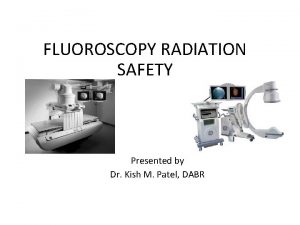
1 Introduction to Fluoroscopy Radiation Safety RTEC 124




- Slides: 55
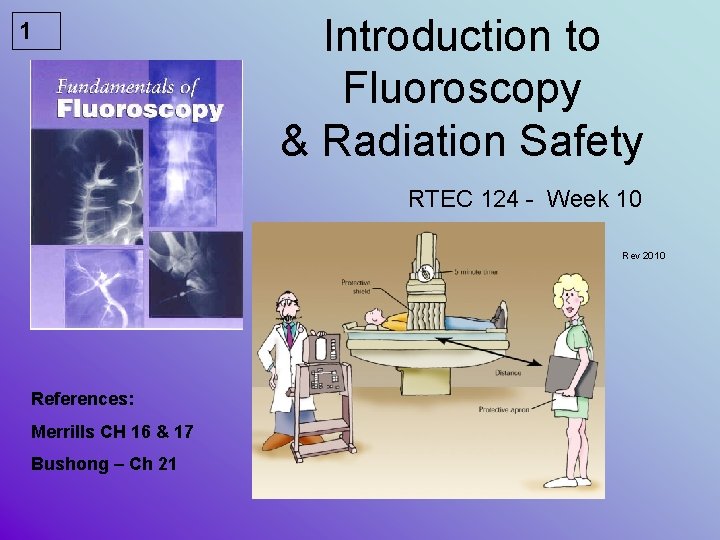
1 Introduction to Fluoroscopy & Radiation Safety RTEC 124 - Week 10 Rev 2010 References: Merrills CH 16 & 17 Bushong – Ch 21
2 CONVENTIONAL FLUOROSCOPY INVENTED BY THOMAS EDISON Early Fluoroscopy
3 Digital / Fluoro Equipment Check off • MUST BE COMPLETED PRIOR TO DOING ANY PATIENT EXAMS • Fluoroscopy Procedures must ALWAYS be supervised – even after a check off • You MUST be a CRT to have a Fluoroscopy Lic to operated fluoro units in California (CDPH-RHB Title 17)
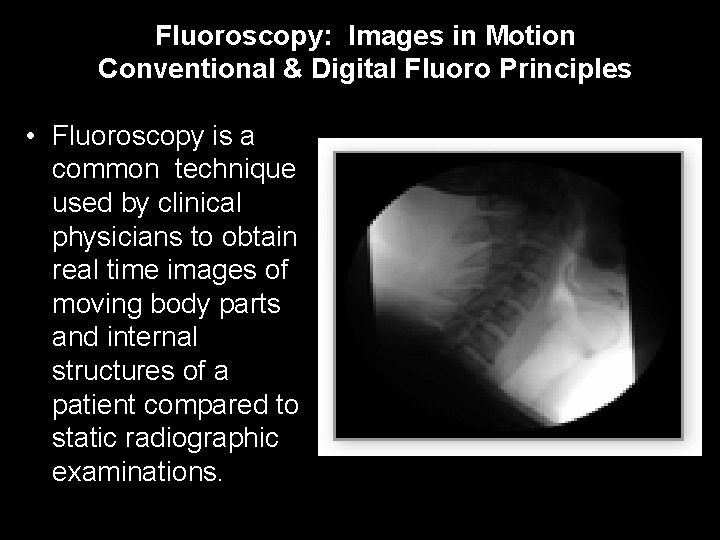
4 Fluoroscopy: Images in Motion Conventional & Digital Fluoro Principles • Fluoroscopy is a common technique used by clinical physicians to obtain real time images of moving body parts and internal structures of a patient compared to static radiographic examinations.
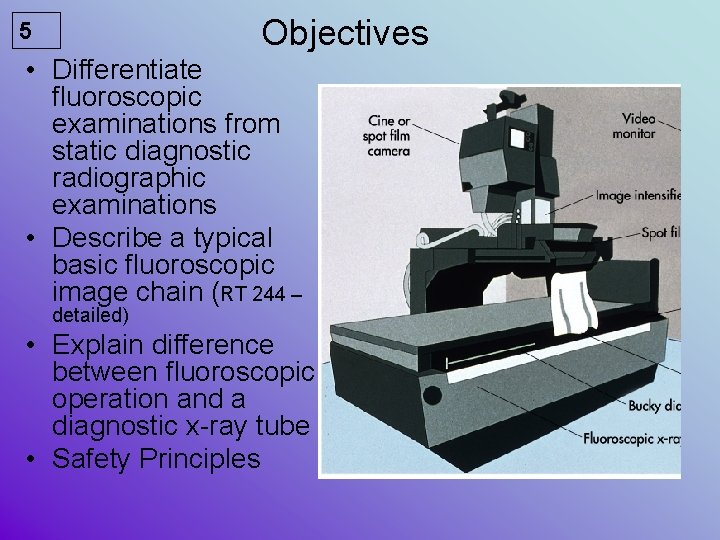
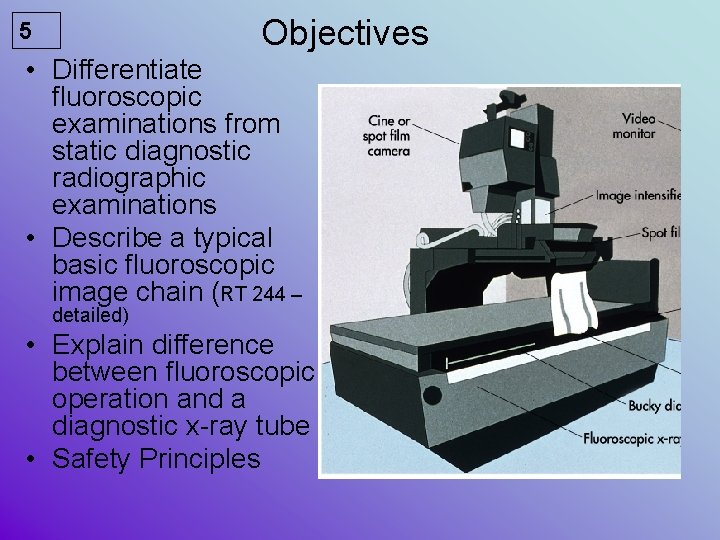
Objectives 5 • Differentiate fluoroscopic examinations from static diagnostic radiographic examinations • Describe a typical basic fluoroscopic image chain (RT 244 – detailed) • Explain difference between fluoroscopic operation and a diagnostic x-ray tube • Safety Principles
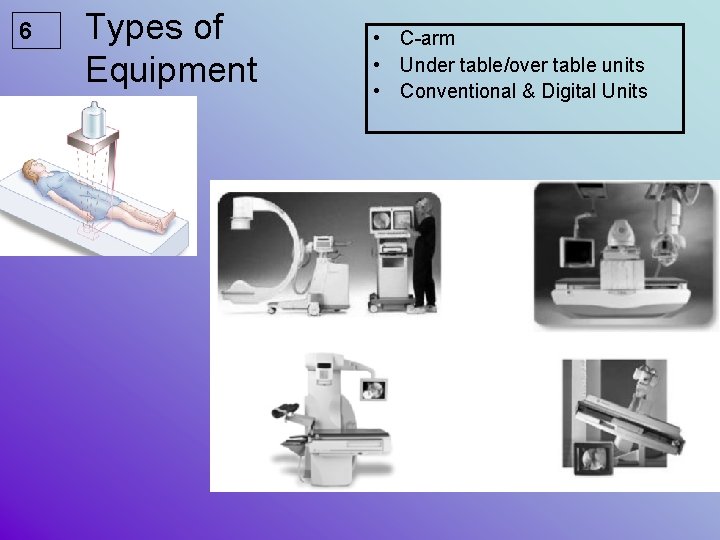
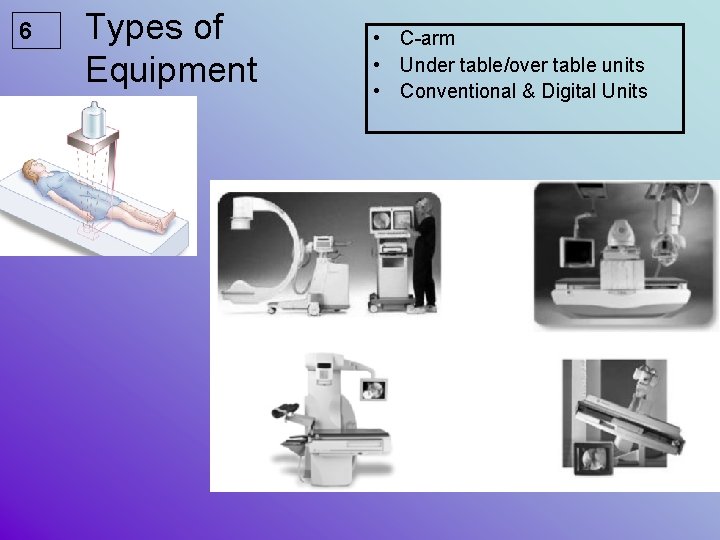
6 Types of Equipment • C-arm • Under table/over table units • Conventional & Digital Units
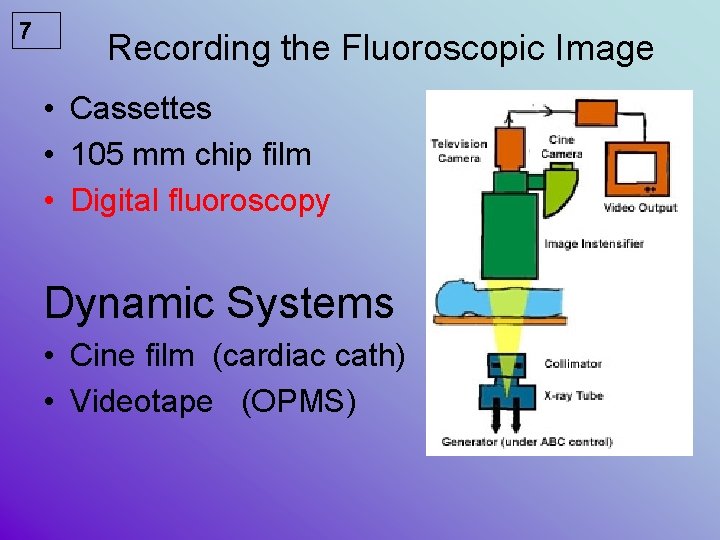
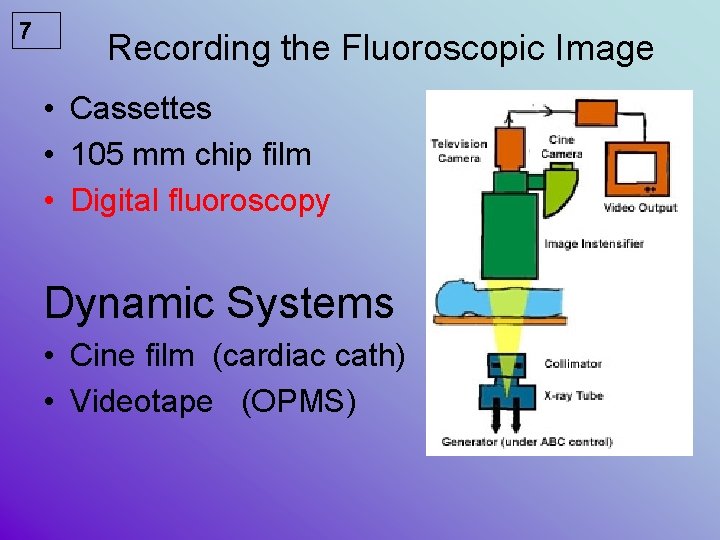
7 Recording the Fluoroscopic Image • Cassettes • 105 mm chip film • Digital fluoroscopy Dynamic Systems • Cine film (cardiac cath) • Videotape (OPMS)
