1 Medicare Cost Report 101 WHAT YOU REALLY

- Slides: 36
1 Medicare Cost Report 101 WHAT YOU REALLY NEED TO KNOW
2 Presented by Bill Emrhein President 440. 243. 6020 bill. emrhein@emrheinandassociates. com
3 Medicare Cost Report Purpose All Medicare certified institutional providers are required to file an annual cost report to their respective Medicare Administrative Contractor (MAC). The cost report is a summary of a provider’s activities for the fiscal period. Consists of a series of forms that collect descriptive, financial, and statistical data.
4 Medicare Cost Report Purpose Provides Centers for Medicare & Medicaid Services (CMS) the basis for future rate setting and gives lawmakers data to make policy decisions. The cost report is utilized to set prospective payment rates such as: Ø Wage Index Ø Disproportionate Share Hospital (DSH) adjustment Ø Indirect Medical Education (IME)/Graduate Medical Education (GME) Ø Outliers
5 Medicare Cost Report Purpose Determines Qualification for the 340 B Drug Pricing Program Determines whether Medicare over or underpaid the provider for services provided to Medicare patients. Gives the provider an opportunity to claim additional reimbursement from Medicare depending on certain criteria and current year activity. Used by external sources such as Medicaid and Worker’s Comp
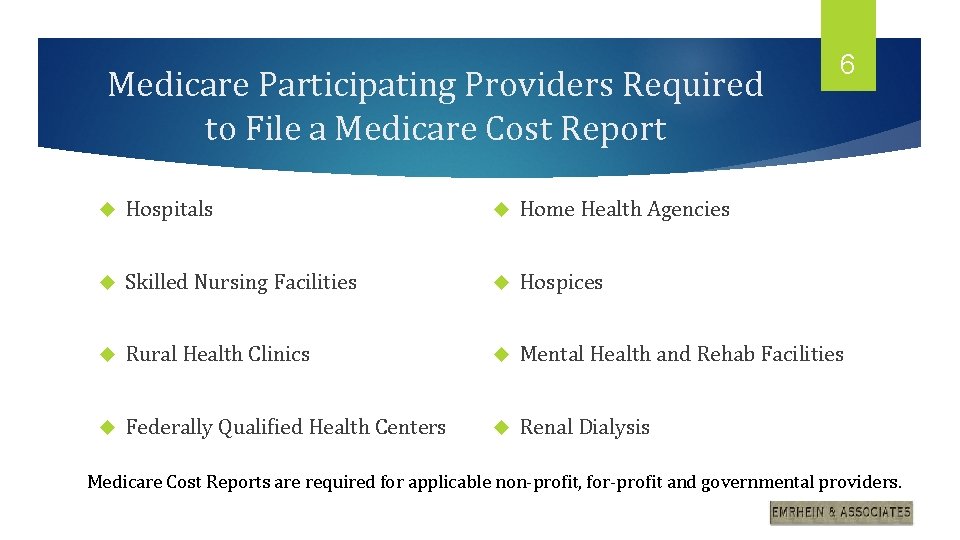
Medicare Participating Providers Required to File a Medicare Cost Report 6 Hospitals Home Health Agencies Skilled Nursing Facilities Hospices Rural Health Clinics Mental Health and Rehab Facilities Federally Qualified Health Centers Renal Dialysis Medicare Cost Reports are required for applicable non-profit, for-profit and governmental providers.
