1 FQHC and Residency Partnerships for Financial Sustainability
1 FQHC and Residency Partnerships for Financial Sustainability: Paying the Mortgage for the Patient Centered Medical Home Chris Hiromura, MD James Douglas, MHA/Ph. D
2 Disclosure • For the last several Jim Douglas years has acted as a consultant to residency programs in the Los Angeles area, considering FQHC partnerships
3 Challenges in financing residency programs? • How many of your programs have experienced financial challenges/strains due to: ▫ Hospital budgetary cuts? ▫ Challenges in the recruitment and retention of physician faculty? Behavioralists? Nutritionists? ▫ Designated physical space for resident practice? ▫ Service to disproportionately large “poor-paying” insurance populations such as Medicaid
4 Exploring other business models? • How many of your programs have considered or been through some type of practice restructuring to improve the financial stability of your residency program? ▫ ▫ FQHC or other community partnerships? Limiting patients with certain types of insurance? Foundation D clinic model? Non-profit? Have not felt the need, our program is financially stable?
5 How we got to this point • There was a FMRP that was doing great… ▫ 5 yr RRC approval for four consecutive cycles ▫ Statewide awards for successfully placing physicians in underserved communities ▫ The flagship residency program for the Hospital ▫ Successfully generating millions in grants • Then a hospital consultant came… ▫ Budget cuts soon followed ▫ The cuts would have a significant effect on the ability to continue delivering high quality training
6 How we got to this point? • 25% budget cut to the White Memorial FMRP • The $600, 000 physical site residency expense had to be underwritten by the private faculty practice • CAFP: California Residency Funding Task Force ▫ Significant number of residency programs reported operating deficits ▫ Tendency to treat large Medicaid patient populations ▫ Many programs under significant financial strain
7 Objectives • Accept the premise that FQHC an ideal funding structure for the PCMH • Understand how an FQHC can be the answer to several significant challenges unique to FMRP • Appreciate the basic governance and finance structure of FQHC’s • Obtain sufficient understanding of FQHC’s to know if a partnership might benefit your residency • Return to your residency program and discuss the applicability of this concept with one other faculty member