8 IMAGE INTENSIFICAITON photons are ampilfied + multiplied • IMAGES ARE VIEWED ON A TV SCREEN/MONITOR
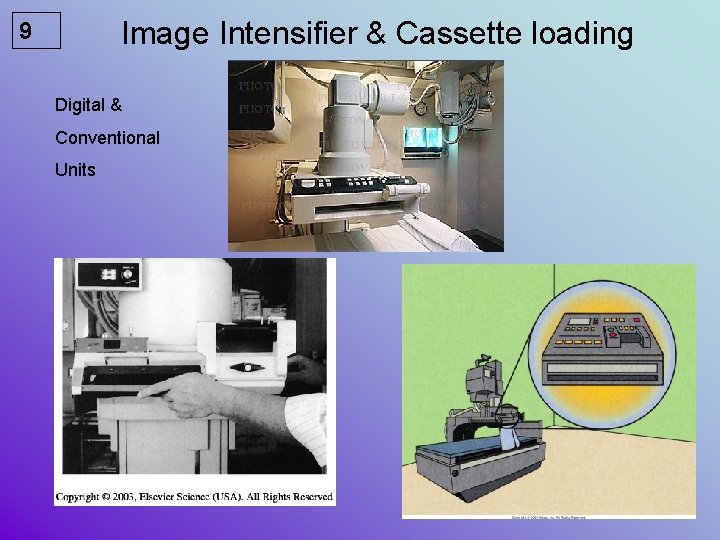
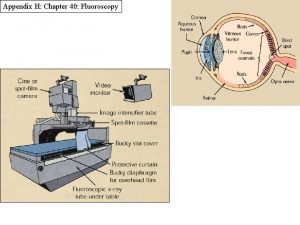
Image Intensifier & Cassette loading 9 Digital & Conventional Units
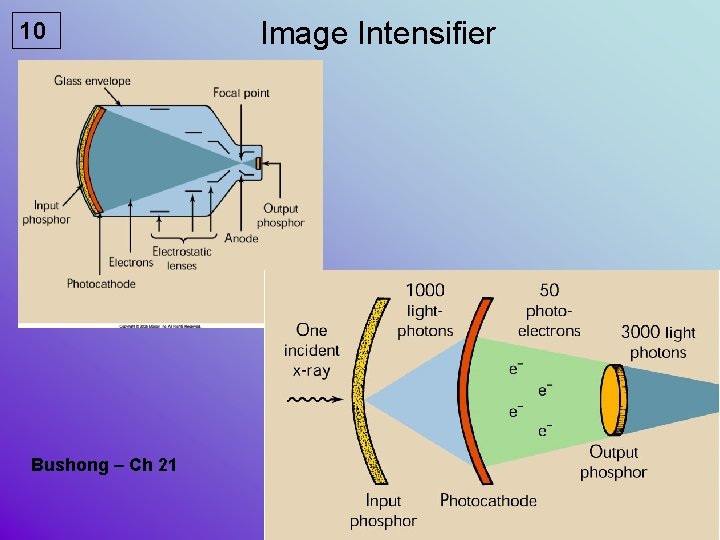
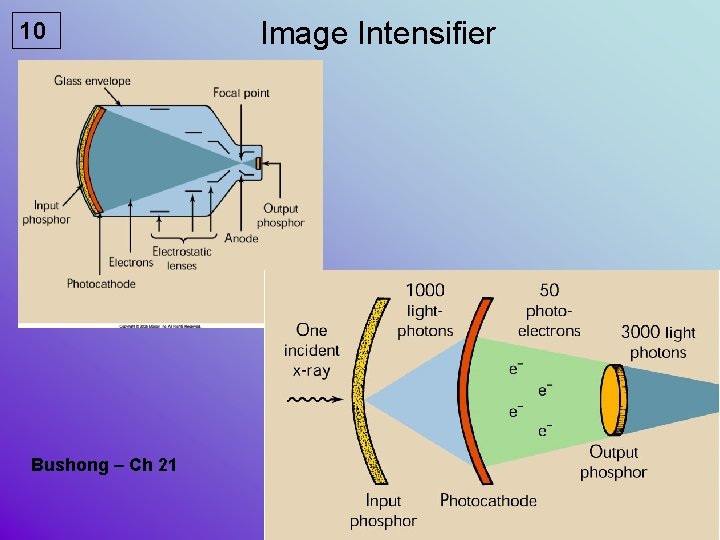
10 Bushong – Ch 21 Image Intensifier
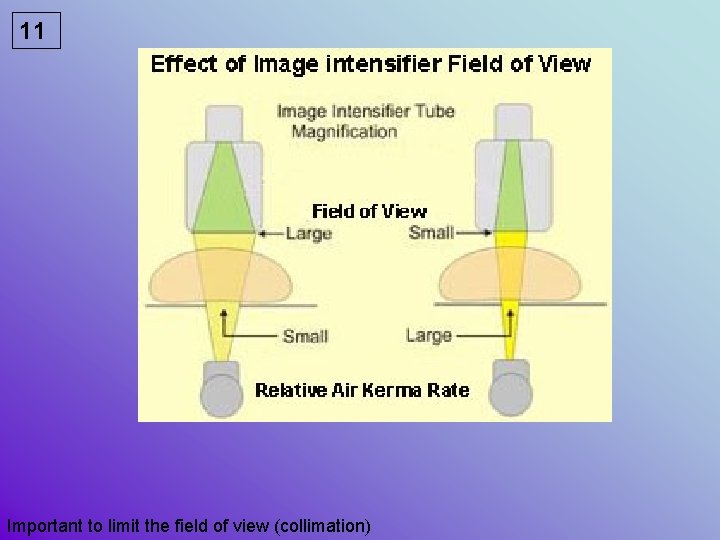
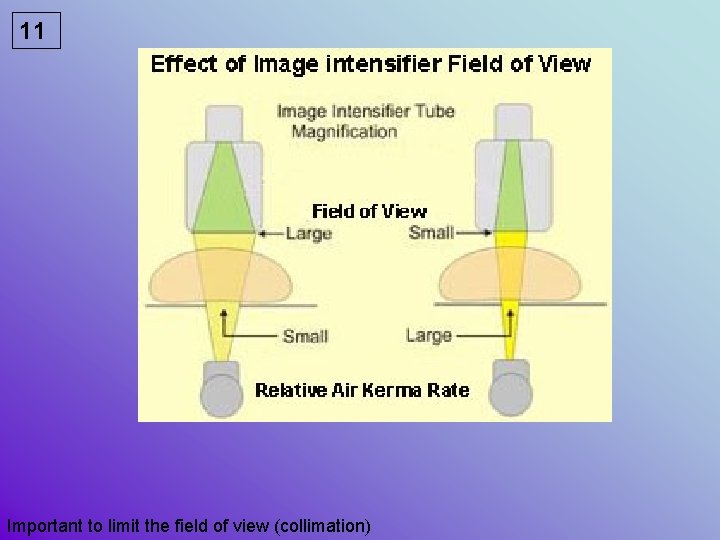
11 Important to limit the field of view (collimation)
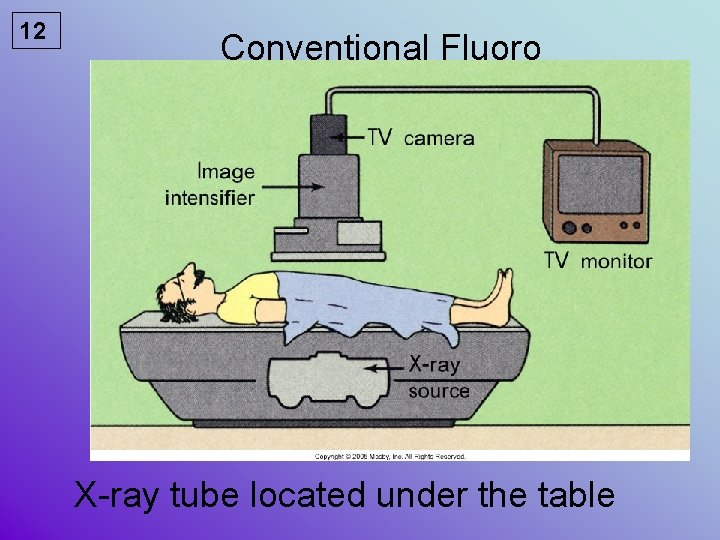
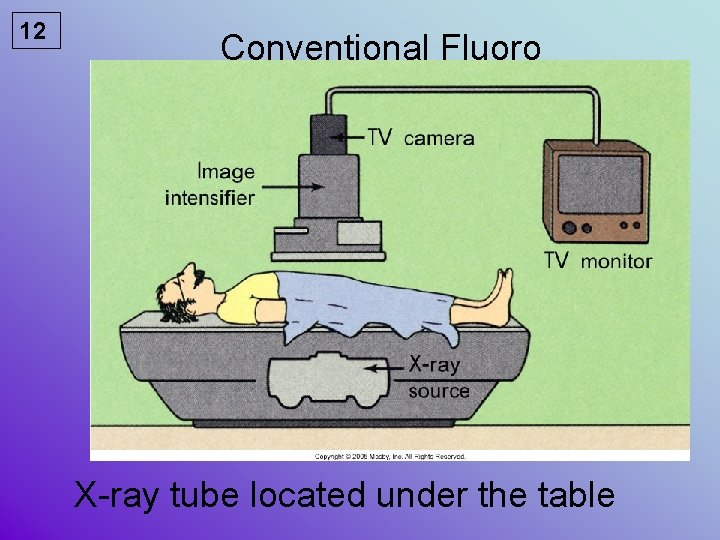
12 Conventional Fluoro X-ray tube located under the table
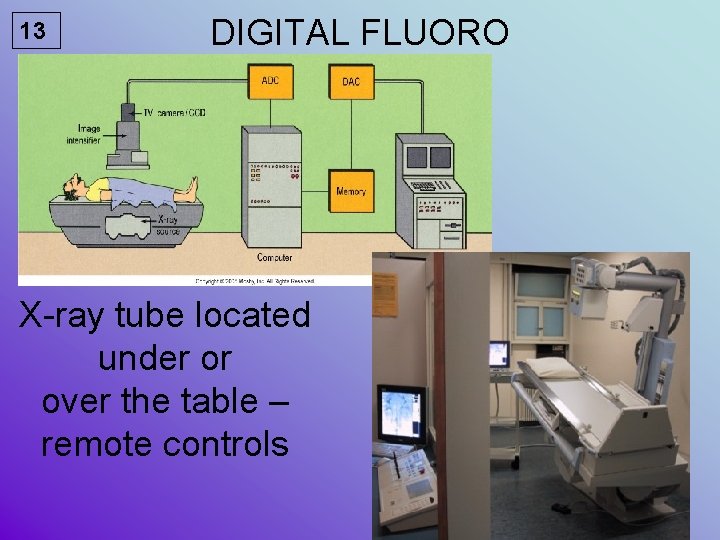
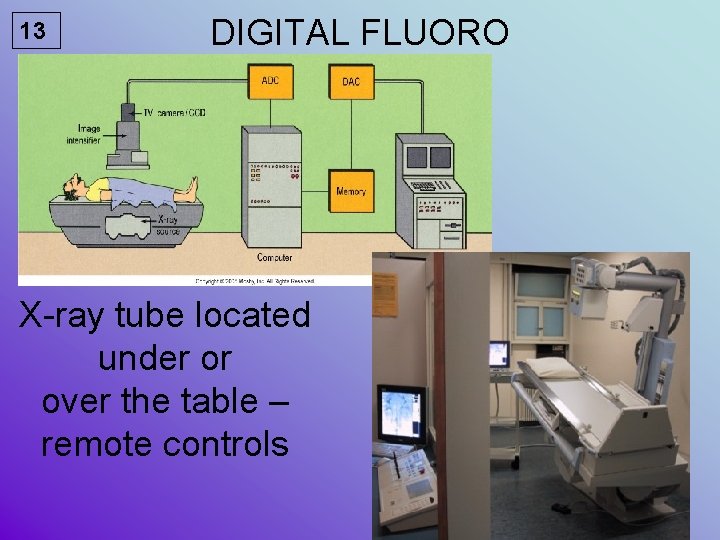
13 DIGITAL FLUORO X-ray tube located under or over the table – remote controls
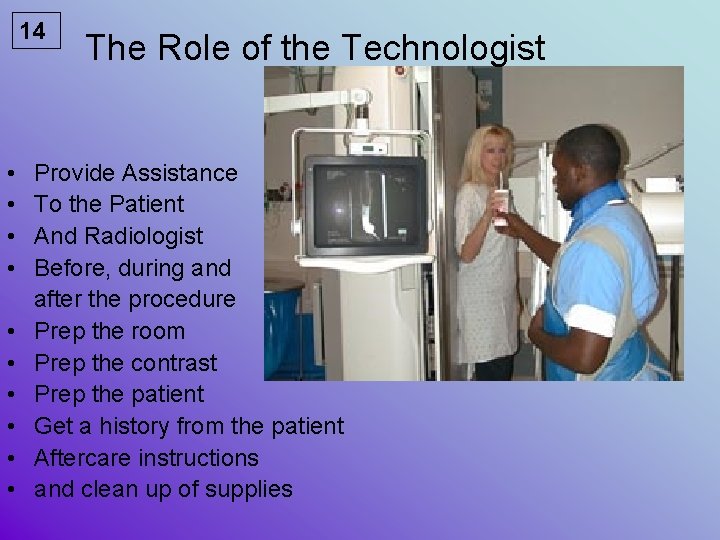
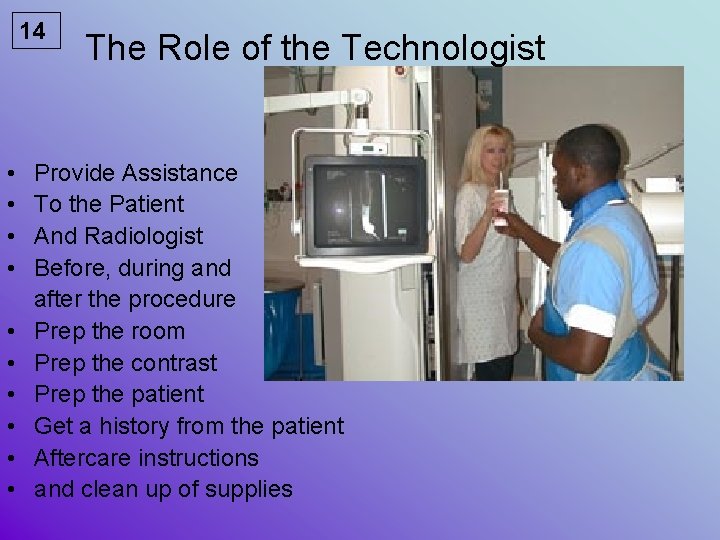
14 • • • The Role of the Technologist Provide Assistance To the Patient And Radiologist Before, during and after the procedure Prep the room Prep the contrast Prep the patient Get a history from the patient Aftercare instructions and clean up of supplies
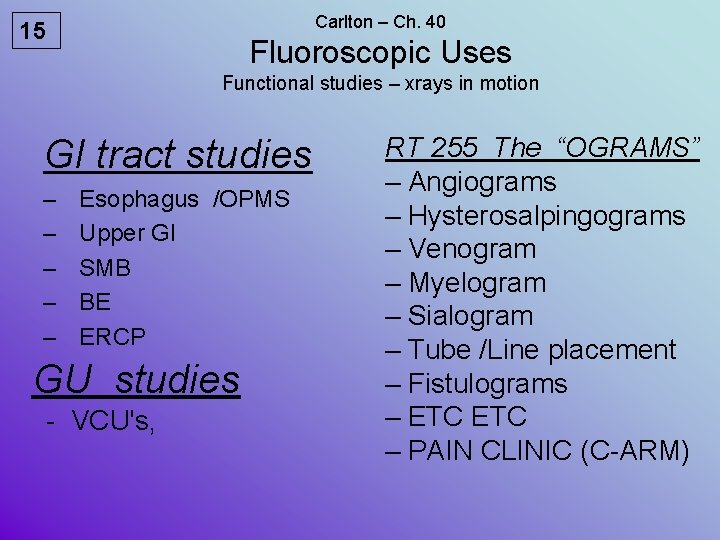
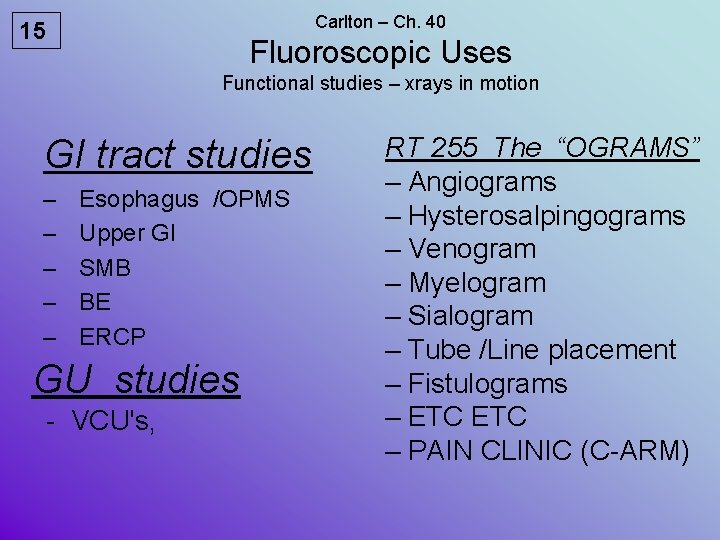
Carlton – Ch. 40 15 Fluoroscopic Uses Functional studies – xrays in motion GI tract studies – – – Esophagus /OPMS Upper GI SMB BE ERCP GU studies - VCU's, RT 255 The “OGRAMS” – Angiograms – Hysterosalpingograms – Venogram – Myelogram – Sialogram – Tube /Line placement – Fistulograms – ETC – PAIN CLINIC (C-ARM)
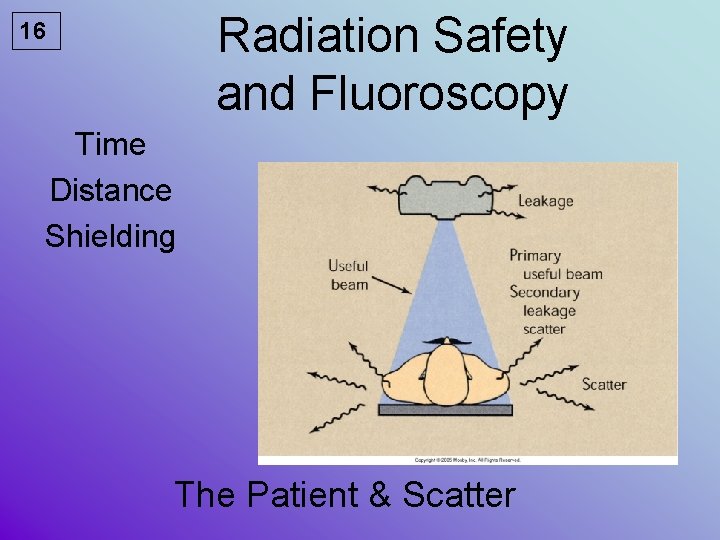
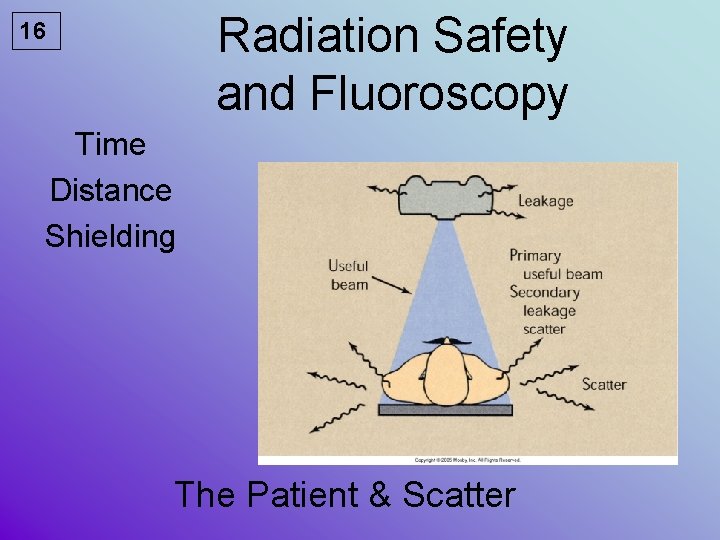
Radiation Safety and Fluoroscopy 16 Time Distance Shielding The Patient & Scatter