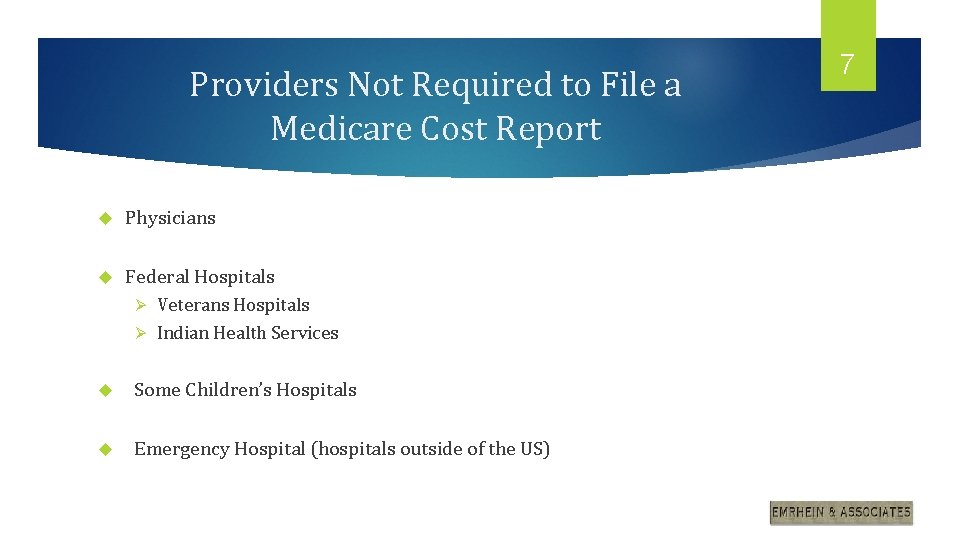
Providers Not Required to File a Medicare Cost Report Physicians Federal Hospitals Veterans Hospitals Ø Indian Health Services Ø Some Children’s Hospitals Emergency Hospital (hospitals outside of the US) 7
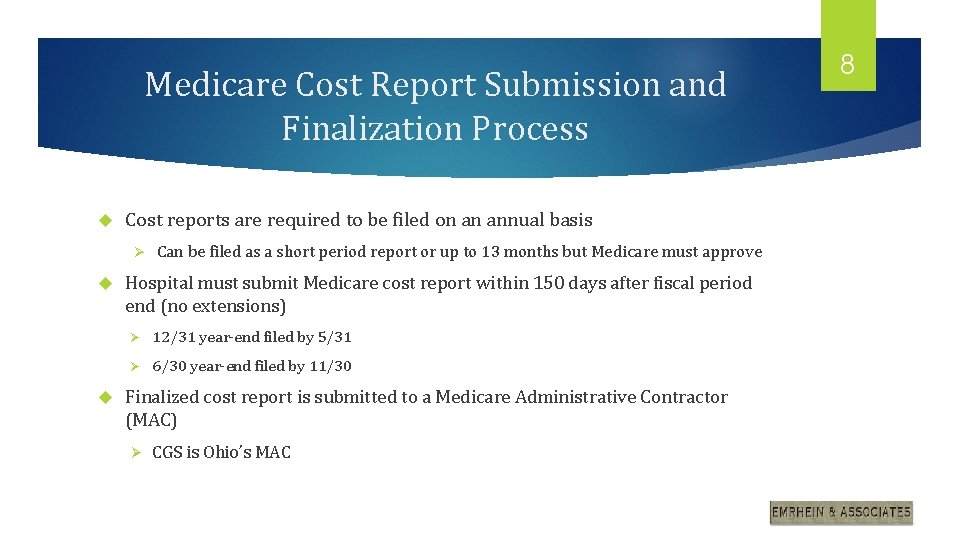
Medicare Cost Report Submission and Finalization Process Cost reports are required to be filed on an annual basis Ø Can be filed as a short period report or up to 13 months but Medicare must approve Hospital must submit Medicare cost report within 150 days after fiscal period end (no extensions) Ø 12/31 year-end filed by 5/31 Ø 6/30 year-end filed by 11/30 Finalized cost report is submitted to a Medicare Administrative Contractor (MAC) Ø CGS is Ohio’s MAC 8
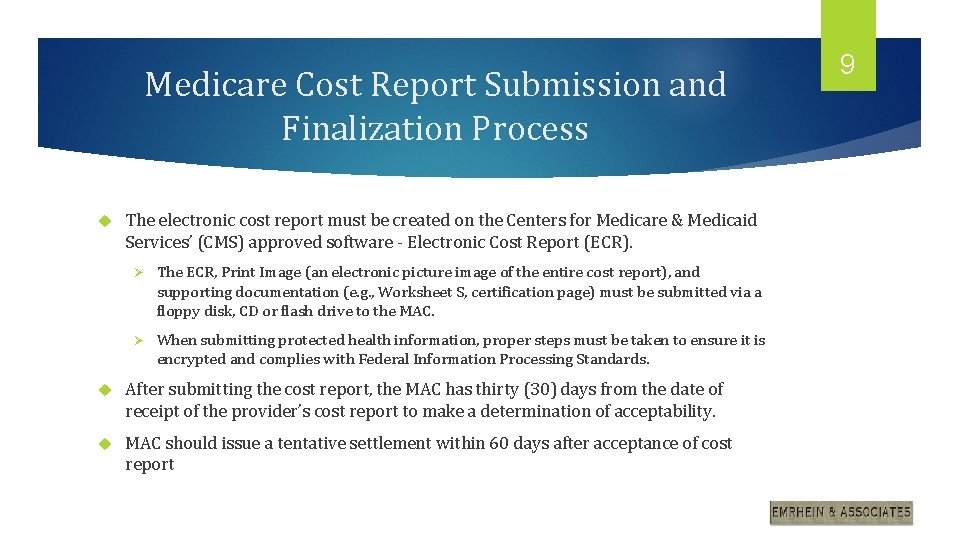
Medicare Cost Report Submission and Finalization Process The electronic cost report must be created on the Centers for Medicare & Medicaid Services’ (CMS) approved software - Electronic Cost Report (ECR). Ø The ECR, Print Image (an electronic picture image of the entire cost report), and supporting documentation (e. g. , Worksheet S, certification page) must be submitted via a floppy disk, CD or flash drive to the MAC. Ø When submitting protected health information, proper steps must be taken to ensure it is encrypted and complies with Federal Information Processing Standards. After submitting the cost report, the MAC has thirty (30) days from the date of receipt of the provider’s cost report to make a determination of acceptability. MAC should issue a tentative settlement within 60 days after acceptance of cost report 9
Medicare Cost Report Submission and Finalization Process MAC will examine the cost report and determine the scope using one of the following two levels : Ø Desk Review Ø Field Audit Once the MAC has completed a review of the cost report they will provide an audit adjustment report to the hospital for review Ø It is important to review and challenge audit adjustments as necessary 10
