of the diarrheal process decrease of the immune function poverty inadequate feeding and environmental contamination persistent diarrhea
Etiology o o 8 EAEC is an important pathogen causative of diarrhea in children, and it has been found more frequently in episodes of persistent diarrhea than in controls. In 1992, in the Northeast of Brazil, a high incidence of enteroadherent E. coli was verified in the feces and in the jejunal juice of children with persistent diarrhea (36% with aggregative adherence, 29% with diffuse adherence, and 13% with local adherence). In the same year, Henry et al. , in Bangladesh, isolated EAEC in the feces of 27. 4% of the diarrhea cases that persisted for more than 14 days and in the feces of 17. 9% of the acute episodes, while Shigella, Aeromonas, Giardia and ETEC appeared more frequently in acute episodes than in persistent ones. In 1993, Bhatnagar et al. , in India, studying 284 children younger than 2 years old with nonsanguineous diarrhea and 107 controls, found EAEC in 21. 4% of the persistent diarrhea cases, in 9. 9% of the acute diarrhea cases, and in 3. 7% of the controls. The isolation of EAEC in persistent diarrhea was significantly higher than in patients with acute diarrhea and in controls, but with no statistical significance. persistent diarrhea
Etiology o o 9 In 1995, Fang et al. reviewed 4, 800 cases of diarrheal disease in Brazil, and 56 children with persistent diarrhea, 52 with acute diarrhea and 42 controls were selected for the investigation. EAEC was isolated in 68% of the persistent diarrhea cases, in 46% of the acute diarrhea cases, and in 31% of the controls. In 1998, Bardhan et al. studied 195 children, out of which 135 had persistent diarrhea, 42 had acute diarrhea, and 15 were controls. EAEC was isolated in the feces of 25. 4% of the children with persistent diarrhea. Other organisms also significantly associated with persistent diarrhea were Aeromonas and Klebisiella. These authors also concluded that EAEC is an important pathogen associated with persistent diarrhea. In 1993, Levine et al. , in Chile, studying children with diarrhea, isolated EAEC at the same frequency both in children with diarrhea and in controls. Out of the 1, 081 episodes of diarrhea evaluated, 103 were persistent, and, out of these, 17 were associated with EAEC (16. 5%). Out of the 96 controls evaluated, EAEC was isolated in 24 (25%). Among the newborns, 77 out of the 662 episodes of diarrhea evaluated were persistent, and 12 of these (15. 6%) were associated with EAEC. However, this agent was also isolated in 10 out of the 77 controls without diarrhea. Therefore, in this study, EAEC was not significantly associated with persistent diarrhea
Epidemiology Lanata et al. 8 followed 677 children below 3 years of age for a period of 27 months, in Peru, and they found an incidence of 8. 1 episodes of acute diarrhea per children per year, and 0. 25 episodes of persistent diarrhea. In this work, 3. 2% of the diarrheal episodes became persistent. o Henry et al. , in Bangladesh, 9 evaluated 363 children for a period of 24 months. The evaluated children had, on average, 1. 5 episode of acute diarrhea and 0. 5 episode of persistent diarrhea per year, seeing that 23% of the diarrheal episodes became persistent. Fang et al. , evaluating children younger than 3 years old in the Northeast of Brazil for a period of 3 years, showed that 10% of the diarrheal episodes evolved for more than 14 days. o In 1993, Sarti et al. , in Mexico, evaluated 1, 034 episodes of diarrhea in children below 5 years of age, out of which 19 were persistent, with a prevalence of 1. 8/100 children with diarrhea (2%). A study performed in Tunisia investigated 380 children hospitalized because of diarrhea for a period of 2 years, and, out of them, 74 (19. 5%) evolved to persistent diarrhea. 12 In Nairobi, Kenya, 384 children with diarrhea were evaluated, and, out of them, 16. 5% evolved persistently in the diarrheal status. o In 1999, in Guinea-Bissau, 319 children with diarrhea below 5 years of age were studied, and, out of them, 40 (12. 5%) evolved for more than 14 days. 14 However, we still observe, in regions of low income in Brazil, that persistent diarrhea presents high prevalence, reaching levels over 50%. o Recently, in February 2000, Lins & Silva showed that out of 246 children younger than 2 years old considered to have diarrheal disease in Recife, 140 (56. 9%) evolved for more 10 than 2 weeks. persistent diarrhea o