17 Radiation Protection During Fluoroscopy • The patient • The radiographer and radiologist • Others
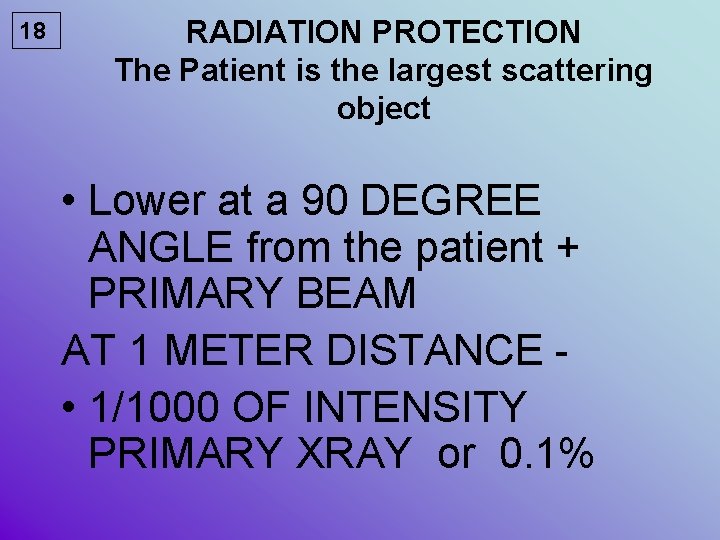
18 RADIATION PROTECTION The Patient is the largest scattering object • Lower at a 90 DEGREE ANGLE from the patient + PRIMARY BEAM AT 1 METER DISTANCE • 1/1000 OF INTENSITY PRIMARY XRAY or 0. 1%
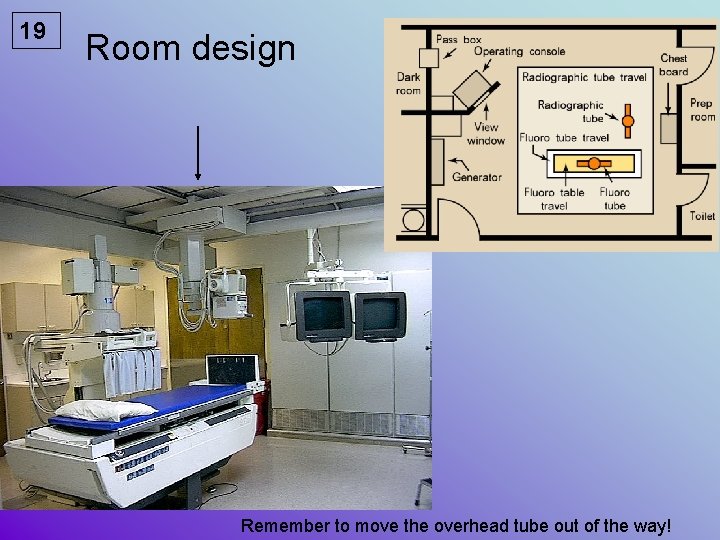
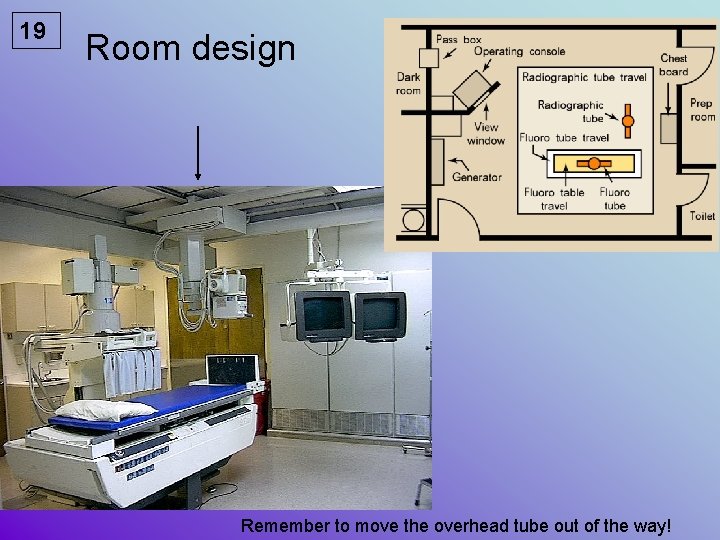
19 Room design Remember to move the overhead tube out of the way!
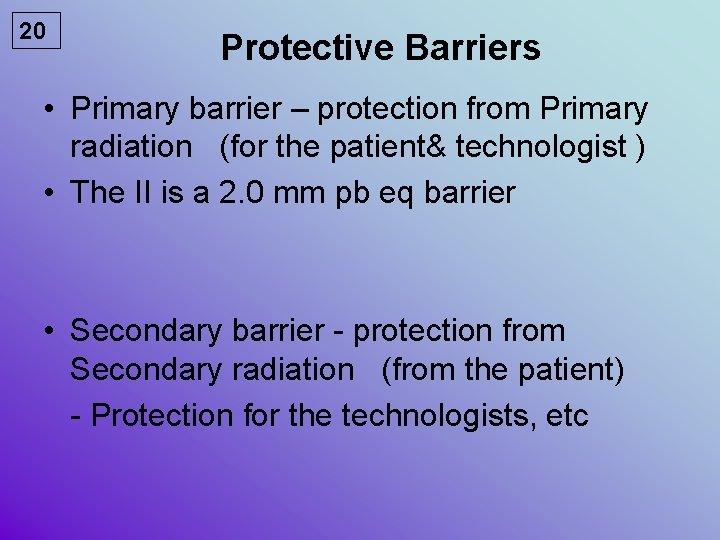
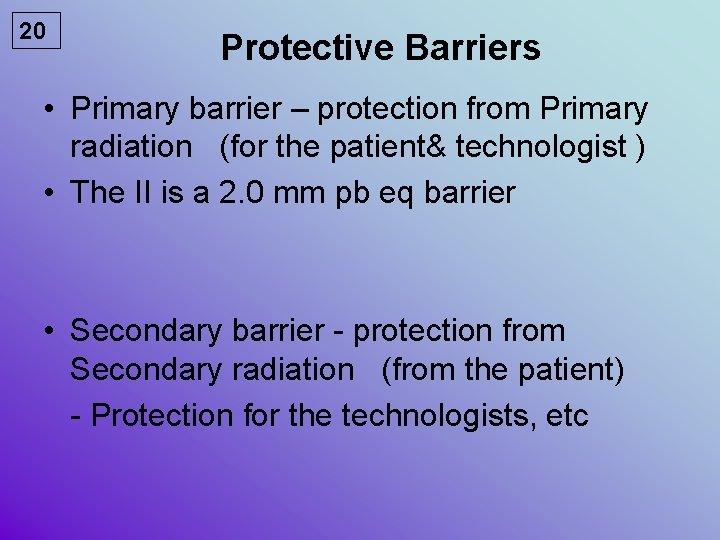
20 Protective Barriers • Primary barrier – protection from Primary radiation (for the patient& technologist ) • The II is a 2. 0 mm pb eq barrier • Secondary barrier - protection from Secondary radiation (from the patient) - Protection for the technologists, etc
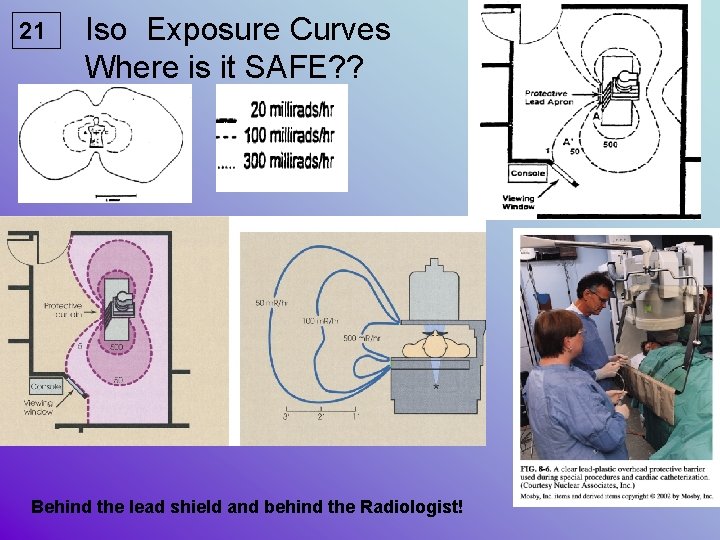
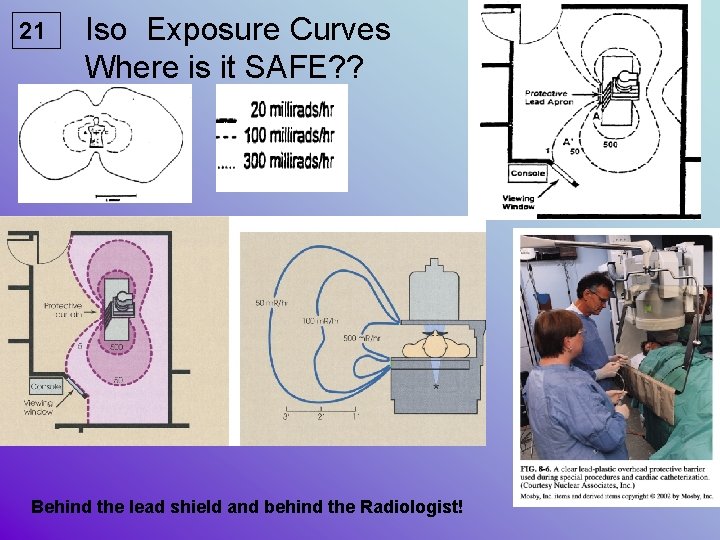
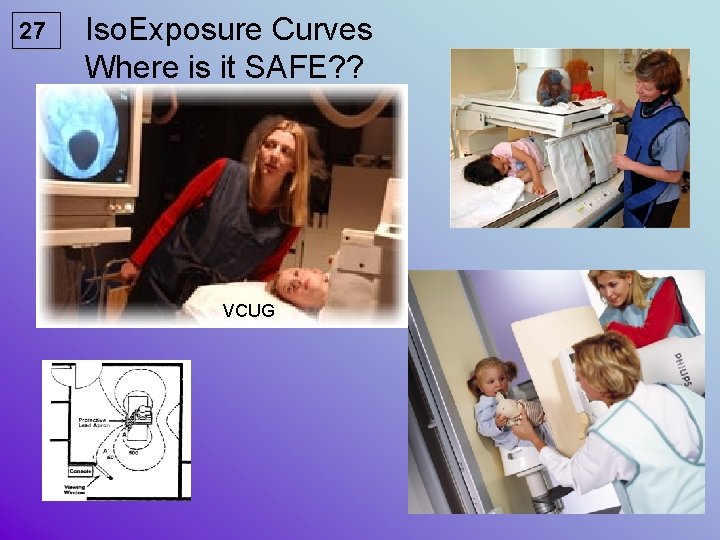
21 Iso Exposure Curves Where is it SAFE? ? Behind the lead shield and behind the Radiologist!
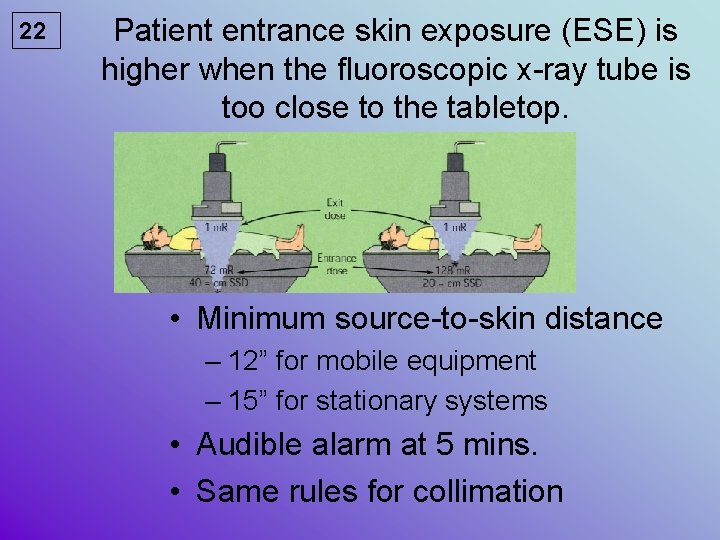
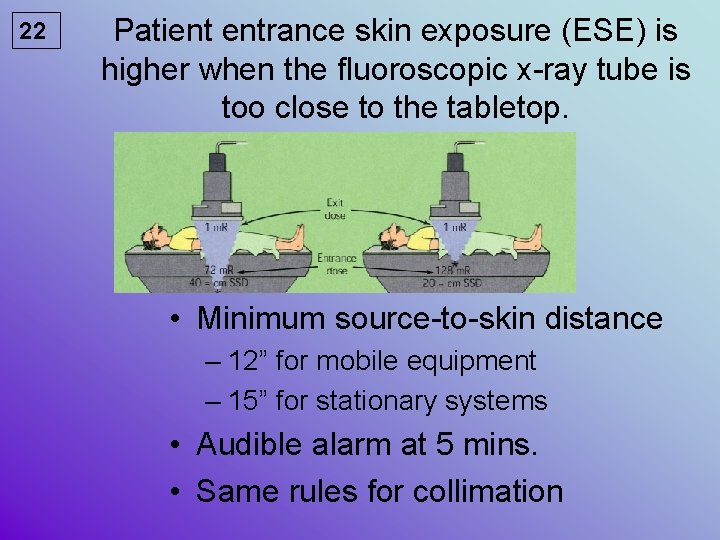
22 Patient entrance skin exposure (ESE) is higher when the fluoroscopic x-ray tube is too close to the tabletop. • Minimum source-to-skin distance – 12” for mobile equipment – 15” for stationary systems • Audible alarm at 5 mins. • Same rules for collimation
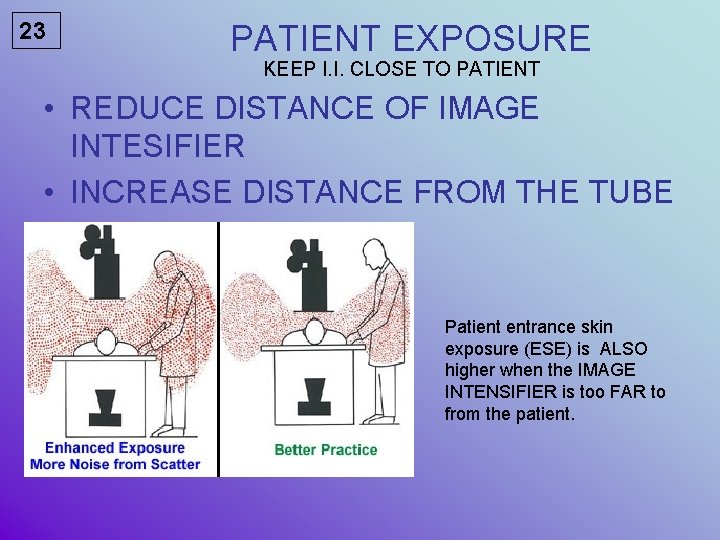
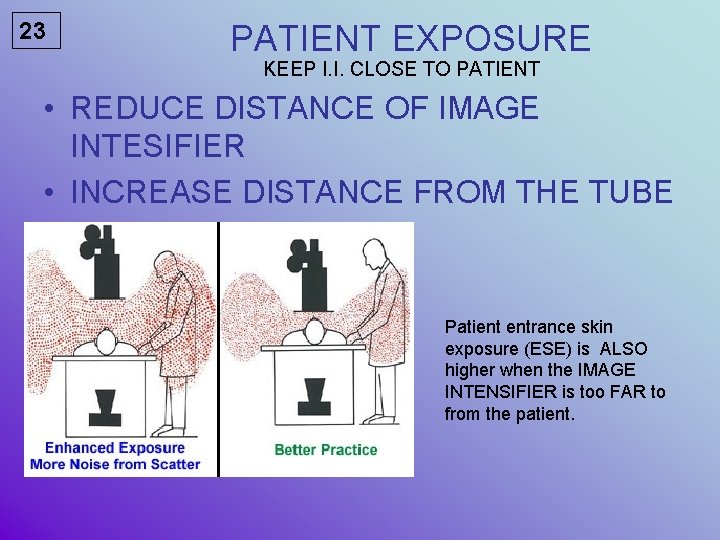
23 PATIENT EXPOSURE KEEP I. I. CLOSE TO PATIENT • REDUCE DISTANCE OF IMAGE INTESIFIER • INCREASE DISTANCE FROM THE TUBE Patient entrance skin exposure (ESE) is ALSO higher when the IMAGE INTENSIFIER is too FAR to from the patient.