Medicare Cost Report Submission and Finalization Process MAC will issue a Notice of Program Reimbursement (NPR) with the final settlement amount when they complete their work. If the provider is dissatisfied with the NPR, the provider may appeal to the Provider Reimbursement Review Board (“PRRB”), an independent panel, within 180 days of the receipt of the NPR. A cost report may be reopened by the provider, MAC or CMS if a written request is received within three (3) years of the date that the NPR was issued. A provider’s request for a cost report final determination reopening may be honored by the MAC if: Ø new and material evidence has been submitted Ø a clear and obvious error was made Ø the determination is found to be inconsistent with the law, regulations and rulings, or general instructions 11
12 Medicare Cost Report Fundamentals Medicare cost report groups expenses, revenue and statistics by specific categories/cost centers by inputting data into specified worksheets. Allocates support and overhead costs to patient care areas Calculates Medicare related cost Compares calculated Medicare reimbursement to actual Medicare payments paid on an interim basis Calculates final settlement
13 Medicare Cost Report Fundamentals Final Settlement – Acute PPS Hospitals Ø PPS reimbursement has no settlement on Part A and Part B claims. Ø Settlement generally includes differences between rates/payment set from a previous years filed cost report to current year totals. Ø Items usually impacting settlement: § Actual bad debts and allied health costs vs bi-weekly pass-through payments § Lump Sum payments/receipts § Medicare DSH percentage changes § Low Volume rate changes § Medical Education rate, PY I&R FTE and or bed changes § Hospital Specific rate changes (MDH/SCH)
14 Medicare Cost Report Fundamentals Final Settlement - Critical Access Hospital (CAH) Ø Reimbursement equals 101% of costs and there can be significant settlement fluctuations due to: § Expense or revenue fluctuations § Changes in ancillary service mix § Census increases or decreases § Hospital cost control issues § Medicare audit adjustments § Bad Debt vs Pass Through payments § Lump Sum payments/receipts