Pathophysiology o o o 11 The pathophysiologic mechanisms that may be present and that determine the perpetuation of the diarrheal process, with compromising of the nutritional status, are multiple and complex. Great part of the patients with persistent diarrhea had as onset an episode of acute diarrhea. It is known, nowadays, that some factors resulting from acute diarrhea may propitiate the installation of persistent diarrhea. The enteropathogens, persistent diarrhea according to its virulence mechanisms, provoke lesions in the intestinal mucosa. So, the status of the mucosa barrier and the host’s microbial clearing capacity may influence the vulnerability to the persistence of those lesions. This way, during the diarrheal process, aggression to the mucosa and to the enterocyte brush border occurs, altering its morphology. The malabsorption of carbohydrates depends on the mucosa level of desquamation, considering that the loss of mature epithelial cell provokes a reduction of enzymes in the enteric membrane and increases, in the lumen, the subtract of carbohydrates, which then promote an osmotic phenomenon. Initially, loss of the capacity to hydrolyze and absorb the disaccharides occurs, because of deficiency in the disaccharidases. With the extension of the lesion, glucose and galactose absorption mechanisms and the facilitated fructose absorption may also be affected. The lesions in the small intestine favor the passage of alimentary proteins, intact or partially hydrolyzed by the mucosa, having, as a consequence, allergy to the proteins of the diet (cow milk, soybean protein). persistent diarrhea
Pathophysiology o o 12 A series of pathologic events will start to occur in chain, such as disconjugation and 7 m-dehydroxylation of bile salts, morphologic alterations in the intestinal mucosa, provoking decrease in the absorption surface, and functional lesions with deficiency of enterokinase and of the ATPase (Na+K+) enzym. Besides, desconjugated bile salts and dehydroxylated 7 m are able to provoke alterations in the permeability barrier of the intestinal mucosa. On the other hand, dysfunction in the terminal ileum has been described 48 in patients with persistent. Diarrhea and malnutrition, leading not only to deficiency of the B 12 vitamin, but also to the inadequate absorption of bile salts. The consequent decrease of bile salts pool will lead, first, to the malabsorption of fats of the diet, 49 having as result the steatorrhea, which will deprive the patient of an important caloric offer. Secondly, the excretion of bile salts will induce the appearance of choleric diarrhea, because of the direct toxic action of the bile salts on the colonic mucosa. Another factor that perpetuates the diarrheal process is related to the lack of regeneration of the intestinal mucosa morphology. persistent diarrhea
Pathophysiology o o o 13 Patients with ersistent diarrhea have important abnormalities in the mucosa of the small intestine. Total extension of the mucosa, the height of the villus or the villuscrypt relation are significantly decreased in the group of patients in whose feces EPEC was isolated, in relation to the control group. Transmission electron microscopy (TEM), showed several structural alterations, specially the flattening of microvilli, besides the increased number of multivesicular bodies and the vacuolization of mitochondria and of the endoplasmic reticulum. Tissue lesions, such as the increased thickness of the enterocytes basal lamina and of the vases endothelium, as well as the deposit of collagen in lamina propria. At scanning electron microscopy, intense and unspecific to the enteropathogenic agent lesions were demonstrated, such as decrease of the number and size of microvilli, structural disarrangement of enterocytes, and, in half of the cases, presence of mucous material covering part of the epithelium. Besides, due to some level of incapacity on the host’s part to keep the mechanisms that regulate the bacterial flora effective, a bacterial overgrowth may occur in the superior portions of the small intestine. The synergic actuation of all these pathophysiologic factors becomes responsible for the perpetuation of the diarrheal process and for the aggravation of the nutritional state, if therapeutic measures are not taken. persistent diarrhea
Is persistent diarrhea a serious problem? o o o 14 In 8 community based studies in Asia and Latin America (see table 1), persistent diarrhoea accounted for between 3 per cent and 23 per cent of all cases of diarrhoea. In 7 studies (see table 2) the incidence of persistent diarrhoea varied greatly. For every 100 children aged 4 years or less, 7 cases of persistent diarrhoea were seen per year in India, and 150 cases in northeastern Brazil. In all studies the incidence was much higher in children under 2 years than in older children. Persistent diarrhoea may account for a large proportion of all deaths due to diarrhoea. Although findings from some studies indicate that persistent diarrhoea most often occurs in children below 2 years of age, most persistent diarrhoeal deaths occur in children aged 1 to 4 years old when malnutrition is most common, because deaths from persistent diarrhoea are frequently associated with malnutrition. WHO and UNICEF estimated that in 1991 persistent diarrhoea accounted for only 10 per cent of diarrhoeal episodes, but as many as 35 per cent of diarrhoeal deaths in children under 5 years of age. Evidence from studies in Bangladesh, India, Peru and Brazil indicated that approximately 45 per cent (range 23 per cent to 62 per cent) of diarrhoea associated deaths were due to persistent diarrhoea. persistent diarrhea