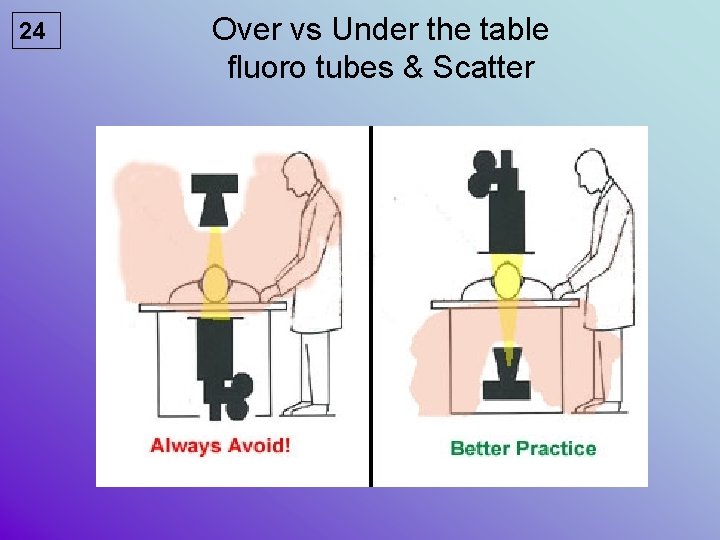
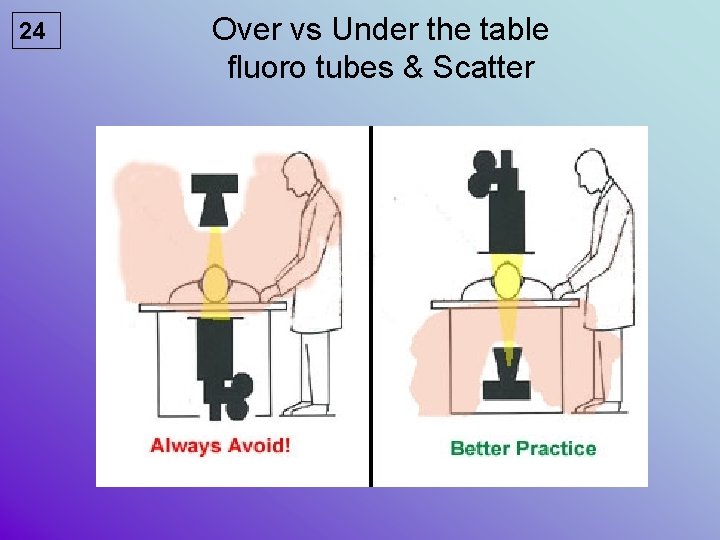
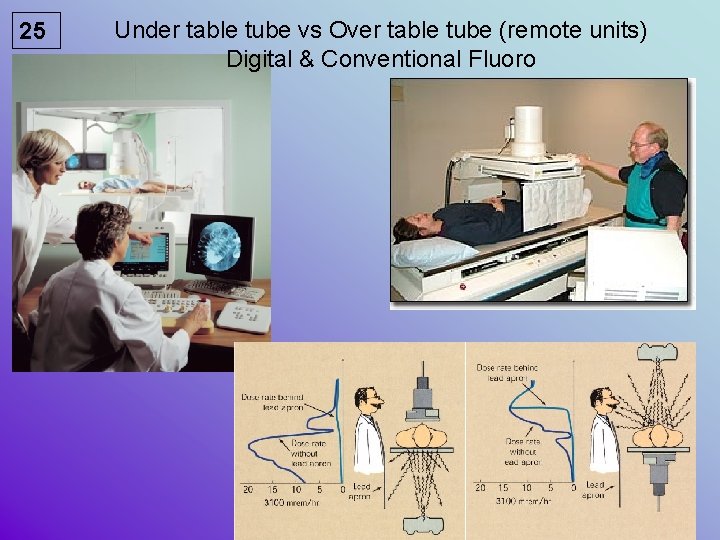
24 Over vs Under the table fluoro tubes & Scatter
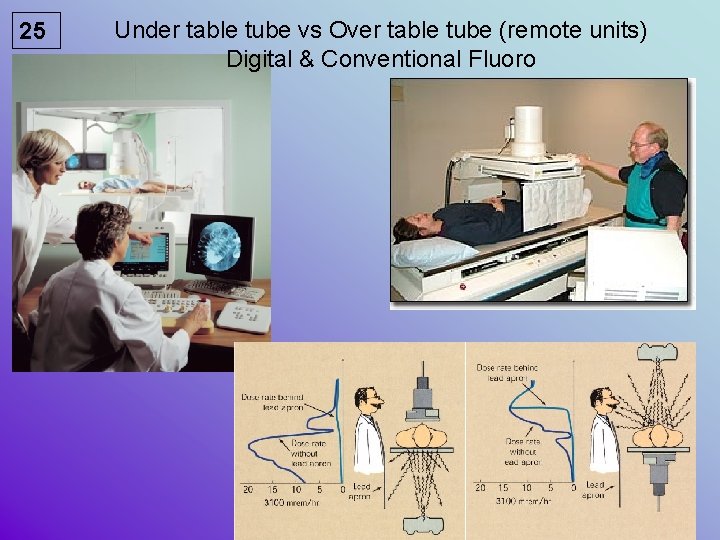
25 Under table tube vs Over table tube (remote units) Digital & Conventional Fluoro
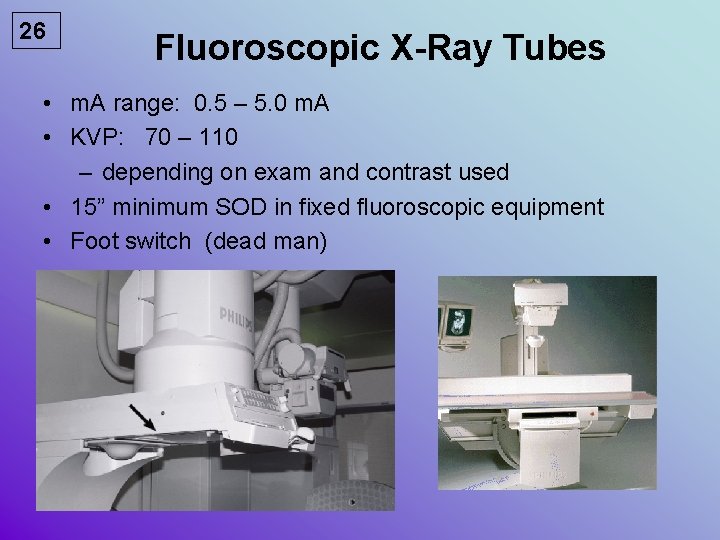
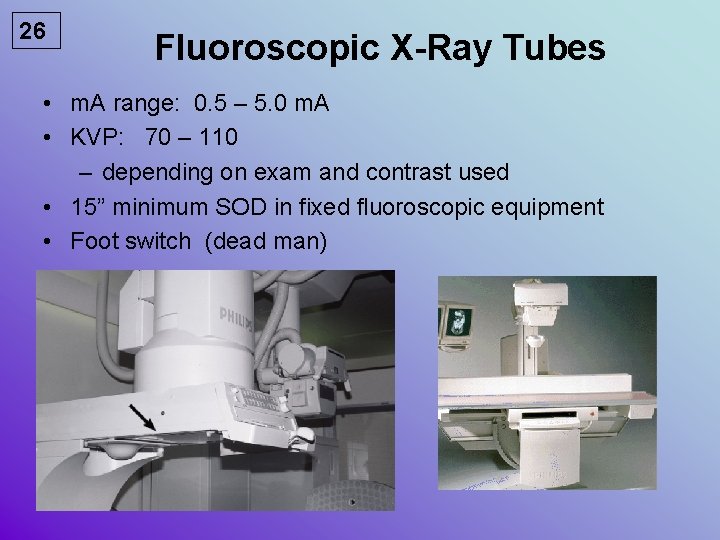
26 Fluoroscopic X-Ray Tubes • m. A range: 0. 5 – 5. 0 m. A • KVP: 70 – 110 – depending on exam and contrast used • 15” minimum SOD in fixed fluoroscopic equipment • Foot switch (dead man)
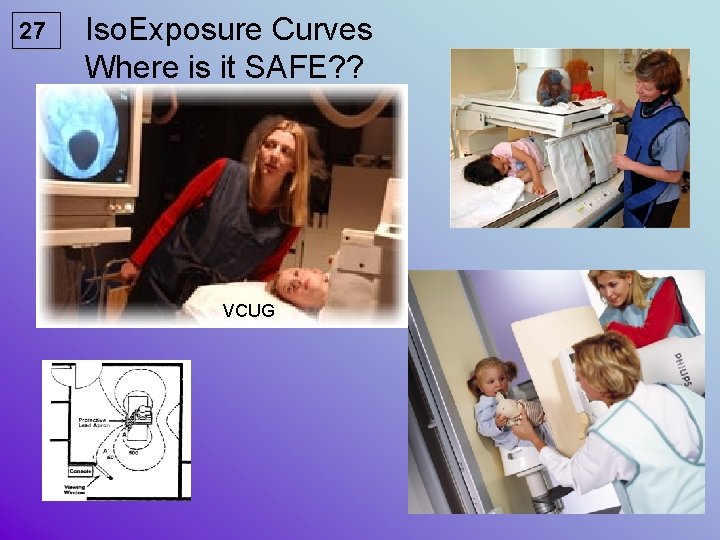
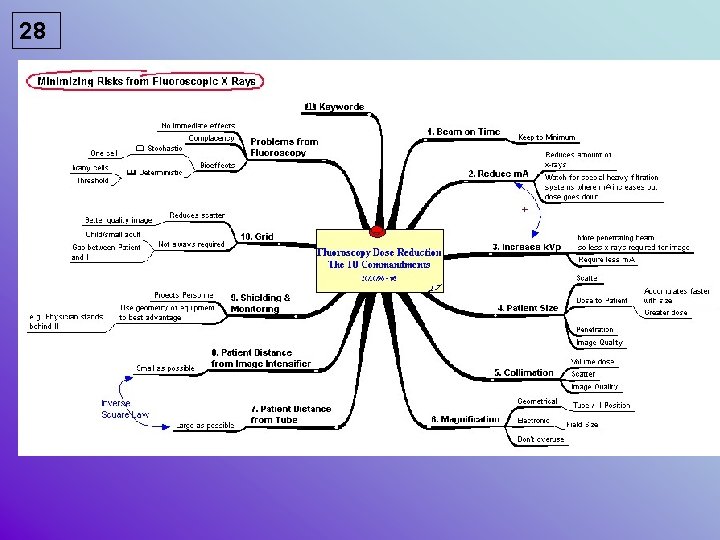
27 Iso. Exposure Curves Where is it SAFE? ? VCUG
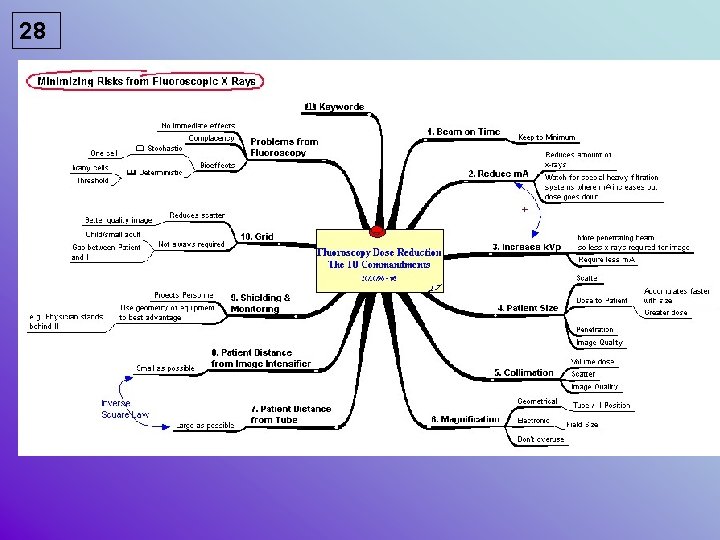
28
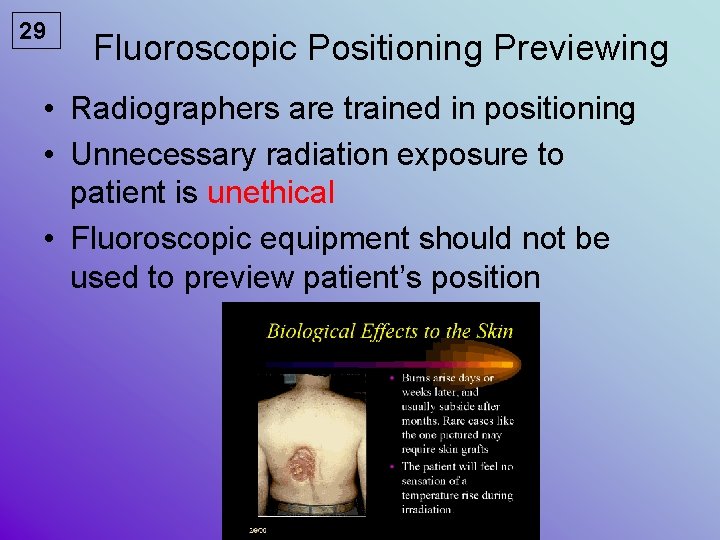
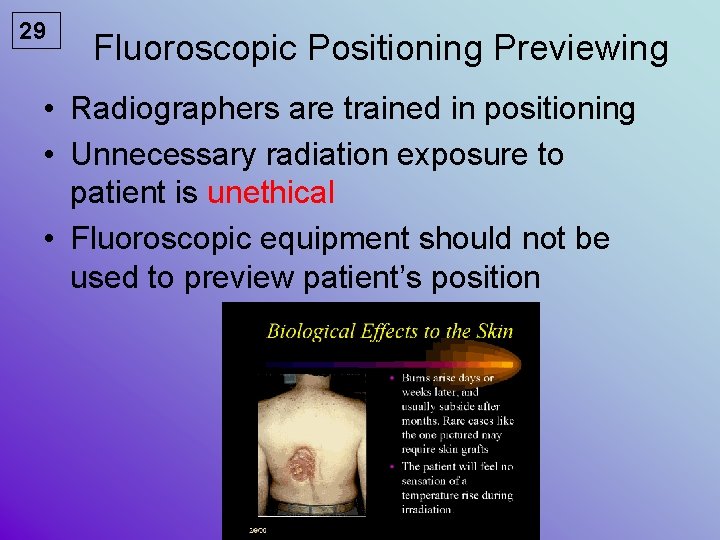
29 Fluoroscopic Positioning Previewing • Radiographers are trained in positioning • Unnecessary radiation exposure to patient is unethical • Fluoroscopic equipment should not be used to preview patient’s position
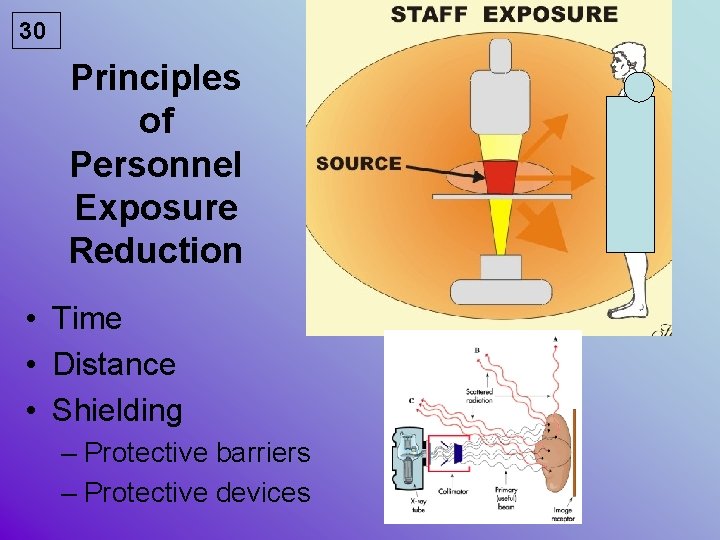
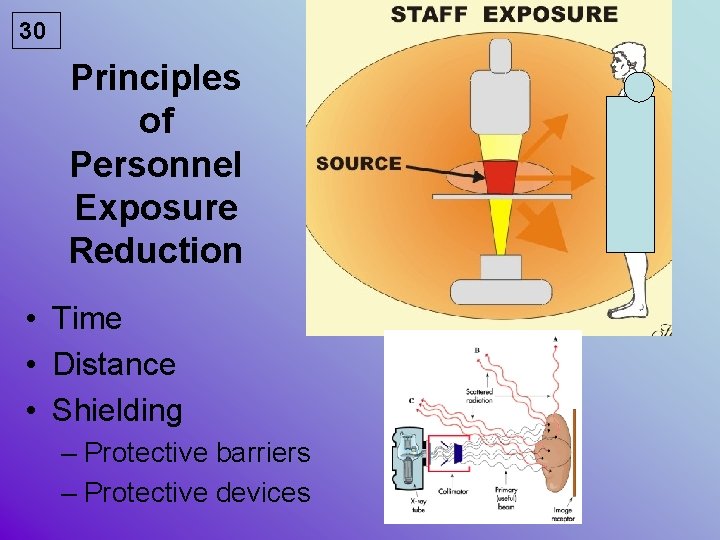
30 Principles of Personnel Exposure Reduction • Time • Distance • Shielding – Protective barriers – Protective devices
