1 Classification of diabetes WHO ADA etc Type

1

Classification of diabetes (WHO, ADA etc. ) Type 1 diabetes (due to β-cell destruction, usually leading to absolute insulin deficiency) Type 2 diabetes (due to a progressive insulin secretory defect on the background of insulin resistance) Diabetes due to other causes: Genetic defects in β-cell function, genetic defects in insulin action, diseases of the exocrine pancreas (such as cystic fibrosis), and drug- or chemical-induced (such as in the treatment of HIV/AIDS or after organ transplantation) Gestational diabetes mellitus (GDM) (diabetes diagnosed during pregnancy that is not clearly overt diabetes)
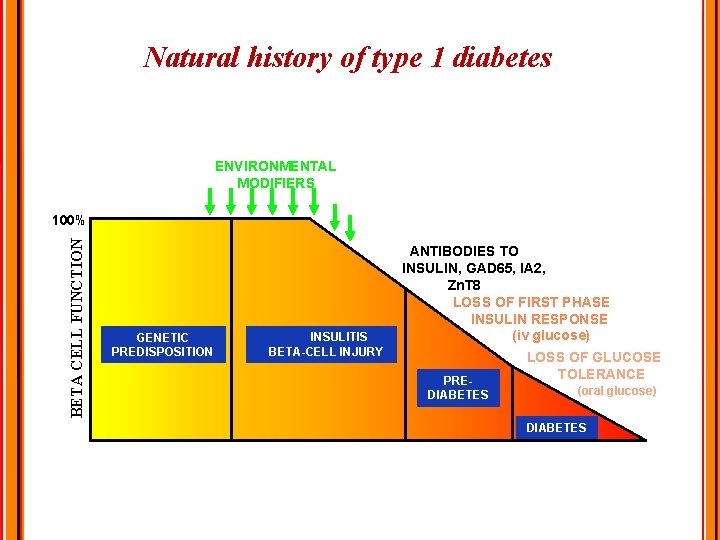
Natural history of type 1 diabetes ENVIRONMENTAL MODIFIERS BETA CELL FUNCTION 100% GENETIC PREDISPOSITION ANTIBODIES TO INSULIN, GAD 65, IA 2, Zn. T 8 LOSS OF FIRST PHASE INSULIN RESPONSE (iv glucose) INSULITIS BETA-CELL INJURY PREDIABETES LOSS OF GLUCOSE TOLERANCE (oral glucose) DIABETES Years