15 Medicare Cost Report Worksheets WS S Series – Settlement, questionnaire, statistics, days, discharges, wage index, and uncompensated care information WS A Series – Trial balance of expenses grouped by cost center WS B Series – Allocation of overhead expenses to routine, ancillary, and other departments WS C Series – Trial balance of revenue grouped by cost center and calculates cost/charge ratios WS D Series – Determines the reimbursable Medicare costs of treating Medicare patients
16 Medicare Cost Report Worksheets WS E Series – Determines the due to/from Medicare Program based on payments received WSG Series – Financial Statements summary WS H Series – Home Health Services WS I Series – Renal Dialysis WS M Series – Provider Based RHC WS N Series – Provider Based FQHC WS O Series – Hospice series
17 Worksheet S Series Certification and Settlement page (WS S) Ø Hospital senior executive signs report attesting that the cost report is filed in compliance with Medicare regulations Ø Summary of settlement Provider Identification (WS S-2 Part I) Ø Hospitals answer questions that determine the Reimbursement methodology (CAH, PPS) and the required worksheets to complete Ø Important to include all sub-providers and identify all add-on payments Ø Medicare DSH days
18 Worksheet S Series Provider Questionnaire (WS S-2 Part II) Ø Replaced the old CMS-339 form Ø Bad Debt listing and Physician time study summaries are generally filed separately Ø Used to identify items claimed on the cost report or changes that occurred between years § Bad debts § Bed changes § Capital changes
19 Worksheet S Series Provider Statistical Data (WS S-3 Part I) Ø Total and program (Medicare, Medicaid) days and discharges by nursing unit § Include Adults and Peds, ICU, Nursery, Sub providers, Home Health, and Hospice Ø Bed count and bed days available Ø CAH inpatient hours of care Ø Observation bed days Ø FTE count