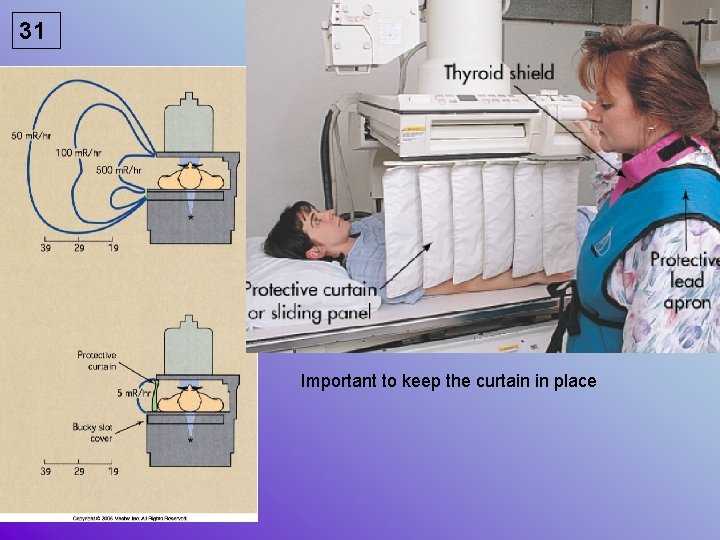
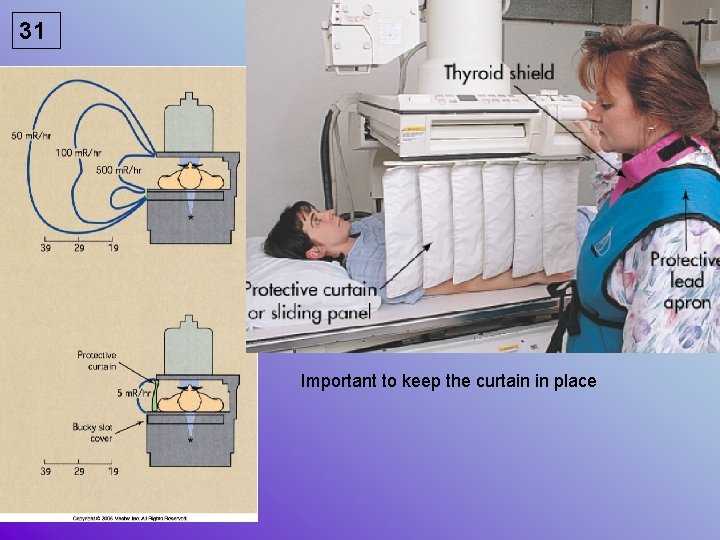
31 Important to keep the curtain in place
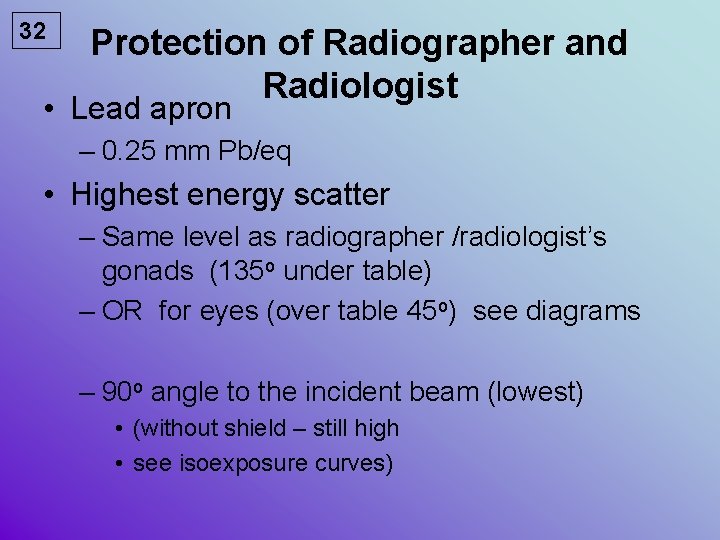
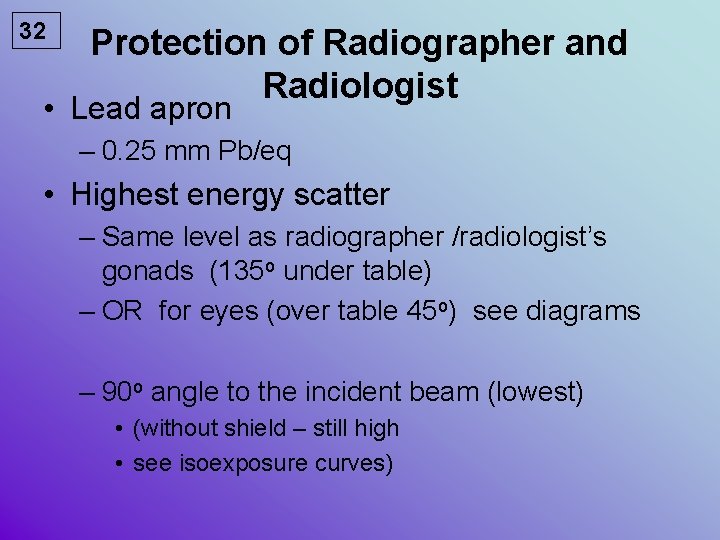
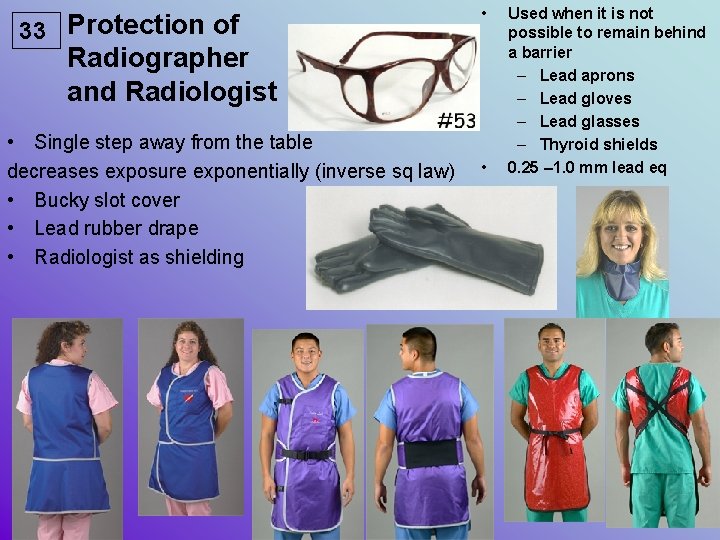
32 Protection of Radiographer and Radiologist • Lead apron – 0. 25 mm Pb/eq • Highest energy scatter – Same level as radiographer /radiologist’s gonads (135 o under table) – OR for eyes (over table 45 o) see diagrams – 90 o angle to the incident beam (lowest) • (without shield – still high • see isoexposure curves)
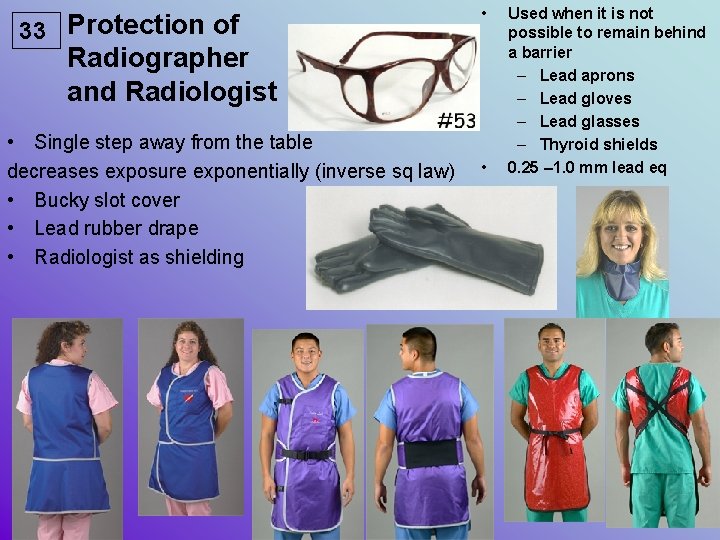
33 Protection of • Radiographer and Radiologist • Single step away from the table decreases exposure exponentially (inverse sq law) • Bucky slot cover • Lead rubber drape • Radiologist as shielding • Used when it is not possible to remain behind a barrier – Lead aprons – Lead gloves – Lead glasses – Thyroid shields 0. 25 – 1. 0 mm lead eq
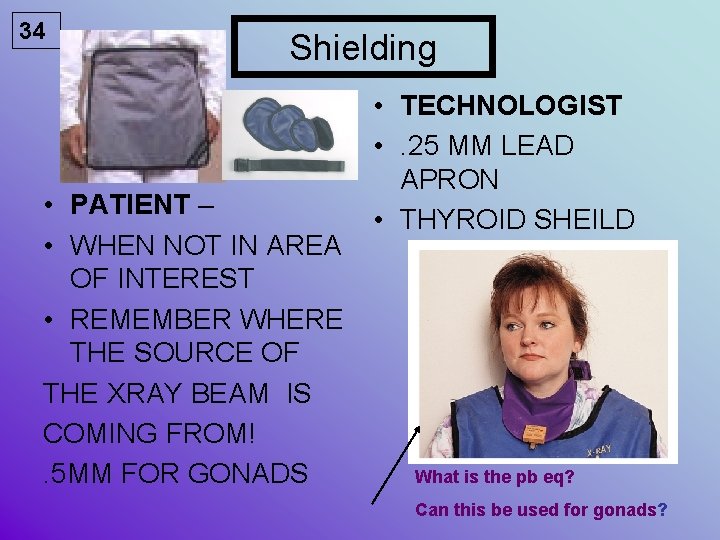
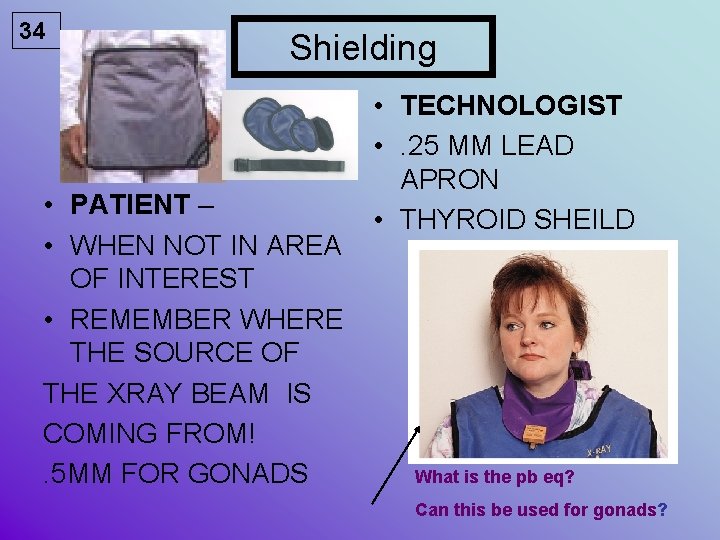
34 Shielding • PATIENT – • WHEN NOT IN AREA OF INTEREST • REMEMBER WHERE THE SOURCE OF THE XRAY BEAM IS COMING FROM!. 5 MM FOR GONADS • TECHNOLOGIST • . 25 MM LEAD APRON • THYROID SHEILD What is the pb eq? Can this be used for gonads?