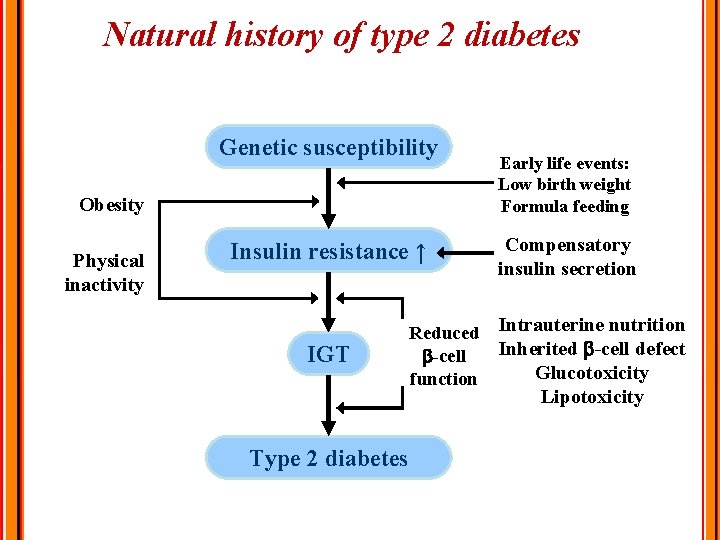
Natural history of type 2 diabetes Genetic susceptibility Obesity Physical inactivity Insulin resistance ↑ IGT Early life events: Low birth weight Formula feeding Compensatory insulin secretion Reduced Intrauterine nutrition Inherited -cell defect -cell Glucotoxicity function Lipotoxicity Type 2 diabetes
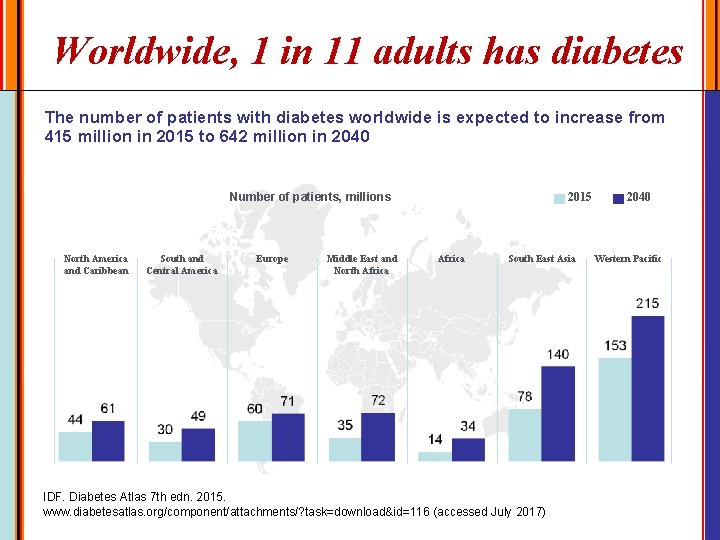
Worldwide, 1 in 11 adults has diabetes The number of patients with diabetes worldwide is expected to increase from 415 million in 2015 to 642 million in 2040 Number of patients, millions North America and Caribbean South and Central America Europe Middle East and North Africa 2015 Africa South East Asia IDF. Diabetes Atlas 7 th edn. 2015. www. diabetesatlas. org/component/attachments/? task=download&id=116 (accessed July 2017) 2040 Western Pacific
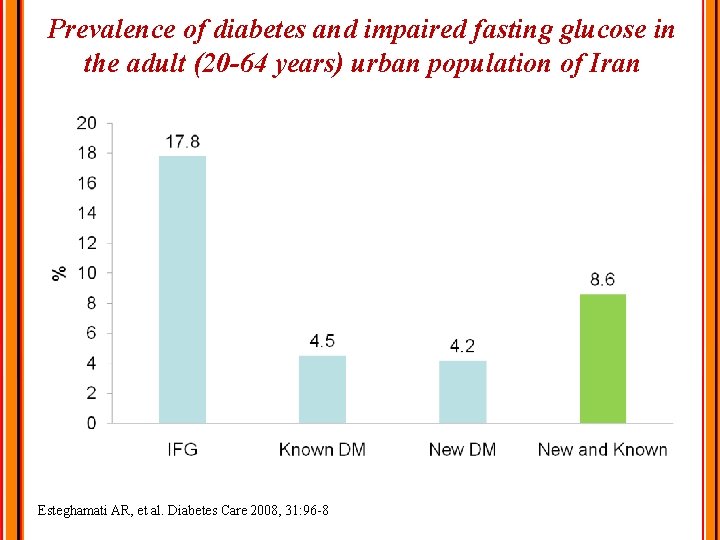