20 Worksheet S Series PPS Hospital Wage Index Information (WS S-3 Part II, Part III, & Part IV) – N/A for CAHs Ø Total adjusted salaries (includes A-6 reclassifications) Ø Total paid hours (allowed to exclude some nonproductive hours) Ø Include all contract labor Ø Calculates average hourly rate used to set and calculate future reimbursement. Ø Amounts filed during cost report are tentative. Hospitals are allowed to review and adjust wage index amounts before they become final
21 Worksheet S Series – Wage Index Used to compare all hospitals in the nation and adjust Medicare DRG and APC payments by designated region Determines overall average hourly wage rate for each acute care hospital based on employee and contract labor average hourly wage and employee benefit costs Sources of information include: Payroll reports, salary, employee benefit and contract labor expenses and hours and contract labor hours from invoices or information provided by vendor Important to maximize and have comparable dollars and hours by department Separate wage index is performed annually by the MAC
22 Worksheet S Series Uncompensated Care Data (WS S-10) Ø Impacts Medicare DSH reimbursement Ø Calculates total unreimbursed and uncompensated care cost Ø Separates defined charity from bad debts for patients with and without insurance. Ø Requires patient payments separated from insurance payments Ø Excludes all professional fees and courtesy discounts from charity charges Ø Requires total bad debts Ø Requires Medicaid gross revenue, assessments and payments, net of professional fees (informational only) Ø Data sources: Charity care logs and patient financial reports
23 Worksheet S Series Other WS S Series Worksheets Ø WS S-4 Home Health Agency Statistical Data § Ø WS S-8 Rural Health Clinic/Federally Qualified Health Center Questionnaire § Ø Days, FTE’s, PPS Activity Clinic hours, Location, Federal Funds WS S-9 Hospice Identification Data § Unduplicated days by level of care and payor type