Lethality o the risk of mortality because of acute diarrhea increases significantly along the duration of the disease much more important cause of morbidity and mortality than the acute one, mainly after the introduction of an oral rehydration therapy the identification of risk factors 15 persistent diarrhea o o

Lethality o o 16 Persistent diarrhea occurred in more than 62% of the deaths for diarrhea in Brazil, 47% in India, 36% in Senegal, and 26% in Bangladesh. These findings are probably due to the low rates of mortality for acute diarrhea in countries that use oral rehydration therapy (ORT) largely. Faveau et al. Demonstrated that 49% of the deaths for diarrhea presented association between persistent diarrhea and malnutrition. observation, out of the total number of deaths for diarrhea among children with less than 1 year of age, persistent diarrhea was responsible for 62% of the dysfunctions, while 28% were due to acute diarrhea, and 10% to “dysentery”. In this study, the authors suggested that infections acquired during hospitalization would be associated with 2/3 of the fatal cases, and reinforced the importance of the protector role of motherly suckling. In 1995, in Kenya, the percentage of death among children with persistent diarrhea was of 31. 7%. In 1998, in Brazil, Andrade et al. analyzed the risk factors to death among children with persistent diarrhea. In this study, 189 children hospitalized because of persistent diarrhea were evaluated, out of which 21 (11. 1%) died. The factors that showed a significant association with death were: 6 months of age or less, provenance from other hospitals, dehydration of III degree during hospitalization, presence of classic enteropathogenic Escherichia coli (EPEC) in the feces and the use of total parenteral nutrition (TPN). Systemic infection was considered the most important probable cause of death among infants hospitalized with persistent diarrhea
What causes persistent diarrhoea? o o o 17 Most cases of persistent diarrhoea seem to be associated with the same pathogens that cause acute diarrhoea. Four studies in India, Bangladesh and Peru found that rotavirus. Aeromonas, Campylobacter, Shigella and Giardia lamblia were equally common in acute and persistent diarrhoea. Cryptosporidium was more common in persistent than acute diarrhoea in Bangladesh, but the reverse was true in Peru. Evidence from several studies suggests that the entero-adherent Escherichia coli (so called because of their ability to adhere to intestinal cells in tissue culture) may be particularly associated with persistent diarrhoea. However. these organisms may be responsible for only a small proportion of all episodes. Even though most pathogens seem to be equally common at the onset of acute episodes that do or do not become persistent, different pathogens are found if cultures are taken from the same individual during the course of persistent diarrhoea. Studies in Bangladesh and Peru showed that it was not common to find the same pathogen in samples taken at different times during a persistent episode. The current evidence therefore suggests that no single pathogen is responsible for the persistence of episodes. Moreover, successive infections with different pathogens often occur in children with persistent diarrhoea. persistent diarrhea
What increases the risk of persistent diarrhoea? o o o Previous diarrhoea infection A relatively small proportion of children have many episodes of diarrhoea, and it is predominantly these children who develop persistent diarrhoea. This observation is supported by studies which show that a recent diarrhoeal illness is often associated with the occurrence of persistent diarrhoea. More studies are required to find out whether these, high-risk children are in an environment where there is greater transmission of enteric pathogens, or if they have greater susceptibility to illness. Studies are also needed to find out if the frequency of diarrhoea infections affects the child's immune status and ability to resist subsequent infection. Nutritional status Malnutrition is strongly associated with persistent diarrhoea. Researchers have found a small increased risk of diarrhoea incidence in malnourished children, but a large increased risk of prolongation of the episode. In Bangladesh, for example among persistent diarrhoea deaths, 81 per cent were associated with malnutrition. These findings suggest that malnutrition significantly increases the risk of dying in children suffering from persistent diarrhoea. Other factors These include deficiency of vitamin A, zinc, iron and other micronutrients; behaviours related to water source and use, food preparation and consumption and hygiene; presence of other diseases such as measles; suppression of immunity; and the interaction of these factors. 18 persistent diarrhea