8 FQHC’s are an ideal financing structure for the Patient Centered Medical Home • Problem with the PCMH is the lack of compensation for the PCMH elements • FQHC’s, with their cost-based reimbursement methodology, can get reimbursed for a number of the elements of the PCMH (FQHC status should not be sought, simply to get PCMH compensation)
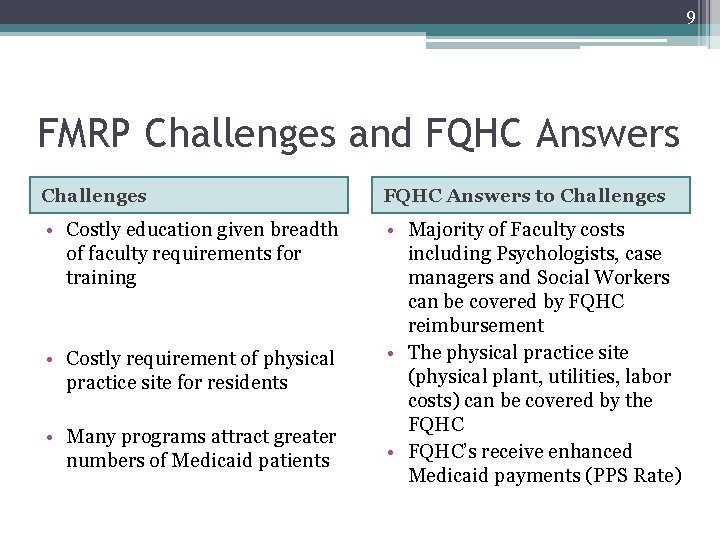
9 FMRP Challenges and FQHC Answers Challenges FQHC Answers to Challenges • Costly education given breadth of faculty requirements for training • Majority of Faculty costs including Psychologists, case managers and Social Workers can be covered by FQHC reimbursement • The physical practice site (physical plant, utilities, labor costs) can be covered by the FQHC • FQHC’s receive enhanced Medicaid payments (PPS Rate) • Costly requirement of physical practice site for residents • Many programs attract greater numbers of Medicaid patients
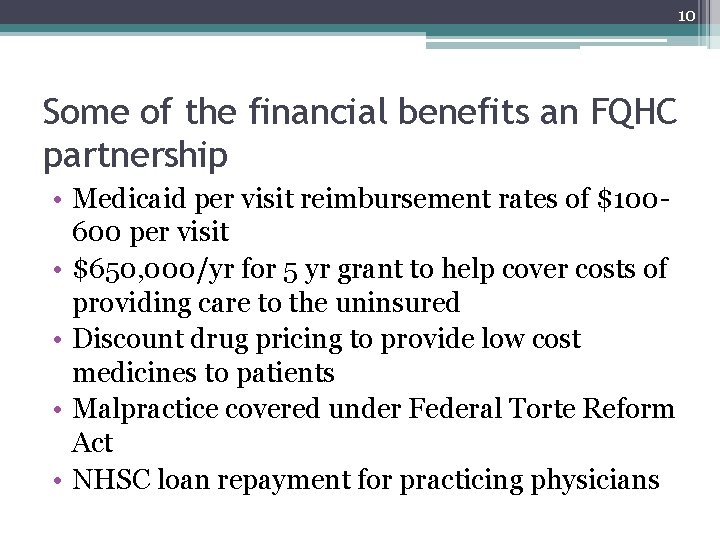
10 Some of the financial benefits an FQHC partnership • Medicaid per visit reimbursement rates of $100600 per visit • $650, 000/yr for 5 yr grant to help cover costs of providing care to the uninsured • Discount drug pricing to provide low cost medicines to patients • Malpractice covered under Federal Torte Reform Act • NHSC loan repayment for practicing physicians
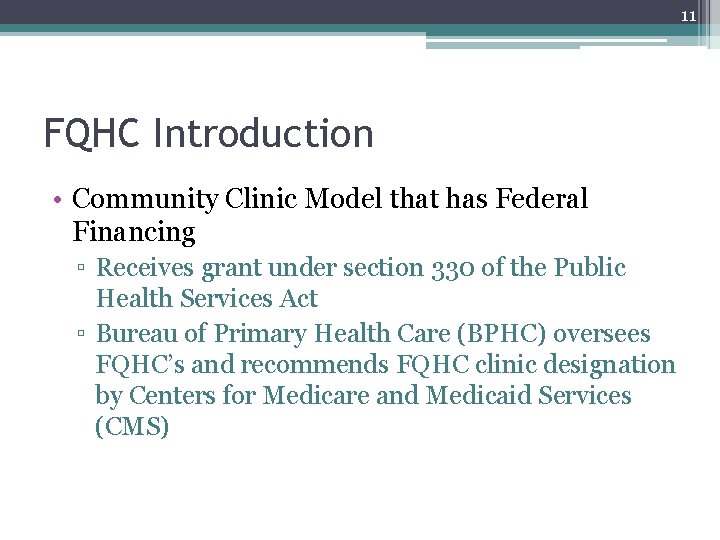
11 FQHC Introduction • Community Clinic Model that has Federal Financing ▫ Receives grant under section 330 of the Public Health Services Act ▫ Bureau of Primary Health Care (BPHC) oversees FQHC’s and recommends FQHC clinic designation by Centers for Medicare and Medicaid Services (CMS)
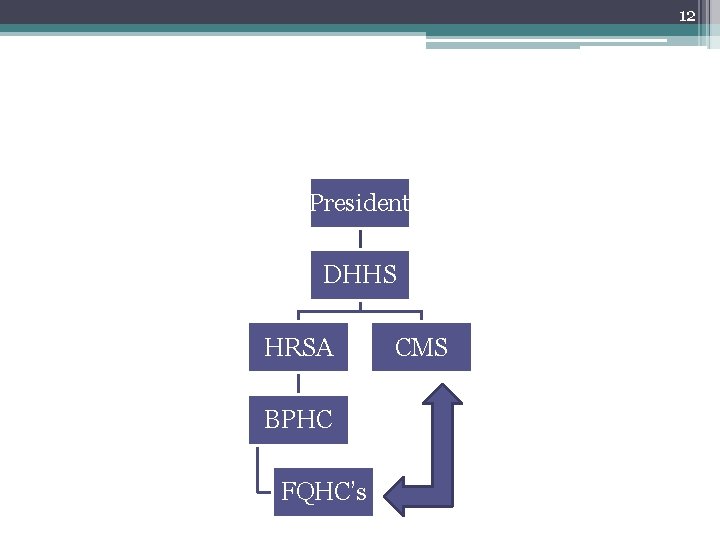
12 President DHHS HRSA BPHC FQHC’s CMS
13 FQHC’s Success in Underserved Populations • Thrive in high volume Medicaid populations • Bipartisan support ▫ Expanded under GW Bush by 1, 297 new clinics or access points, a 50% increase ▫ Further expansion under the Obama administration with ARRA and Health Reform (11 billion for New Access Points)
14 FQHC’s: Governance • Governance ▫ Oversight by Board of Directors: 9 -25 members, 51% of the BOD have to be patients of the clinic
15 FQHC’s: Finance • Finance ▫ $650, 000/yr for 5 yrs (renewable) to help cover uninsured patients ▫ Prospective Payment System Rate (PPS rate) �Can vary from $100 -600 per visit for each Medicaid visit �The enhanced payment offsets costs of care for uninsured patients ▫ Obligation to see the uninsured �Charge a sliding scale fee
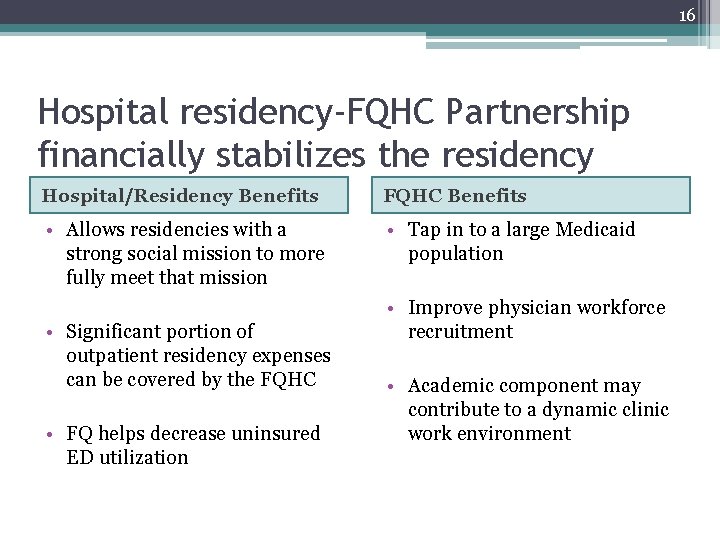