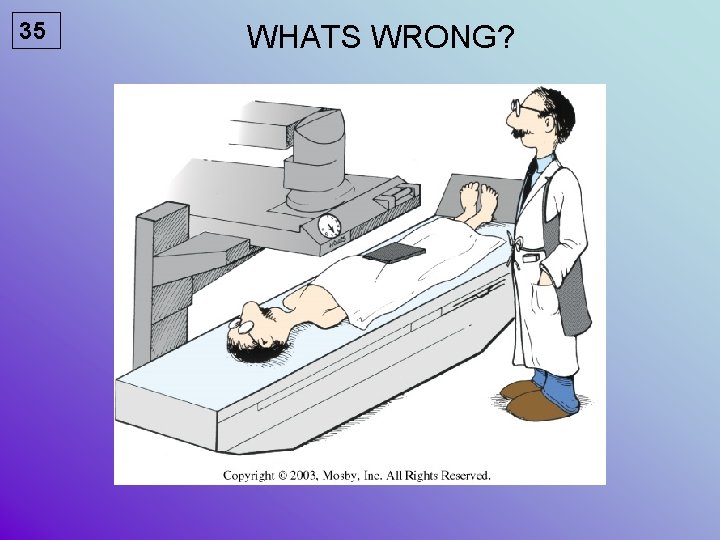
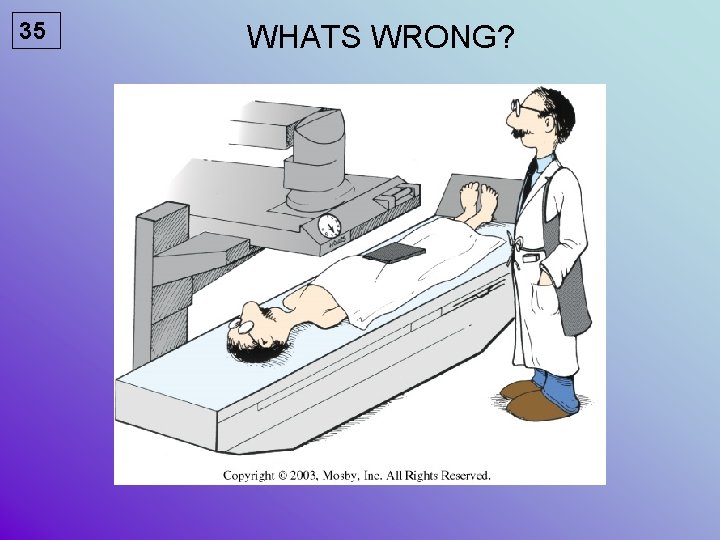
35 WHATS WRONG?
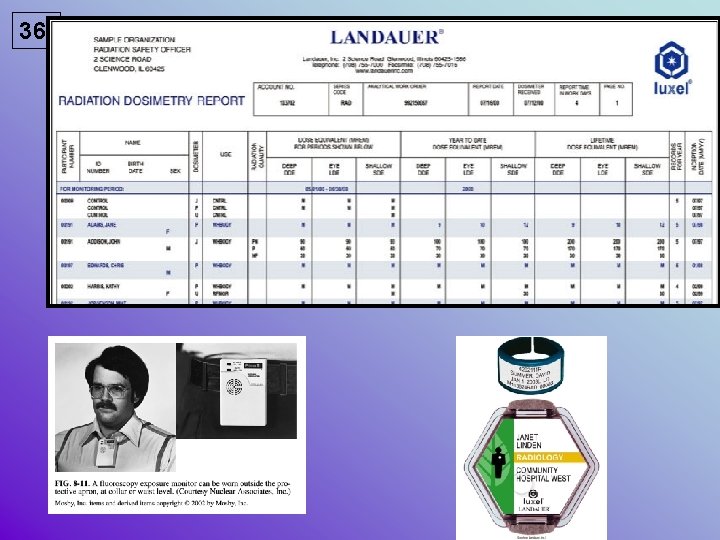
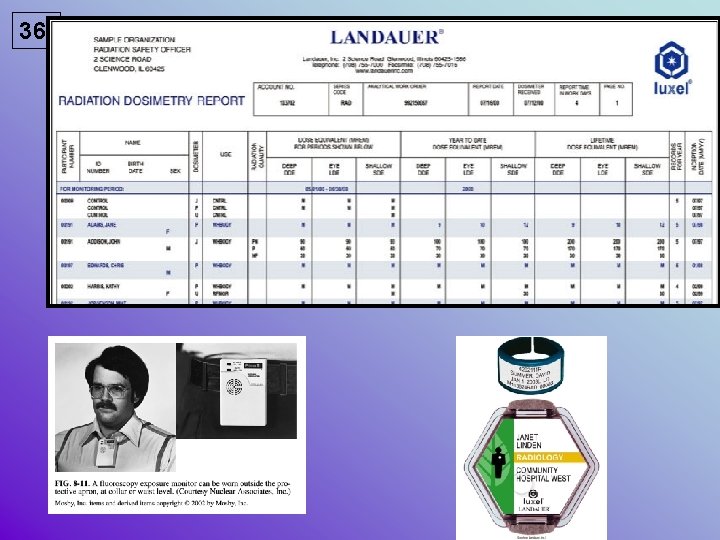
36
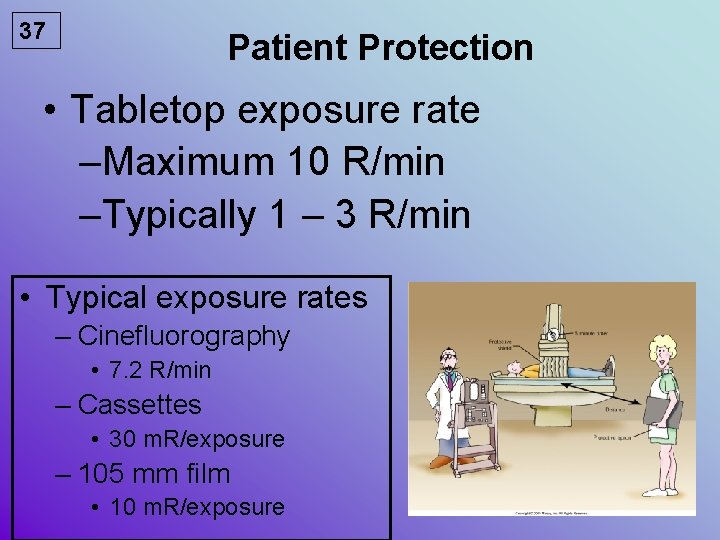
37 Patient Protection • Tabletop exposure rate –Maximum 10 R/min –Typically 1 – 3 R/min • Typical exposure rates – Cinefluorography • 7. 2 R/min – Cassettes • 30 m. R/exposure – 105 mm film • 10 m. R/exposure
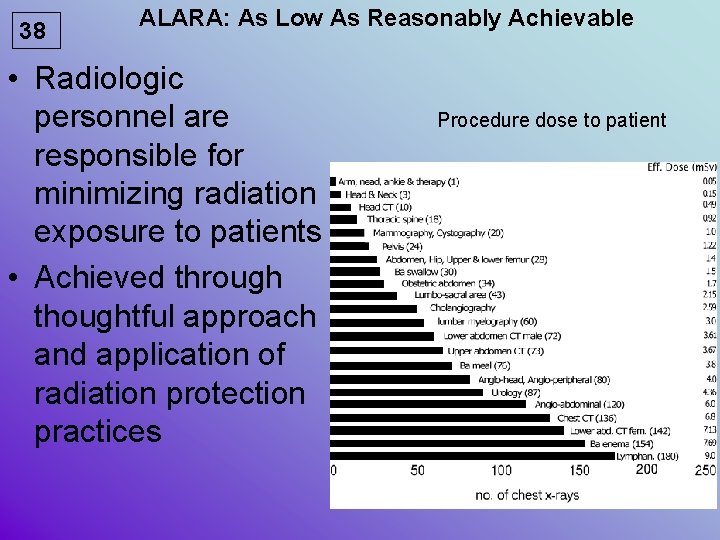
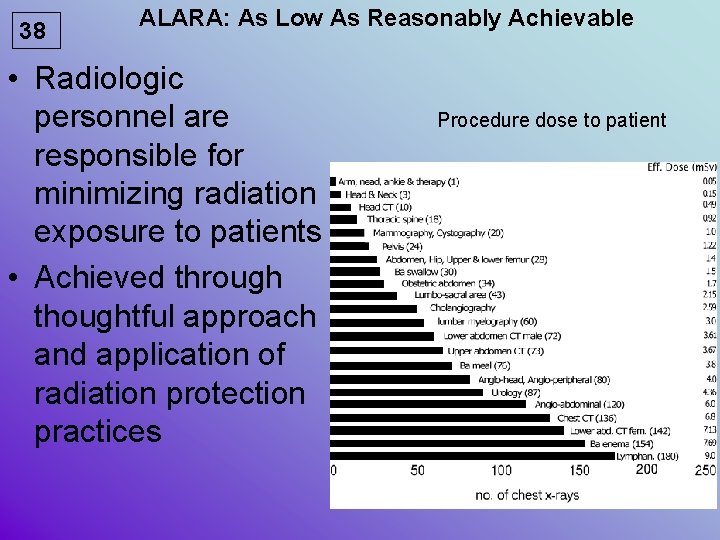
38 ALARA: As Low As Reasonably Achievable • Radiologic personnel are responsible for minimizing radiation exposure to patients • Achieved through thoughtful approach and application of radiation protection practices Procedure dose to patient
39 Protection of Others • Radiographer’s responsibility to inform others in the room to wear lead apron • Do not initiate fluoroscopy until all persons have complied
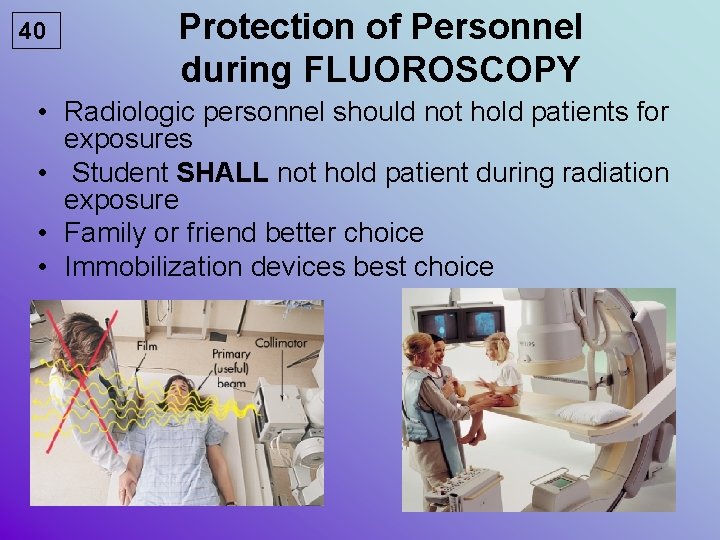
40 Protection of Personnel during FLUOROSCOPY • Radiologic personnel should not hold patients for exposures • Student SHALL not hold patient during radiation exposure • Family or friend better choice • Immobilization devices best choice
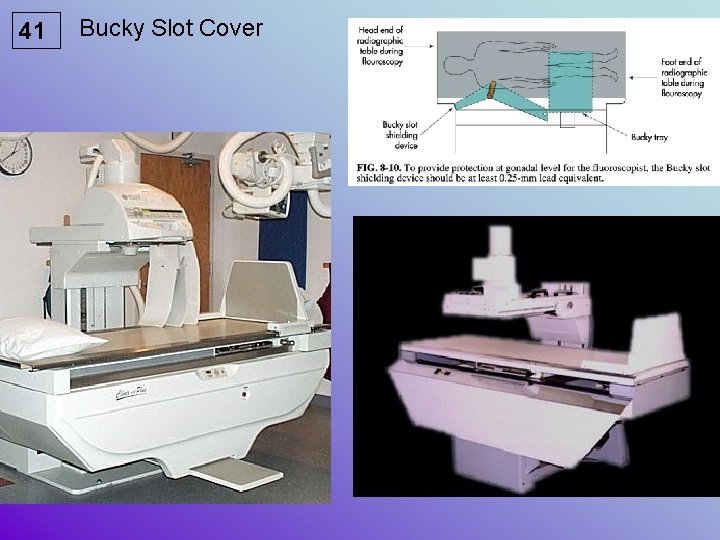
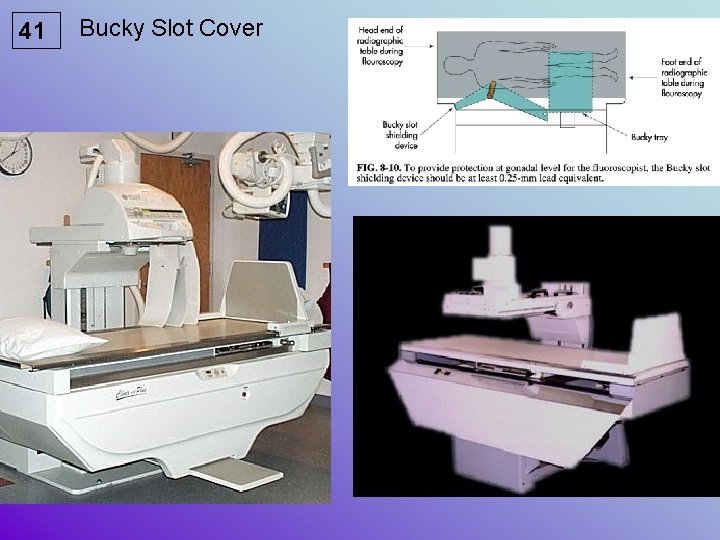
41 Bucky Slot Cover
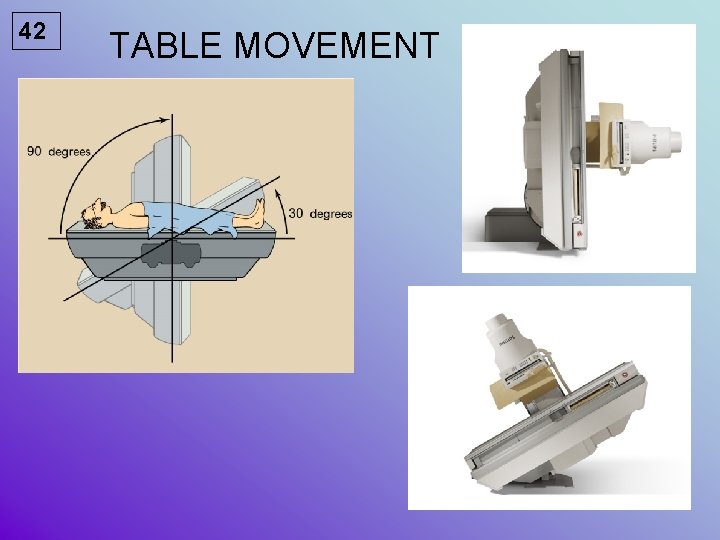
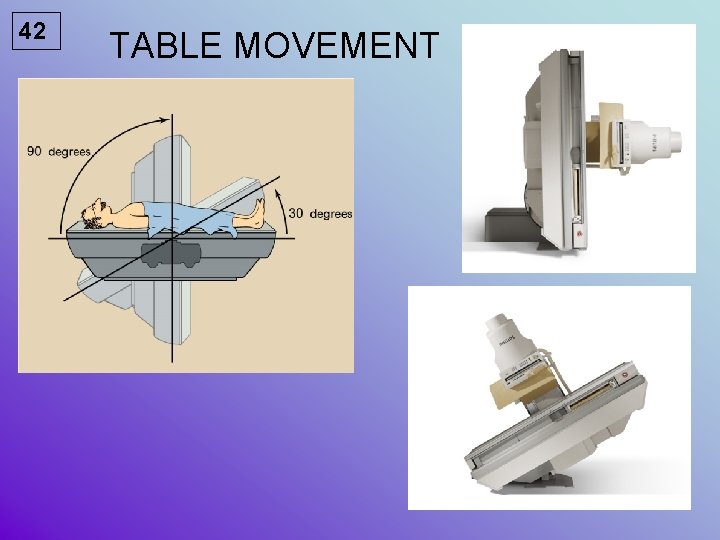
42 TABLE MOVEMENT
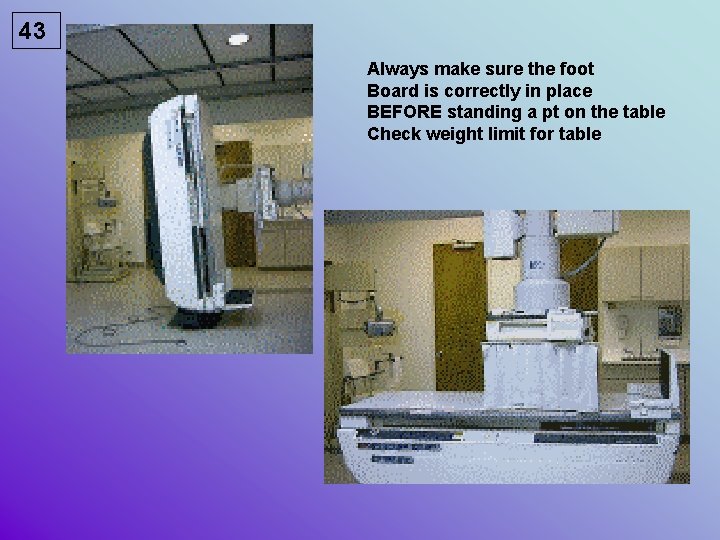
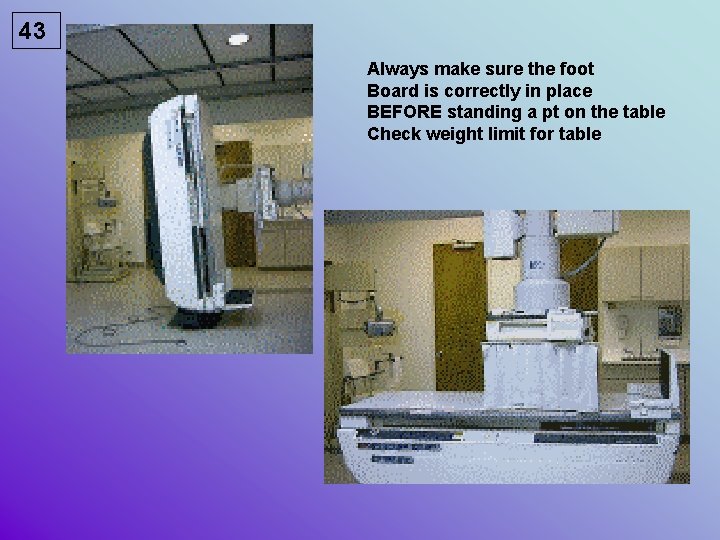
43 Always make sure the foot Board is correctly in place BEFORE standing a pt on the table Check weight limit for table

44 BASIC PROCEDURES For FLUOROSCOPY Note – do not allow pt to place Cup on the II - Table will move from vertical to horizontal!