Clinical aspects o o o 19 In general, the clinical characteristics of patients with persistent diarrhea do not vary significantly according to the causative agent. Most of the times, these children did not receive motherly suckling or were weaned very early. The diarrheal status is similar to the acute episode, but it is associated with the malabsorption syndrome, which, if not controlled with an adequate dietetic management, leads to malnutrition and its fatal consequences. Among them, we emphasize a higher vulnerability of the immunological capacity, favoring the installation of infectious processes Persistent diarrhea that may disseminate systematically, causing a high life risk. With repeated diarrheal episodes or with the persistence of them, the nutritional damage gets aggravated. This phenomenon becomes more serious when the nutritional support remains deficient in the convalescence phase, what usually happens due to anorexia and inadequate realimentation practices. Persistent diarrhea seems to represent the final result of a variety of insults to a child who is predisposed to frequent and serious episodes of diarrhea because of a combination between the host’s factors and environmental contamination. As a consequence, all the efforts have to be done in the sense of treating the diarrheal episodes efficiently, with an adequate follow-up. persistent diarrhea
Principles for Treatment of persistent diarrhoea o o 20 Appropriate fluids to prevent or treat dehydration A nutritious diet that does not cause diarrhoea to worsen Supplementary vitamins and minerals, including zinc for 10 - 14 days Antimicrobial(s) to treat diagnosed infections persistent diarrhea
The objective of treatment is to restore weight gain and normal intestinal function. Children who have persistent diarrhoea and severe malnutrition should be treated in hospital. 21 persistent diarrhea
Notice o Antimotility drugs (codeine, paregoric, tincture of opium, diphenoxylate and loperamide) have serious side effects and should not be used. Adsorbants such as kaolin, smectite and charcoal are also unlikely to be effective. 22 persistent diarrhea o

Diagnosis o o o 23 In 1989, Kleinman et al. suggested that the malabsorption syndrome and malnutrition are common factors of persistent diarrhea. Malabsorption was defined as the presence of nutrients in the feces, followed by loss or insufficient gain of weight, with an appropriate to the age diet. The authors proposed several tests to evaluate the absorption of many nutrients of the diet, and concluded that, in order to judge the efficacy of a determined formula, it is necessary to measure the serum levels of the various elements of the diet, and, mainly, to monitor the retaking of pondered gain during the adequate caloric offer. persistent diarrhea
Where to give treatment? o o o 24 Most children with persistent diarrhoea can be treated at home with careful follow-up to ensure they are improving. Some, however, require treatment in hospital, at least until their condition is stable, their diarrhoea has lessened and they are gaining weight. As the risk of nutritional decline and death in such children is high, every effort should be made to persuade parents that treatment in hospital is necessary. persistent diarrhea
Indication of Hospitalization in Persistent Diarrhea o o o 25 Children with a serious systemic infection, such as pneumonia or sepsis Children with signs of dehydration Infants below 4 months of age persistent diarrhea

Treatment The same general principles apply for treating acute diarrhoea can extrapolate to persistent diarrhoea. Stool losses should be replaced with appropriate fluids, feeding should be continued and unnecessary medicines avoided. Dietary management is especially important in persistent diarrhoea because of the association of persistent diarrhoea with malnutrition, lactose intolerance and (probably) micronutrient deficiency, and because the diet of children with persistent diarrhoea should be modified so that the intake of animal milk is reduced. o o o 26 persistent diarrhea
Oral Rehydration Therapy o o 27 As with acute diarrhoea, giving ORT during a persistent diarrhoea episode is the best way to prevent dehydration. The principle of replacing water and electrolyte losses is well established for acute diarrhoea and is no different for persistent diarrhoea. The aim of treatment is to replace initial and ongoing fluid losses until the diarrhoea stops. In nearly all cases of persistent diarrhoea ORT is all that is required for fluid replacement. persistent diarrhea