24 Worksheet A Series Starts with expenses by Medicare cost center Salary vs. Other Expense Mainly for wage index purposes Worksheet A Trial Balance of Expenses Worksheet A-6 Reclassifications of Expense Worksheet A-7 Analysis of Capital Assets & Capital-Related Costs Worksheet A-8 Adjustments to Expenses Worksheet A-8 -1 Statement of Costs of Services From Related Organizations and Home Office Costs Worksheet A-8 -2 Provider Based Physician Adjustments Worksheet A-8 -3 Reasonable Cost Determination for Therapy Services Furnished by Outside Suppliers (CAHs) Summary of : Reclasses – balances to zero Adjustments – costs added or removed
25 Worksheet A Series Worksheet A – Summary of trial balance expenses by department grouped by cost center Ø Worksheet A-6 - Reclassification of Trial Balance of Expenses (WS A) Ø Separates expenses by Salary and non Salary Reclassifies costs for proper matching Worksheet A-8 – Adjustments to Trial Balance of Expenses (WS A) Ø Ø Removes non-allowable costs § Non-patient revenue § Physician recruiting cost § Lobbying dues § Related party cost in excess of actual cost (WS A-8 -1) § Physician compensation for hospital services not supported by time allocation agreement or time study (WS A-8 -2) Adds costs not included in trial balance
26 Worksheet B Series COST ALLOCATION WS B SERIES Ø Medicare Cost Finding or Allocation Ø Allocates capital, administrative, support and teaching costs to patient care and non- reimbursable cost centers Ø Medicare approved allocation methods for each overhead cost center such as: § Square footage to allocate depreciation § Salaries to allocate employee benefits
27 Worksheet B Series Worksheet B Part I - Cost Allocation General Service Costs Worksheet B Part II - Allocation of Capital-Related Costs Ø Worksheet B - Provides for the allocation of operating and capital expenses of each general service cost (overhead) center to those cost centers which receive the services (patient care and non reimbursable cost centers). Worksheet B-1 - Cost Allocation-Statistical Bases Ø Provides for the proration of the statistical data needed to allocate the expenses of each general service cost center on Worksheet B -All statistics must be current, accurate and meet the tests of audit Ø Change in Cost Allocation Method § Must request 90 days prior to FYE and it is 3 year commitment § Must have a reason for the change other than “to increase Medicare reimbursement”