16 Hospital residency-FQHC Partnership financially stabilizes the residency Hospital/Residency Benefits FQHC Benefits • Allows residencies with a strong social mission to more fully meet that mission • Tap in to a large Medicaid population • Significant portion of outpatient residency expenses can be covered by the FQHC • FQ helps decrease uninsured ED utilization • Improve physician workforce recruitment • Academic component may contribute to a dynamic clinic work environment
17 Teaching Health Center Model • Demonstration project part of health care reform • FQHC’s will host the primary care residency program rather than hospitals • Will receive GME funding (formula yet to be determined) • Stay on the look out for this new model of care
18 Health care reform and FQHCResidency Partnerships • Now is the time to consider these partnerships ▫ Billions available for FQHC’s to expand to New Access Points ▫ NACHC very interested and supportive of the idea of residency partnerships to help meet CHC provider demand ▫ Possibility of THC’s
19 Potential Challenges to Partnering with an FQHC • Make sure that the leadership from both the FQHC and the residency support each others mission and the affiliated hospital • Cautious of the mentality that “if you aren’t losing money, you aren’t doing God’s work”. • Dealing with both ACGME regulations and FQHC federal regulations
20 What are the next steps I should take? • Consider how the benefits of FQHC partnership might support your residency program • Read the articles provided • Discuss the possibility of FQHC partnership with at least one other member of your faculty • Check FQHC’s/RHC’s in your area to find potential partners • You will need a project manager, lawyer, grant writer and an accountant well versed in FQHC regulations to shepherd the process • Please feel free to contact us with any questions along the way
21 Questions • Any questions about the FQHC model in general? • Any questions about linkages between an existing FQHC and a hospital based residency? • Any questions on the THC model? • Any questions on how health care reform might impact these care models? • Any questions on the legal or political issues in developing these linkages?
22 FQHC Reading List • “FQHC Fact Sheet”. Family Care Specialists 2010 • FQHC’s: A new look at a venerable model? ? • Leifer, JC, Golde MD. Key Considerations in Developing Residency Training Program Collaborations. The National Association of Community Health Centers, Issue Brief #26, April, 2004 • Morris CG, Chen FM. Training Residents in Community Health Centers: Facilitators and Barriers. Ann of Fam Med 2009; 7: 488 -494 • Mullan F, Chen C, Wiley, E. The Case For Teaching Health Centers. Medical Education Futures Study – Policy Brief, July 2009
23 Thank You chrishiromura@gmail. com jim@jhdassociates. net
- Slides: 23