Prevent or Treat Dehydration • • • 28 Assess the child for signs of dehydration and give fluids according to Treatment Plan A, B or C, as appropriate. ORS solution is effective for most children with persistent diarrhoea. In a few, however, glucose absorption is impaired and ORS solution is not as effective as usual. When such children take ORS solution, stool volume increases markedly, thirst increases, signs of dehydration develop or worsen, and the stool contains a large amount of unabsorbed glucose. These children require IV rehydration until ORS solution can be taken without causing diarrhoea to worsen. persistent diarrhea
Dietary Management The association between persistent diarrhoea and malnutrition means that appropriate feeding is very important during and after the diarrhoea episode. . 29 persistent diarrhea
Therapeutical management o o 30 The objective of the treatment is to restore the hydroelectrolytic deficits and to restitute the fecal losses until the diarrheal process ceases. In almost all of the cases, this is possible through oral rehydration and early realimentation, using an appropriate dietetic scheme. Concerning the type of alimentation, the risks involving the use of parenteral feeding are known, specially in developing countries. Parenteral feeding shall be left as a last resource, in those patients with multiple alimentary intolerance, even to monosaccharides. As a consequence, most part of the recent studies on nutritional intervention during persistent diarrhea have focused the importance of the use of enteral feeding. In developed countries, there is a wide range of formulas commercially prepared, but their number is limited in third world countries, where these formulas are also very expensive. Thus, it is necessary to select provisions that are of easy digestion, proportionate an adequate nutritional support, have low cost and are hypoallergenic and of easy acceptance. WHO proclaims a nutritional therapy with cheap and available provisions, containing mineral and vitamin supply (WHO, 1996). Vitamin A, other micronutrients, such as folic acid, iron and B 12 vitamin, for its action on the intestinal mucosa and on the immune response, should be given to patients with persistent diarrhea
High calorie diet in PD o o o 31 Roy et al. , in 1998, emphasize that zinc supplementation in children with persistent diarrhea decreases significantly the recuperation time among underfed children, preventing the loss of weight and the decrease of serum concentrations of zinc. In general, underfed children with persistent diarrhea should receive an initial caloric offer of at least 75 kcal/kg/day, which should be increased in 25 kcal/kg/day, until it reaches 250 kcal/kg/day. The lesion in the intestinal mucosa present in the persistent diarrhea leads to lactase deficiency, incapacitating the hydrolysis of lactose into glucose and galactose. persistent diarrhea
Treatment o o 32 The use of lactose-free formulas reduces the duration of diarrheal processes in inpatients. So, the initial dietetic treatment for persistent diarrhea cases in developing countries is based on the use of lactose-free formulas. Bhutta & Hendricks suggest the use of diets based on cereals or vegetables, such as the rice formulas, which should be prepared with the addition of vegetal oil in order to increase the caloric offer. In the impossibility of achieving the adequate caloric and protean offer, these authors suggest the use of sour milk as a complement. Though, a substantial proportion of children do not respond to this dietetic proposal, and should be investigated in relation to other alterations, such as intolerance to monosaccharides and allergy to proteins of the diet. The presumptive diagnosis of alimentary allergy is carried out with suppression and provocation tests using the mentioned proteins, specially the cow milk protein. Harrison, in 1974, and Lyngkaram, 60 in 1978, emphasized the importance of the intolerance to cow milk protein in the perpetuation of the diarrheal process. In these cases, formulas free from the aggressive protein are necessary. Some alternatives may be used when protein hydrolyzates are not available. Human milk proceeding from the milk bank showed to be efficacious when used by Mc. Farlane & Miller in the treatment of children with persistent diarrhea. In spite of the consensus that the soybean protein may be the cause of alimentary allergy, some studies have shown good results with the use of soybean formulas in the treatment of these pathology. Other authors published studies reporting good results with the use of chicken formulas in the treatment of children with prolonged diarrhea. persistent diarrhea