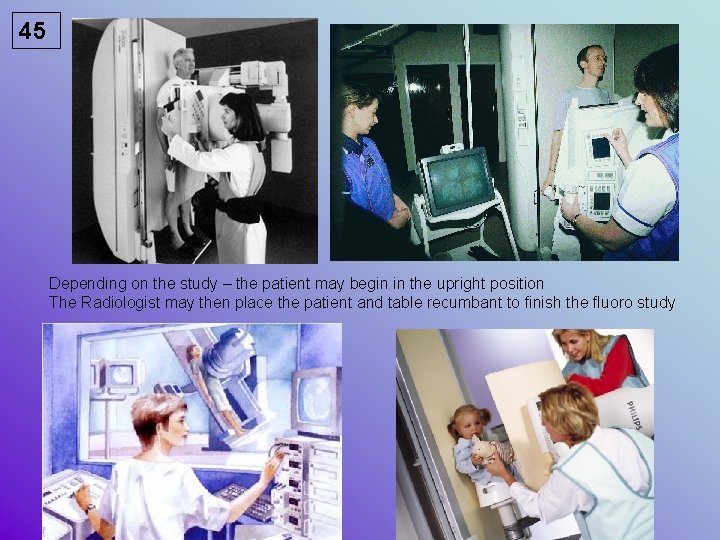
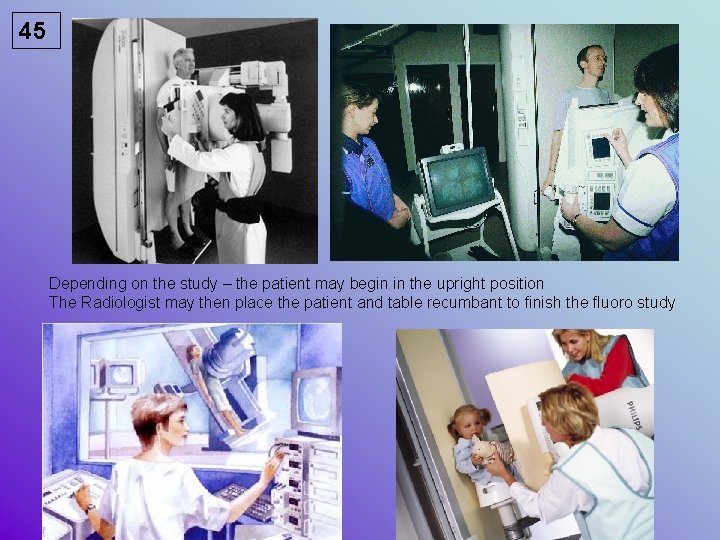
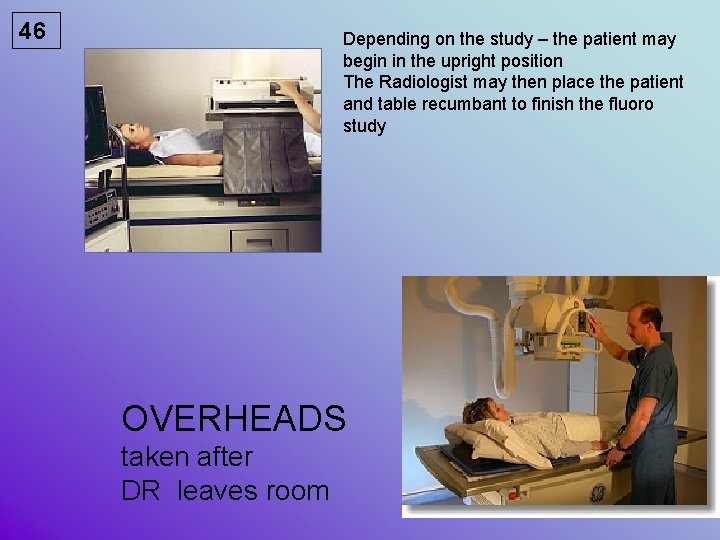
45 Depending on the study – the patient may begin in the upright position The Radiologist may then place the patient and table recumbant to finish the fluoro study
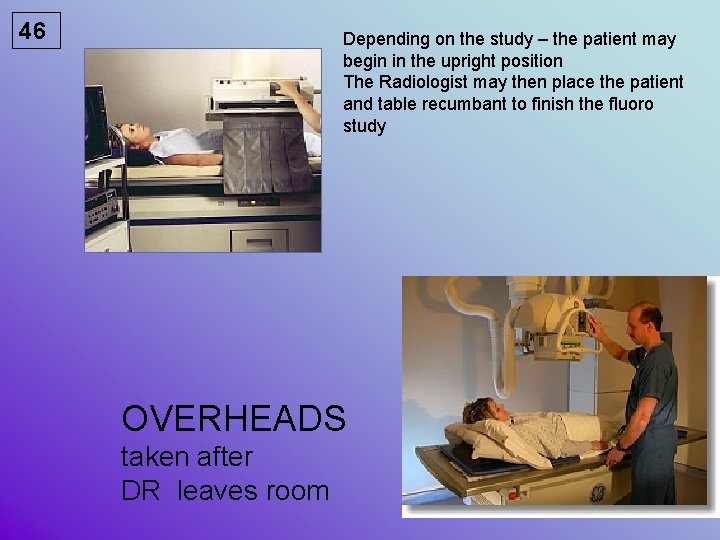
46 Depending on the study – the patient may begin in the upright position The Radiologist may then place the patient and table recumbant to finish the fluoro study OVERHEADS taken after DR leaves room
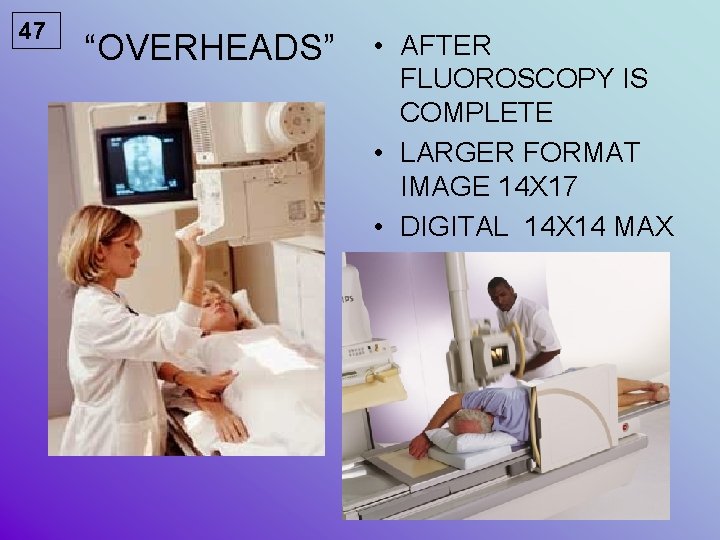
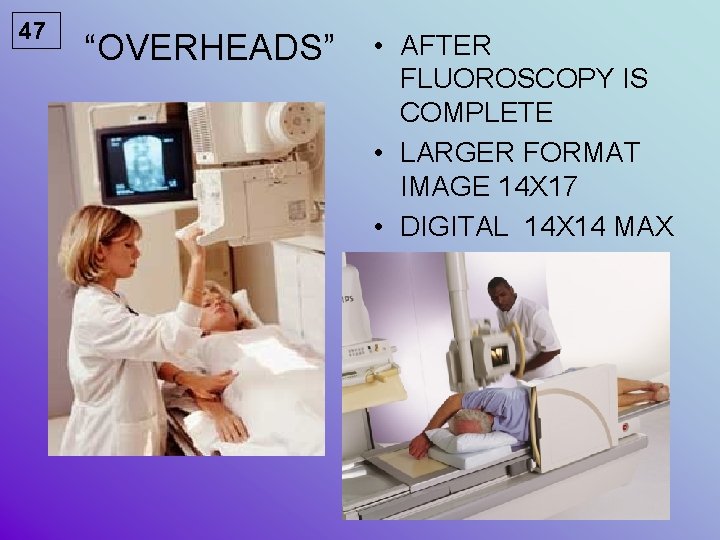
47 “OVERHEADS” • AFTER FLUOROSCOPY IS COMPLETE • LARGER FORMAT IMAGE 14 X 17 • DIGITAL 14 X 14 MAX
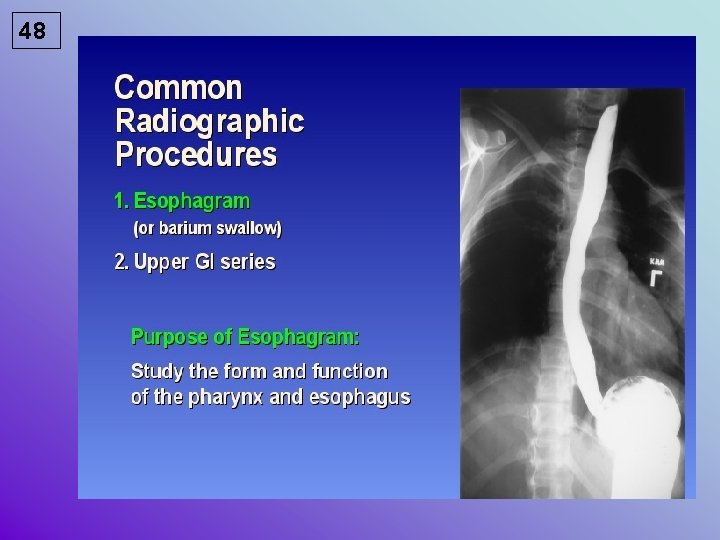
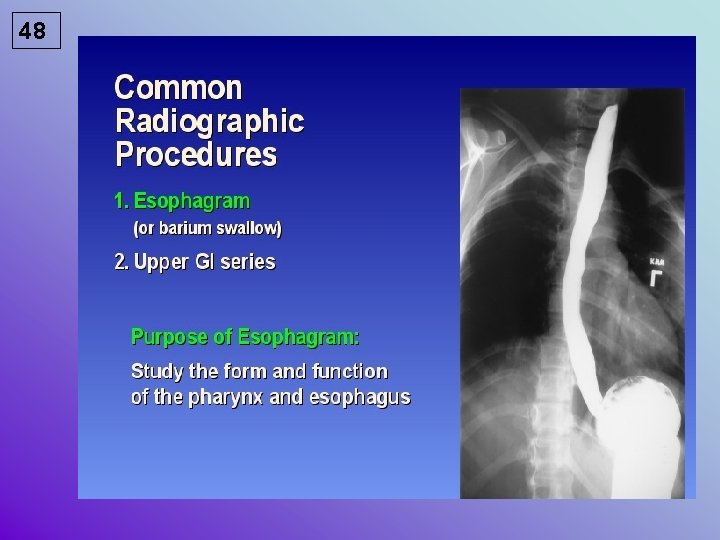
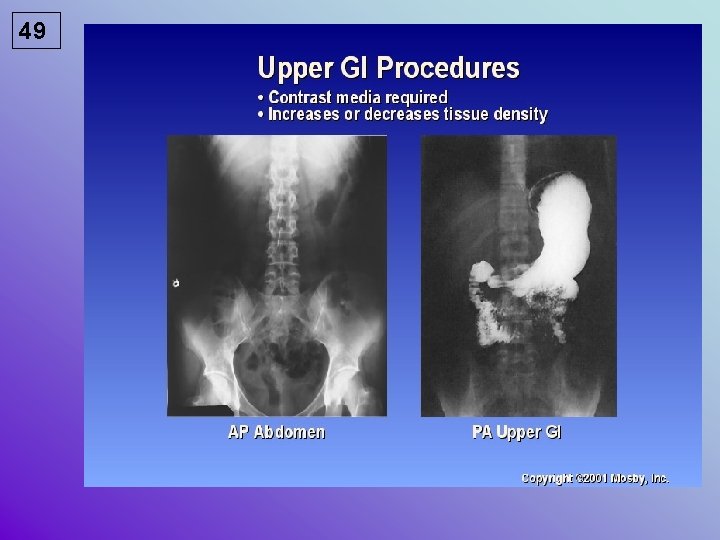
48
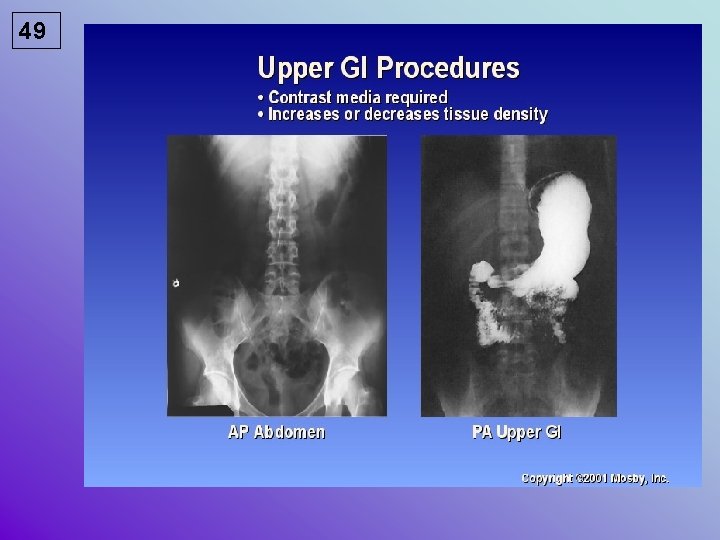
49
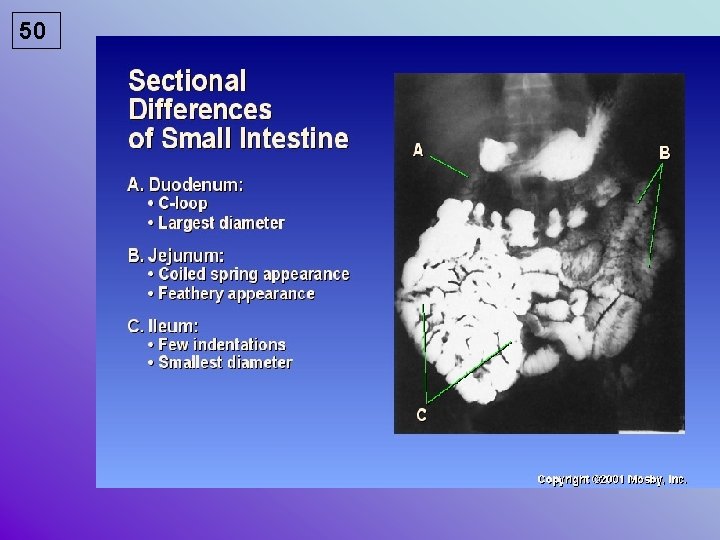
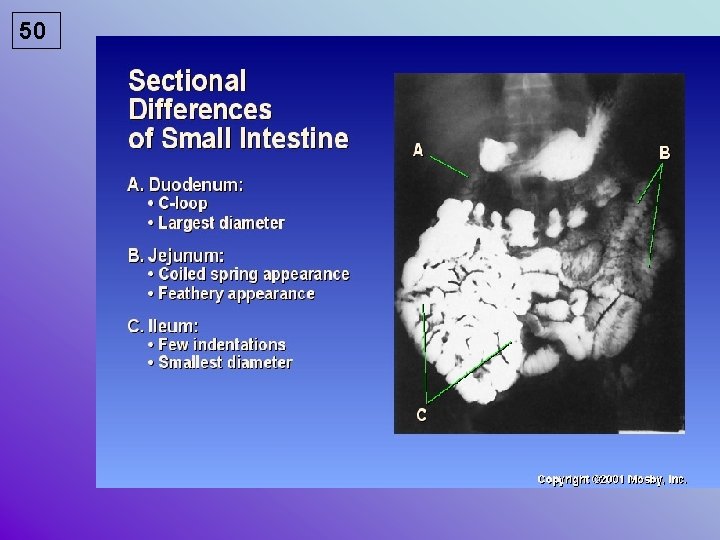
50
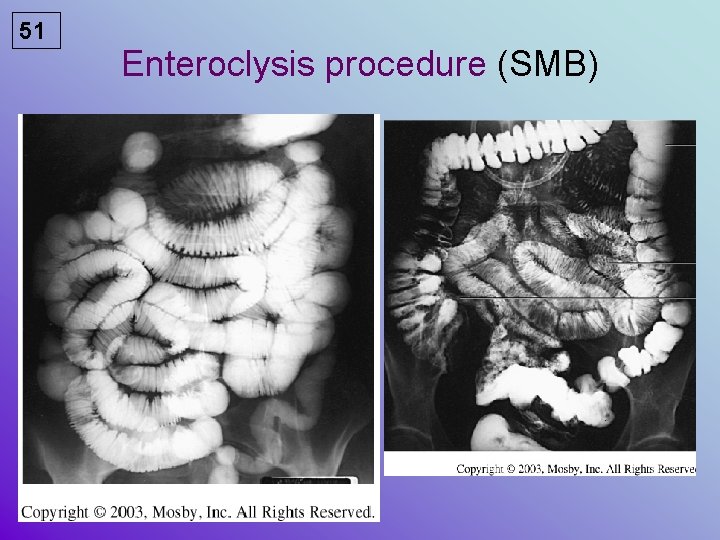
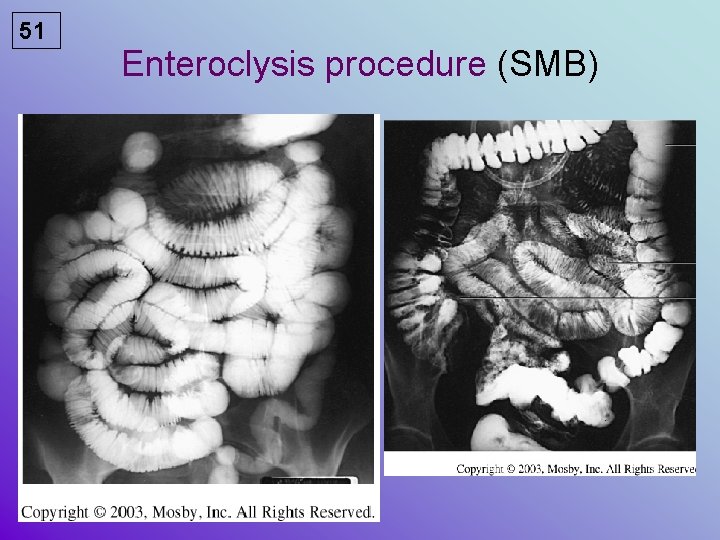
51 Enteroclysis procedure (SMB)

52 Single contrast Double Contrast
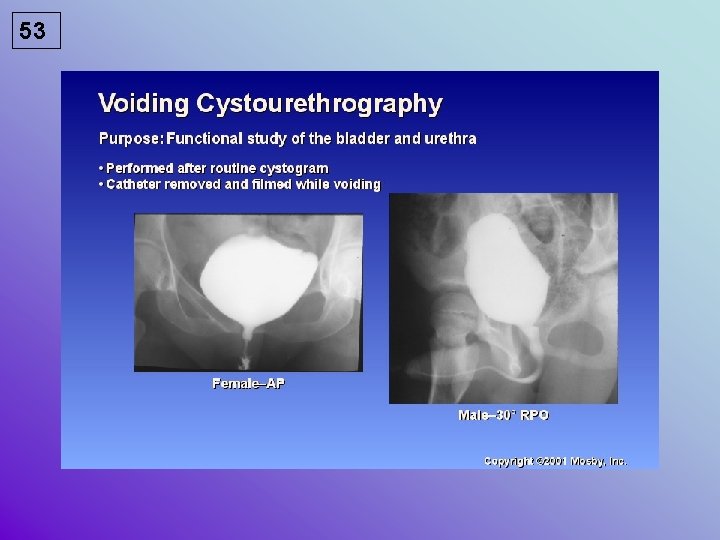
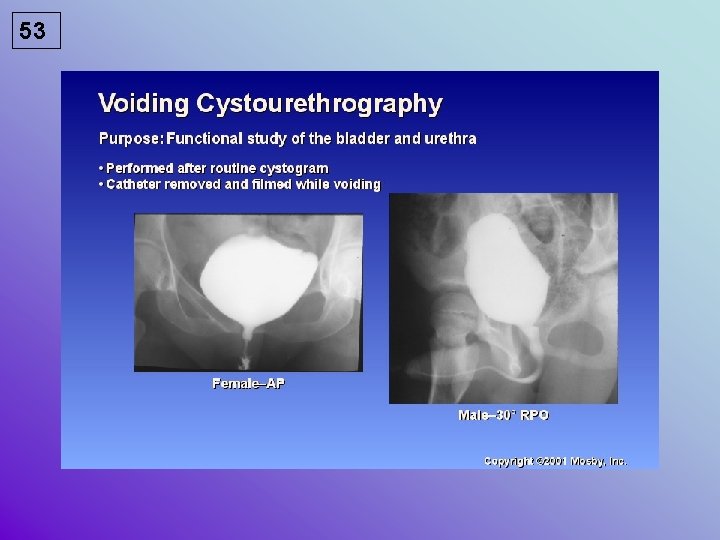
53

54 PROCEDURE? ? ?
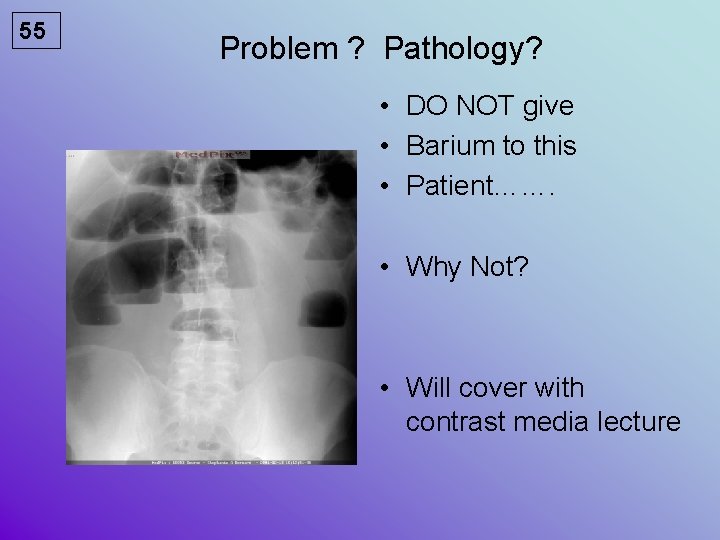
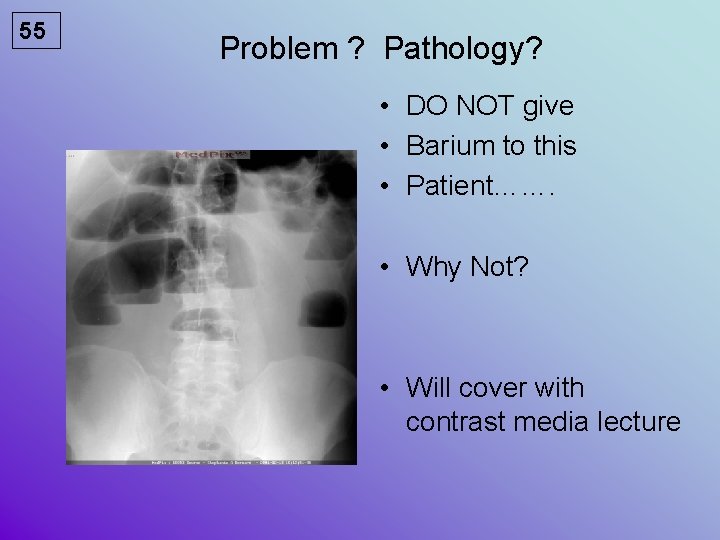
55 Problem ? Pathology? • DO NOT give • Barium to this • Patient……. • Why Not? • Will cover with contrast media lecture
 Digital fluoroscopy vs conventional fluoroscopy
Digital fluoroscopy vs conventional fluoroscopy Real time fluoroscopy
Real time fluoroscopy Bronchoscopy with fluoroscopy
Bronchoscopy with fluoroscopy Photo spot camera in fluoroscopy
Photo spot camera in fluoroscopy Carm fluoroscopy
Carm fluoroscopy Radiation safety
Radiation safety Radiation safety
Radiation safety Background radiation
Background radiation Radiation safety
Radiation safety 340 ucas points
340 ucas points Greatest common factor of 19
Greatest common factor of 19 Adorai o rei do universo harpa cristã
Adorai o rei do universo harpa cristã Buderus u 124
Buderus u 124 As lições do salmo 124