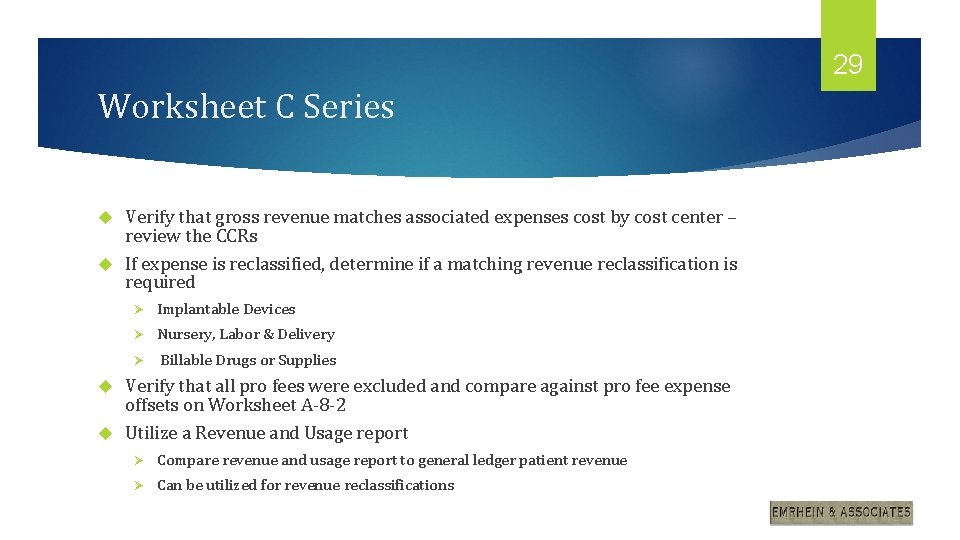
28 Worksheet C Series Worksheet C Computes the ratio of costs to charges (RCCs) for inpatient and outpatient ancillary services by cost center Using direct costs from worksheet A and allocated overhead costs from worksheet B, this schedule computes total cost by service line Input gross patient revenue by service line Cost to charge ratios (CCR/RCC) calculated and carried forward to Medicare cost apportionment worksheets (to D series Worksheets)
29 Worksheet C Series Verify that gross revenue matches associated expenses cost by cost center – review the CCRs If expense is reclassified, determine if a matching revenue reclassification is required Ø Implantable Devices Ø Nursery, Labor & Delivery Ø Billable Drugs or Supplies Verify that all pro fees were excluded and compare against pro fee expense offsets on Worksheet A-8 -2 Utilize a Revenue and Usage report Ø Compare revenue and usage report to general ledger patient revenue Ø Can be utilized for revenue reclassifications
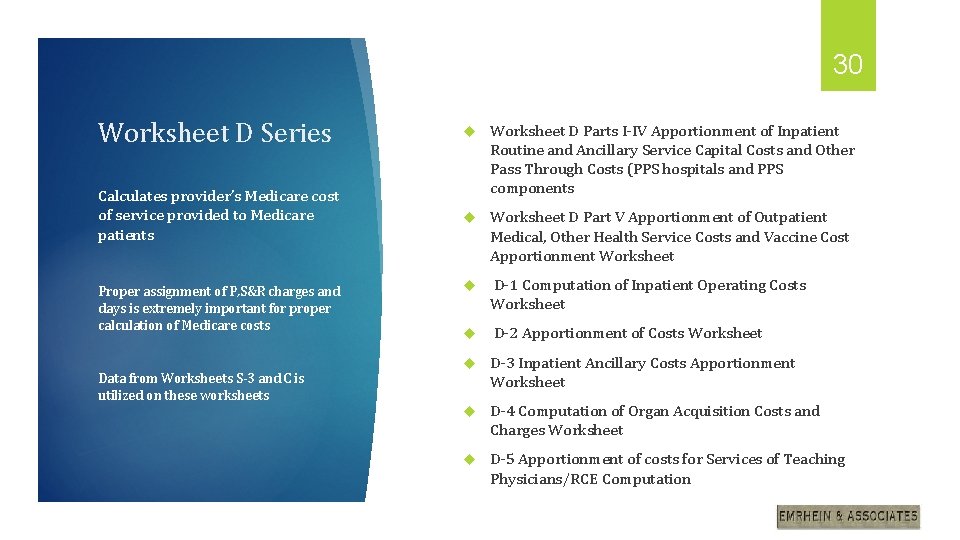
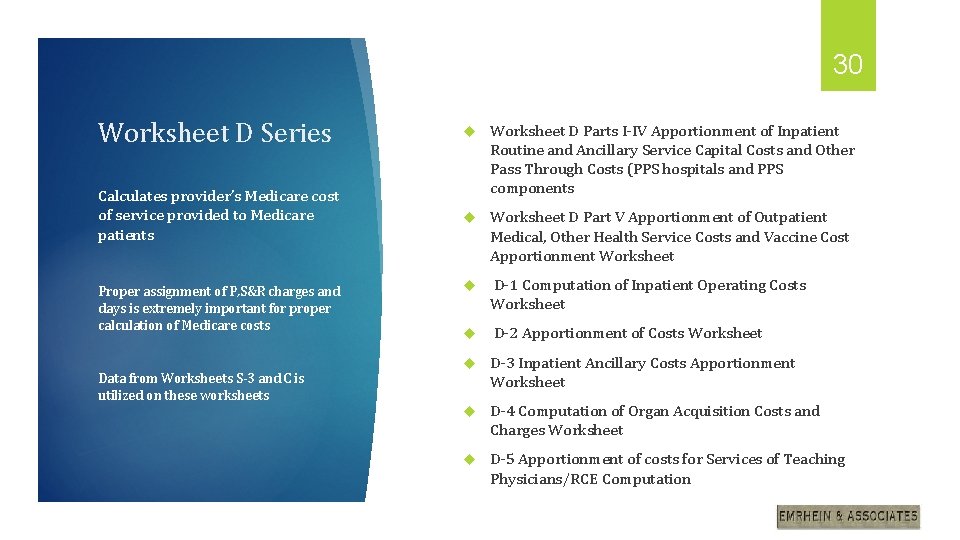
30 Worksheet D Series Calculates provider’s Medicare cost of service provided to Medicare patients Worksheet D Parts I-IV Apportionment of Inpatient Routine and Ancillary Service Capital Costs and Other Pass Through Costs (PPS hospitals and PPS components Worksheet D Part V Apportionment of Outpatient Medical, Other Health Service Costs and Vaccine Cost Apportionment Worksheet D-1 Computation of Inpatient Operating Costs Worksheet D-2 Apportionment of Costs Worksheet D-3 Inpatient Ancillary Costs Apportionment Worksheet D-4 Computation of Organ Acquisition Costs and Charges Worksheet D-5 Apportionment of costs for Services of Teaching Physicians/RCE Computation Proper assignment of P, S&R charges and days is extremely important for proper calculation of Medicare costs Data from Worksheets S-3 and C is utilized on these worksheets