Antibiotic Treatment in PD o o 33 Clinical experiences with the use of antimicrobials in patients with persistent diarrhea are limited. In a casecontrol study carried out in South Africa, using oral gentamicin, metronidazole and cholestyramine in patients with persistent diarrhea, the use of oral gentamicin showed a significant decrease in the fecal losses, what did not happen with metronidazole. Bahl et al. , in 1996, did not find any benefic effect with the use of metronidazole in persistent diarrhea episodes that were not dysenteric and not associated with giardiasis and amebiasis. Alam et al. , in 1995, using sulfamethoxazoletrimethoprim in patients with persistent diarrhea, showed a decrease in the fecal volume, a shorter duration of the diarrhea and a higher rate of recuperation within 7 days of treatment, besides a probable protector role concerning the occurrence of hospital infections in relation to the control group. Our experience along 25 years has shown clearly that the use of antibiotics and/or any other medicine in a routine way does not have any benefic action regarding the control of diarrhea. On the other hand, emphasis on the nutritional support, respecting the needs of each patient and using formulas that fulfill the digestive-absorptive needs and Persistent diarrhea capacities, preferably those with a protein hydrolyzate base, through oral or enteral feeding, represents the basic pillar in the exit regarding clinical recuperation of the patient with persistent diarrhea
Prophylaxis o 34 the incentive to the exclusive motherly suckling persistent diarrhea
Older infants and young children o o Use standard diets prepared from local ingredients. Two diets are described below; • The first contains reduced lactose. • The second, for children who do not improve with the first, contains no lactose and reduced starch. 35 persistent diarrhea
(a) Reduce lactose by decreasing the amount of nonhuman milk in the diet Persistent diarrhoea is less common in children who are breastfed than in those who are given cow's milk or other non-human milks. Lactose intolerance occurs especially in children who are severely malnourished or who have severe diarrhoea. Lactose is a sugar providing about 35 to 45 per cent of the calories in non-human milks used for feeding children. Once in the gut, it must first be broken down by an intestinal enzyme called lactase, before it can be absorbed by the gut wall cells. During the early phase of a diarrhoeal episode lactase production may decline, slowing down digestion of lactose. If the sick child continues to ingest milks containing lactose, any undigested lactose passes into the lower intestine, where it can draw fluid from the gut wall cells into the intestinal lumen, thereby increasing the severity of diarrhoea. Fortunately, clinically significant lactose intolerance occurs in only a very small proportion of children with acute diarrhoea. In a child with persistent diarrhoea, adverse effects can usually be avoided by reducing lactose intake to about 2 to 3 g/kg/day (about 30 to 50 ml/kg/day of whole cow's milk) and mixing the milk with cereal. Replacement of cow's milk by fermented milk products. such as yoghurt, which contains less lactose, is another way to reduce the intake of lactose. o o 36 persistent diarrhea
The First Diet (Reduced lactose) o o o 37 This should be started as soon as the child can eat and should be given six times a day. Many children will eat poorly, however, until any serious infection is treated for 24 -48 hours. Such children may require nasogastric feeding initially. The diet should contain at least 70 Kcal/100 g, provide milk or yoghurt as a source of animal protein, but no more than 3. 7 g lactose/kg body weight/day, and provide at least 10% of calories as protein. A mixture of cow's milk, cooked cereal, vegetable oil and cane sugar is satisfactory. Diets can also be prepared from local ingredients following the above guidelines. persistent diarrhea

(b) Ensure that the child receives enough nutritious food o o o Appropriate feeding is very important during and after a persistent diarrhoea episode. A second essential aspect of the dietary management of persistent diarrhoea is to make sure that adequate food intake is maintained. As most children with persistent diarrhoea are cared for in the community by the family recommendations for dietary management should be based on foods that are inexpensive, readily available, culturally acceptable, and easy to prepare in the home. Special diets, such as formula milks that are free of cow's milk or lactose, are too expensive for most families in developing countries, and are rarely needed. 38 persistent diarrhea
The second diet (lactose-free with reduced starch) o o o 39 About 65% of children will improve on the first diet. Of those who do not, more than half will improve when given a second diet prepared from egg, cooked cereal, vegetable oil and glucose, and providing at least 10% of calories as protein. If finely ground, cooked chicken meat (12 g) is used in place of whole egg, the diet provides 70 Kcal per 100 g. persistent diarrhea
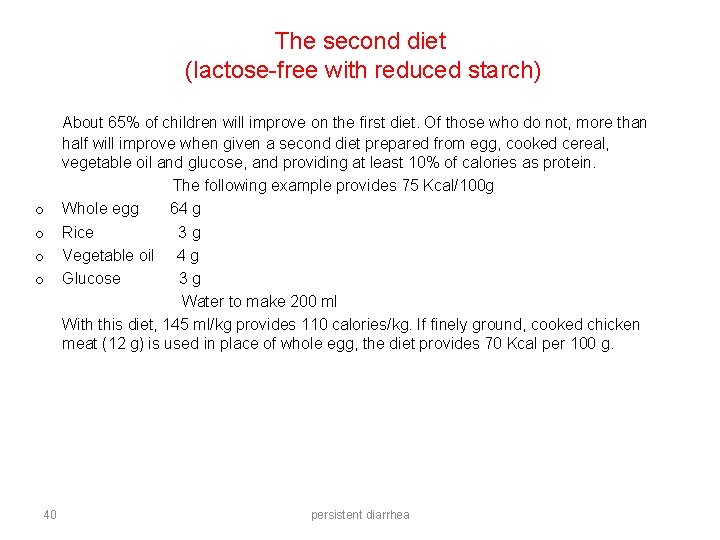
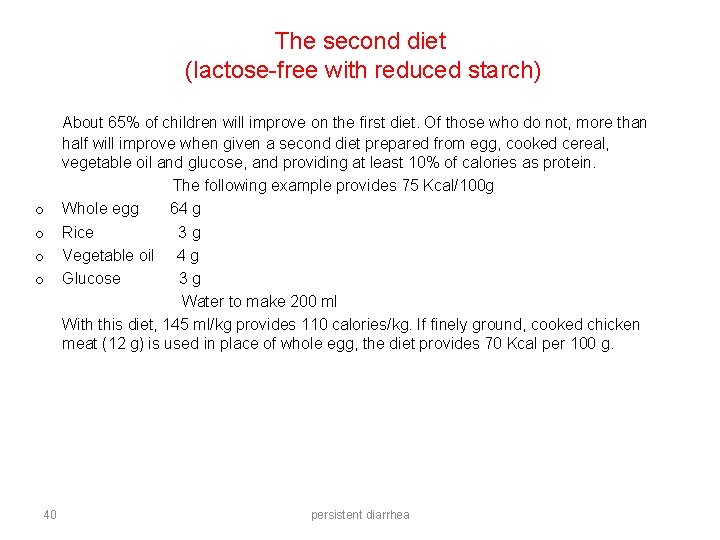