As lições do salmo 124 Art. 124 cpa
Art. 124 cpa In 124
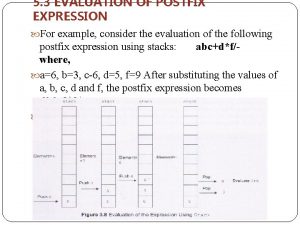
In 124 Evaluate the postfix expression: 562 +*124/
Evaluate the postfix expression: 562 +*124/ Liedboek 124
Liedboek 124 Pohon faktor 92
Pohon faktor 92 Slimbad
Slimbad Ece 124
Ece 124 Bill 124
Bill 124 Project 124
Project 124 Ors 124
Ors 124 Uml inner class
Uml inner class Rev 124
Rev 124 124 binario
124 binario For all your inquiries
For all your inquiries 124 kilos
124 kilos Iec tc 124
Iec tc 124 Subtract 329 from -124
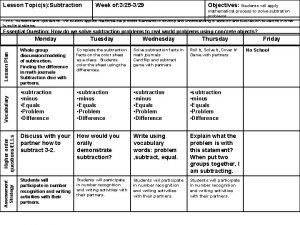
Subtract 329 from -124 Ecdis safety settings
Ecdis safety settings Safety care behavioral safety training
Safety care behavioral safety training Personal safety vs process safety
Personal safety vs process safety Safety assessment for ind safety reporting
Safety assessment for ind safety reporting Basic safety (construction site safety orientation)
Basic safety (construction site safety orientation) Basic safety orientation
Basic safety orientation How electricity works
How electricity works Electrical safety introduction
Electrical safety introduction Module 1 introduction to food safety
Module 1 introduction to food safety Internet safety introduction
Internet safety introduction Food safety questions
Food safety questions Introduction to laboratory safety
Introduction to laboratory safety Grid controlled x ray tube
Grid controlled x ray tube Nhti radiation therapy
Nhti radiation therapy Cancer treatment
Cancer treatment What does conduction
What does conduction Let rbe oer
Let rbe oer Examples of rhythm in fashion
Examples of rhythm in fashion Greenhouse effect long and shortwave radiation
Greenhouse effect long and shortwave radiation Mechanism of uv radiation
Mechanism of uv radiation Solar radiation has a part in the water cycle by
Solar radiation has a part in the water cycle by Reflected radiation formula
Reflected radiation formula Skew t log p
Skew t log p Radiation intensity of antenna
Radiation intensity of antenna What is a semiconductor used for
What is a semiconductor used for