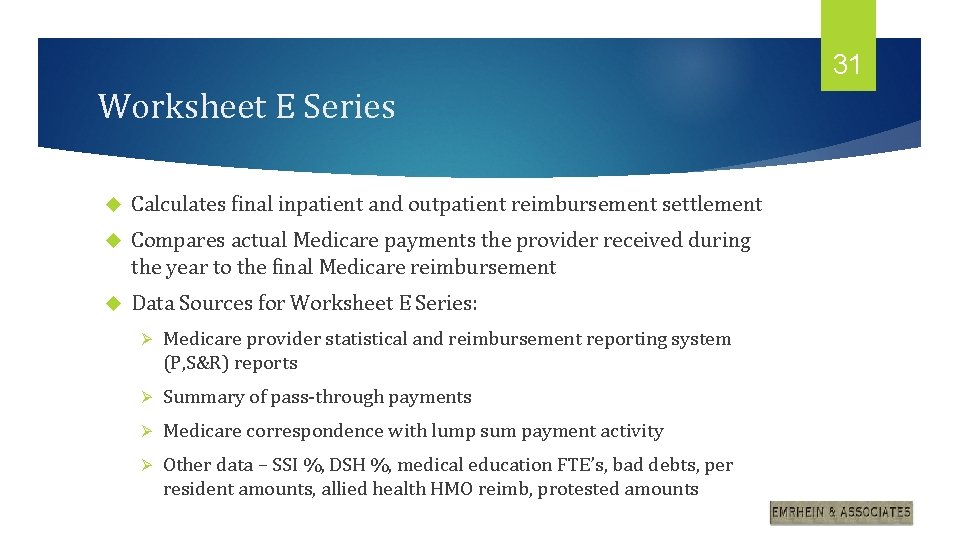
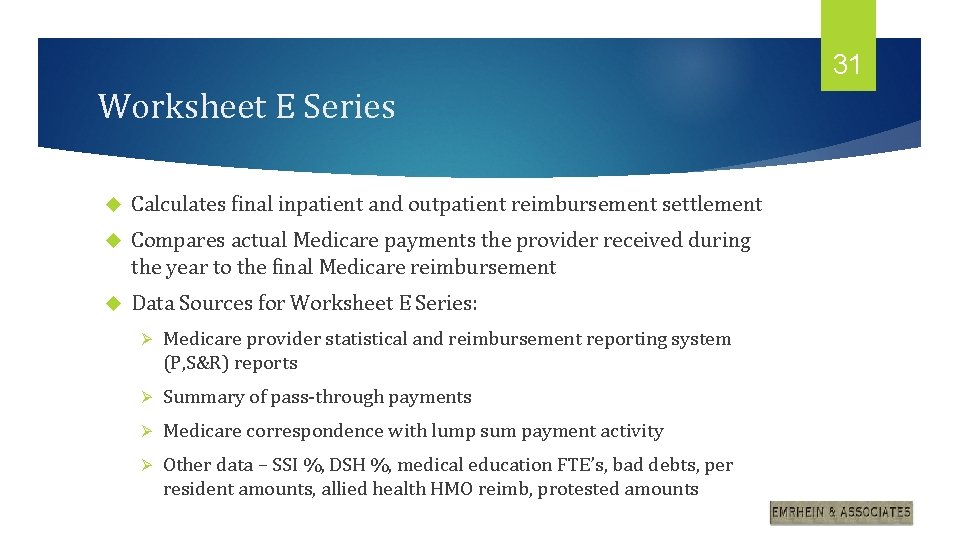
31 Worksheet E Series Calculates final inpatient and outpatient reimbursement settlement Compares actual Medicare payments the provider received during the year to the final Medicare reimbursement Data Sources for Worksheet E Series: Ø Medicare provider statistical and reimbursement reporting system (P, S&R) reports Ø Summary of pass-through payments Ø Medicare correspondence with lump sum payment activity Ø Other data – SSI %, DSH %, medical education FTE’s, bad debts, per resident amounts, allied health HMO reimb, protested amounts
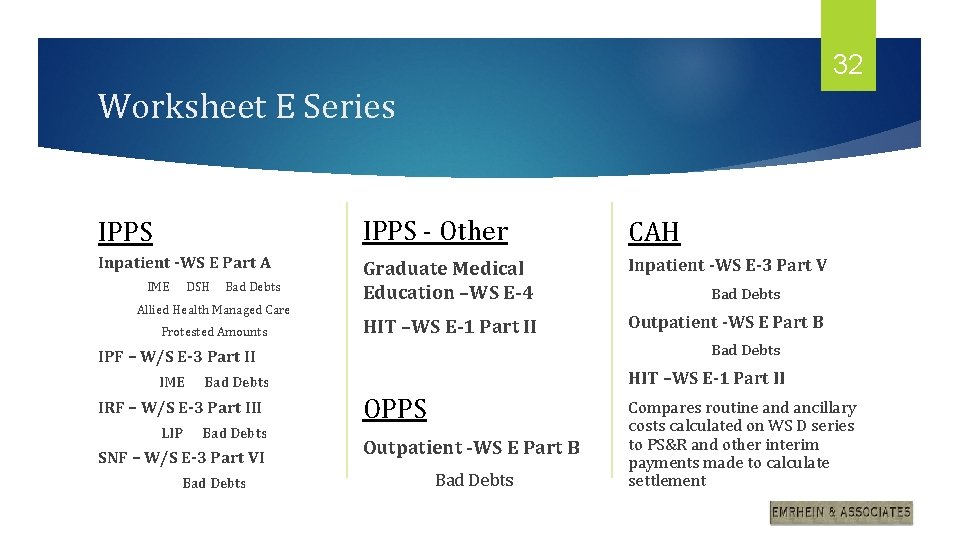
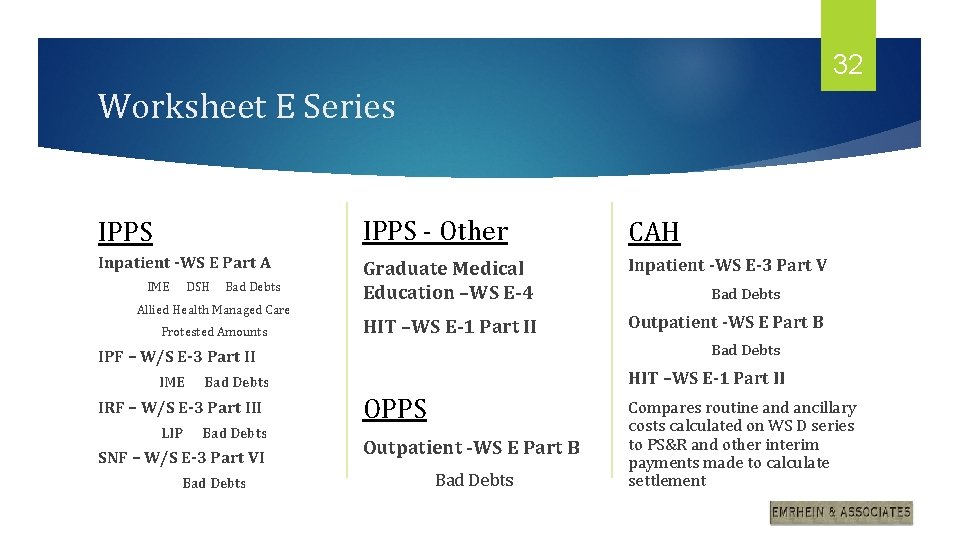
32 Worksheet E Series IPPS - Other CAH Inpatient -WS E Part A Graduate Medical Education –WS E-4 Inpatient -WS E-3 Part V HIT –WS E-1 Part II Outpatient -WS E Part B IME DSH Bad Debts Allied Health Managed Care Protested Amounts Bad Debts IPF – W/S E-3 Part II HIT –WS E-1 Part II IME Bad Debts IRF – W/S E-3 Part III LIP Bad Debts SNF – W/S E-3 Part VI Bad Debts OPPS Outpatient -WS E Part B Bad Debts Compares routine and ancillary costs calculated on WS D series to PS&R and other interim payments made to calculate settlement
33 Worksheet G Series – Financial Statement information Ø G is the balance sheet Ø G-1 is changes in fund balance Ø G-2 is statement of operating revenues and expenses Ø G-3 is the income statement
34 Additional Considerations When preparing the Medicare cost report it is important to keep in mind the following items: Ø Prior period MAC adjustments Ø New accounts, cost centers, changes, etc. Ø Proper identification of non-allowable expenses Ø Provider Reimbursement Manuals on-line Ø Change in number of licensed beds Ø Change in Medicare designation Ø Impact on cost based areas Ø Contracts and subsequent changes Ø Wage index related items Ø Reporting accuracy and consistency

35 Questions?
36 Important Final Thoughts: Once the cost report season is over, golf season begins!