The second diet (lactose-free with reduced starch) o o 40 About 65% of children will improve on the first diet. Of those who do not, more than half will improve when given a second diet prepared from egg, cooked cereal, vegetable oil and glucose, and providing at least 10% of calories as protein. The following example provides 75 Kcal/100 g Whole egg 64 g Rice 3 g Vegetable oil 4 g Glucose 3 g Water to make 200 ml With this diet, 145 ml/kg provides 110 calories/kg. If finely ground, cooked chicken meat (12 g) is used in place of whole egg, the diet provides 70 Kcal per 100 g. persistent diarrhea
Local diet o o o 41 Recent studies have shown that both acute and persistent diarrhoea can be successfully managed with diets based on local staple foods. But the diet for those with persistent diarrhoea should have the animal milk content reduced or mixed with other foods. A multi-centre study to evaluate a treatment scheme for persistent diarrhoea using local foods is now underway in six countries. These studies are based on the principle of reducing the proportion of lactose in diets to treat persistent diarrhoea. Children in Pakistan are given a diet of khitchri (rice and lentils cooked with oil) with yoghurt: children in Peru, India, Vietnam and Bangladesh are given a rice-milk diet; and children in Mexico are given a maize-milk diet. Children who do not recover on the initial diet are switched to a second diet, which contains no milk, such as one diet based on rice mixed with a protein source, for example chicken or egg white. persistent diarrhea
Drugs o o 42 Antibiotics should not be used in persistent diarrhoea except for certain specific pathogens. Shigella is known to cause persistent diarrhoea and can be treated with antibiotics: antibiotics should be used when Shigella is isolated by stool culture or when the stool is bloody. Non-specific antibiotic therapy, given without knowing what is causing the diarrhoea episode, has not proved to be effective against persistent diarrhoea and should not be used. Cholestyramine and bismuth subsalicylate have shown benefit in some studies, but are not recommended for routine use. persistent diarrhea

Identify and treat specific infections o o o 43 Routine treatment of persistent diarrhoea with antimicrobials is not effective and should not be given. Some children, however, have non-intestinal (or intestinal) infections that require specific antimicrobial therapy. The persistent diarrhoea of such children will not improve until these infections are diagnosed and treated correctly. persistent diarrhea

Non-intestinal infections Every child with persistent diarrhoea should be examined for non-intestinal infections, such as: o Pneumonia o Sepsis o Urinary tract infection o Otitis media 44 persistent diarrhea
Intestinal Infections o o o 45 Persistent diarrhoea with blood in the stool should be treated with an oral antimicrobial effective for Shigella. Treatment for amoebiasis should be given only if the diagnostic criteria. Treatment for giardiasis should be given only if cysts or trophozoites of G. duodenalis are seen in the faeces. persistent diarrhea
Hospital-acquired Infections o o o Serious infections are often acquired in hospital. These may include pneumonia, rotavirus diarrhoea and cholera, among others. Hospital-acquired infection should be considered in any child who is lethargic and eats or drinks poorly (but is not dehydrated), or who develops fever, cough, worsening diarrhoea or other signs of serious illness at least two days after being admitted. 46 persistent diarrhea
Give a nutritious diet o o o 47 This is essential treatment for all children with persistent diarrhoea. As the normal diet of such children is often inadequate, their treatment provides an important opportunity to teach their mothers how to feed them correctly. Outpatients should be given a diet appropriate for their age, but with a limited content of lactose. Children treated in hospital require special diets until their diarrhoea lessens and they are gaining weight. In either situation, the goal is a daily intake of at least 110 calories/kg. persistent diarrhea
Feeding of Outpatients o o o o o 48 Continue breastfeeding. If yoghurt is available, give it in place of any animal milk usually taken by the child; yoghurt contains less lactose and is better tolerated. Limit animal milk to 50 ml/kg/day; greater amounts may aggravate the diarrhoea. Mix the milk with the child's cereal. Do not dilute the milk. Give other foods that are appropriate for the child's age. Give enough energy intake. Infants older than 6 months whose only food has been animal milk should begin to take solid foods. Give frequent small meals, at least six times a day. persistent diarrhea
Infants below age 6 months o o o 49 If animal milk must be given, replace it with yoghurt (given with a spoon). Encourage exclusive breastfeeding. Help mothers who are not breastfeeding exclusively to re-establish lactation. If this is not possible, give a lactose free milk formula (given from a cup). persistent diarrhea
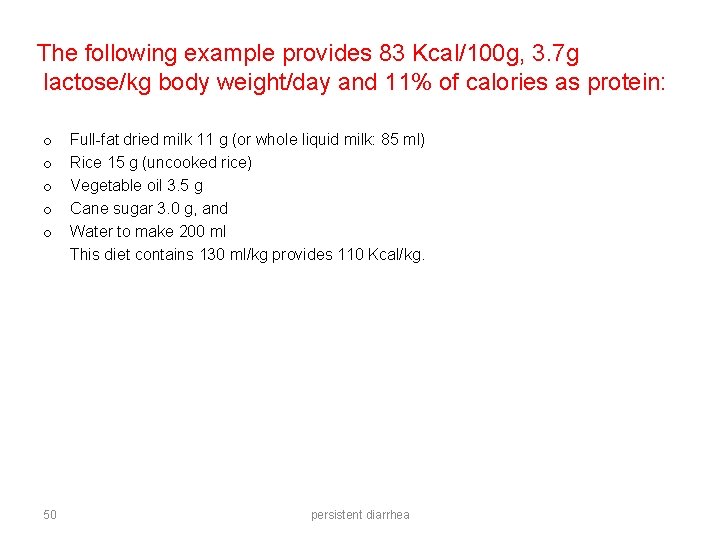
The following example provides 83 Kcal/100 g, 3. 7 g lactose/kg body weight/day and 11% of calories as protein: o o o 50 Full-fat dried milk 11 g (or whole liquid milk: 85 ml) Rice 15 g (uncooked rice) Vegetable oil 3. 5 g Cane sugar 3. 0 g, and Water to make 200 ml This diet contains 130 ml/kg provides 110 Kcal/kg. persistent diarrhea

Infants below age 6 months o o o 51 Encourage exclusive breastfeeding. Help mothers who are not breastfeeding exclusively to re-establish lactation. If animal milk must be given, replace it with yoghurt (given with a spoon). If this is not possible, give a lactose free milk formula (given from a cup). persistent diarrhea
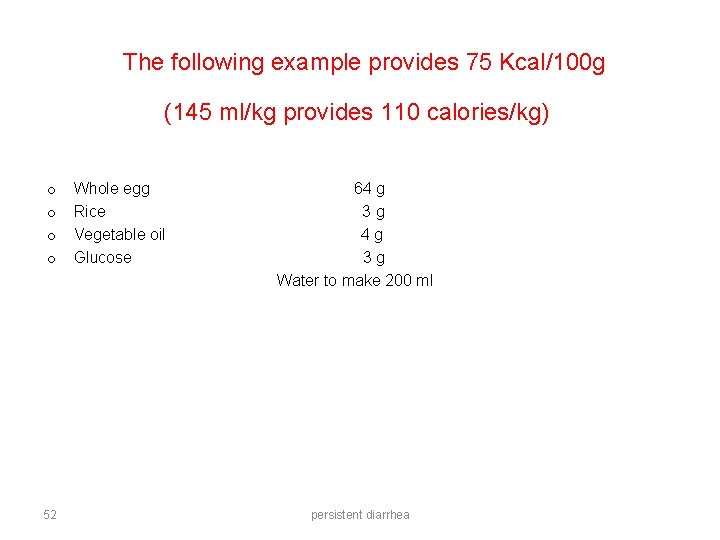
The following example provides 75 Kcal/100 g (145 ml/kg provides 110 calories/kg) o o 52 Whole egg Rice Vegetable oil Glucose 64 g 3 g 4 g 3 g Water to make 200 ml persistent diarrhea
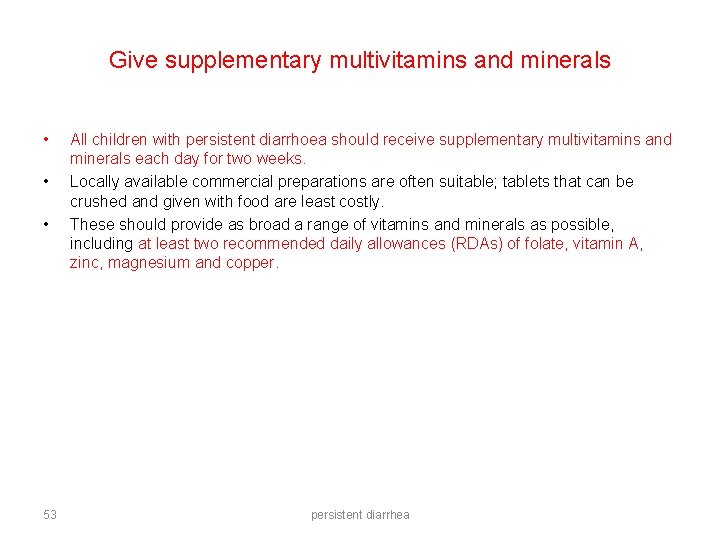
Give supplementary multivitamins and minerals • • • 53 All children with persistent diarrhoea should receive supplementary multivitamins and minerals each day for two weeks. Locally available commercial preparations are often suitable; tablets that can be crushed and given with food are least costly. These should provide as broad a range of vitamins and minerals as possible, including at least two recommended daily allowances (RDAs) of folate, vitamin A, zinc, magnesium and copper. persistent diarrhea
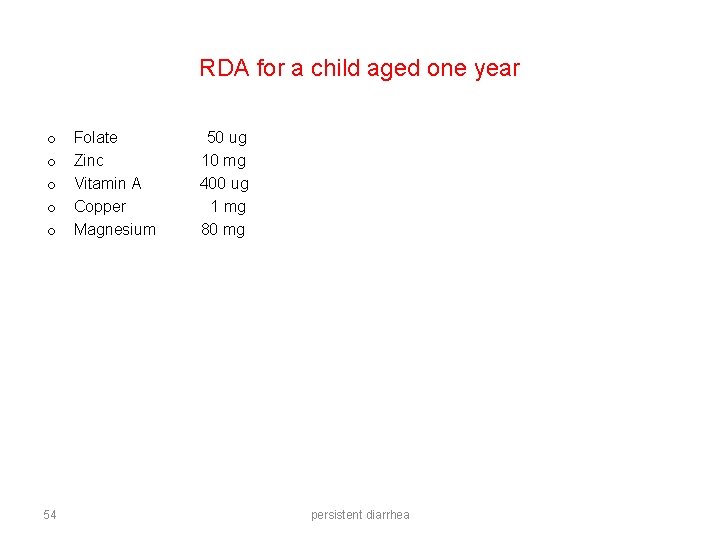
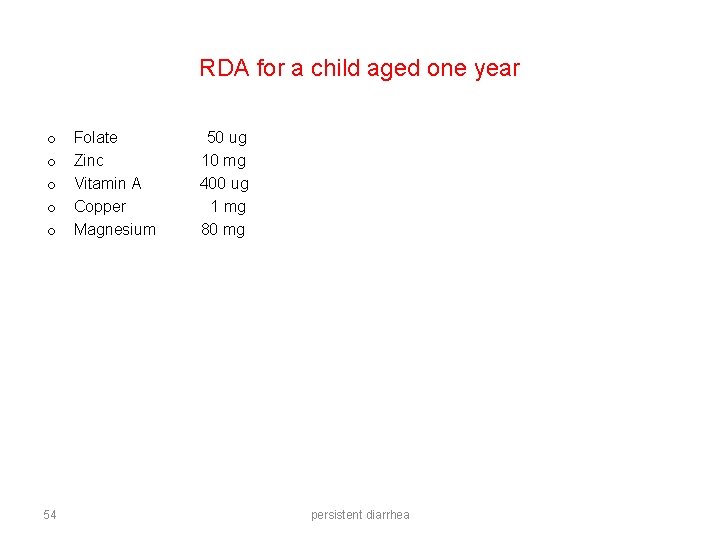
RDA for a child aged one year o o o 54 Folate Zinc Vitamin A Copper Magnesium 50 ug 10 mg 400 ug 1 mg 80 mg persistent diarrhea
Children treated in hospital o o 55 Many children will lose weight for 1 -2 days, and then show steady weight gain as infections come under control and diarrhoea subsides. There should be at least three successive days of increasing weight to conclude that weight gain is occurring; for most children, weight on day 7 will be greater than on admission. persistent diarrhea
The following should be measured and recorded in a standard manner, at least daily: o o 56 Body weight Temperature Food taken Number of diarrhoea stools persistent diarrhea
Successful treatment with either diet is characterized by: o o 57 Adequate food intake Weight gain Fewer diarrhoeal stools Lack of fever persistent diarrhea
Why treatment sometimes fails? o o o 58 Although 80 per cent of children with persistent diarrhoea may be managed with proper feeding and ORT, it is important to be able to identify children for whom such treatment is likely to fail or recovery may be delayed. In Pakistan treatment failure was more likely in younger children and those who were vomiting; delayed recovery was associated with younger age, malnutrition and severe watery diarrhoea. In Bangladesh children with more severe diarrhoea were also more likely to have delayed recovery. persistent diarrhea
Dietary Failure o o o 59 An increase in stool frequency (usually to more than 10 watery stools/day), often with a return of signs of dehydration; this usually occurs shortly after a new diet is begun; or a failure to establish daily weight gain within seven days. The first diet should be given for seven days, unless signs of dietary failure occur earlier, in which case the first diet should be stopped and the second diet given, also for seven days. Children responding satisfactorily to either diet should be given additional fresh fruit and well cooked vegetables as soon as improvement is confirmed; after seven days' treatment with the effective diet, they should resume an appropriate diet for age, including milk, that provides at least 110 Kcal/kg/day. Occasionally it is necessary to restrict milk intake for more than seven days. Children may return home, but should be followed up regularly to ensure continued weight gain and compliance with feeding advice. persistent diarrhea
Children treated as outpatients o o o 60 Children should be re-evaluated after seven days, or earlier if diarrhoea worsens or other problems develop. Those who have gained weight and who have less than three loose stools per day, may resume a normal diet for age. Those who have not gained weight or whose diarrhoea has not improved should be referred to hospital. persistent diarrhea
Key issues for future research o o o 61 Although many aspects of the development of persistent diarrhoea are unclear its strong association with malnutrition and high incidence and fatality rates in developing countries, suggest that it deserves much more attention. Locally available diets that can be used for initial treatment and for treatment failures, so that practical treatment schemes can be developed in different settings. The role of immune factors in the persistence of some episodes and the recovery from diarrhoea. The role of micronutrients in treating persistent diarrhoea and improving growth. Care-seeking behavior during acute and persistent phases of diarrhoea, and the relationship of care-seeking and treatments used to the outcome of the episode. persistent diarrhea
THE END 62 persistent diarrhea