Prevalence of diabetes and impaired fasting glucose in the adult (20 -64 years) urban population of Iran Esteghamati AR, et al. Diabetes Care 2008, 31: 96 -8
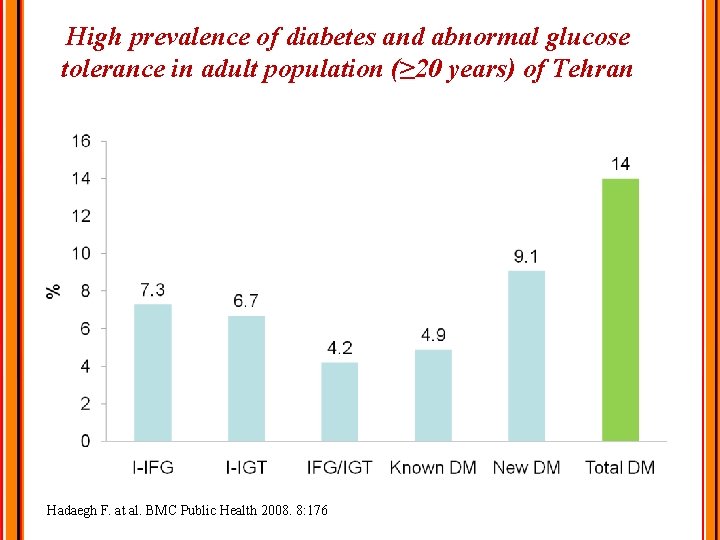
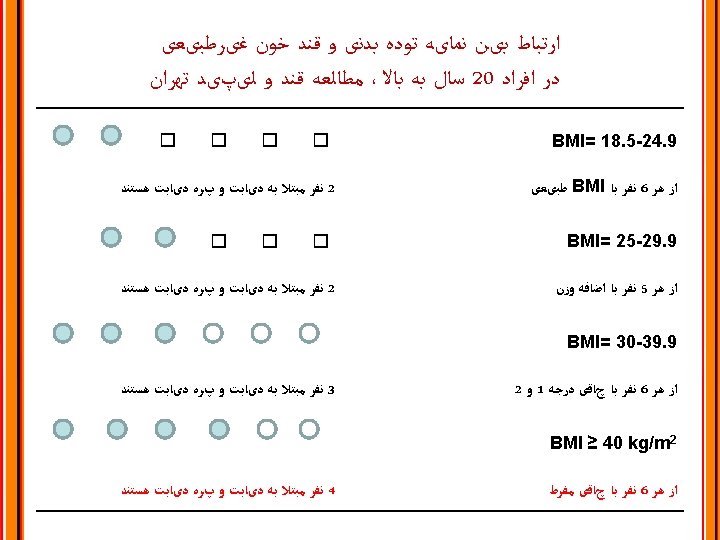
High prevalence of diabetes and abnormal glucose tolerance in adult population (≥ 20 years) of Tehran Hadaegh F. at al. BMC Public Health 2008. 8: 176
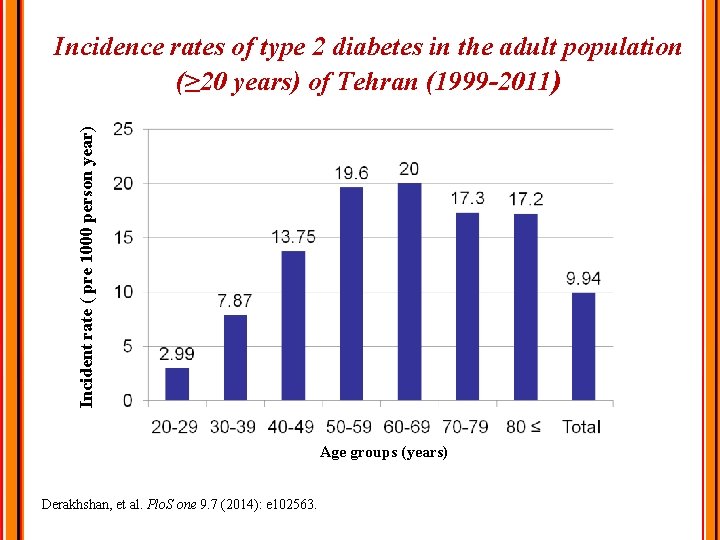
Incident rate ( pre 1000 person year) Incidence rates of type 2 diabetes in the adult population (≥ 20 years) of Tehran (1999 -2011) Age groups (years) Derakhshan, et al. Plo. S one 9. 7 (2014): e 102563.
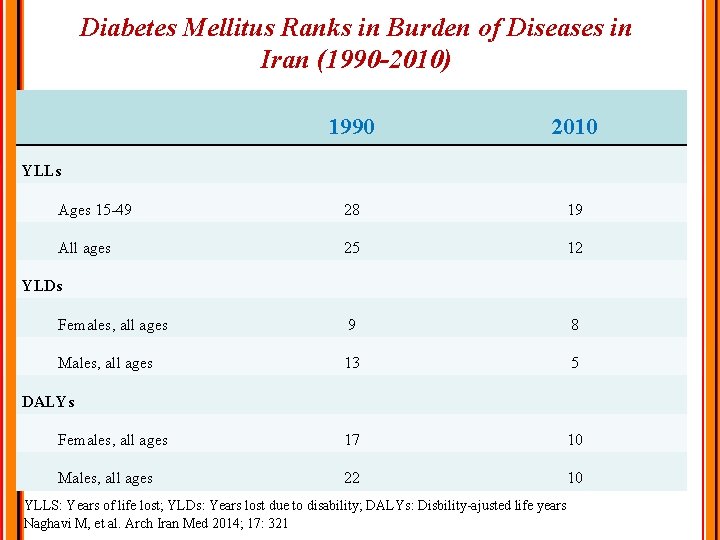
Diabetes Mellitus Ranks in Burden of Diseases in Iran (1990 -2010) 1990 2010 Ages 15 -49 28 19 All ages 25 12 Females, all ages 9 8 Males, all ages 13 5 Females, all ages 17 10 Males, all ages 22 10 YLLs YLDs DALYs YLLS: Years of life lost; YLDs: Years lost due to disability; DALYs: Disbility-ajusted life years Naghavi M, et al. Arch Iran Med 2014; 17: 321
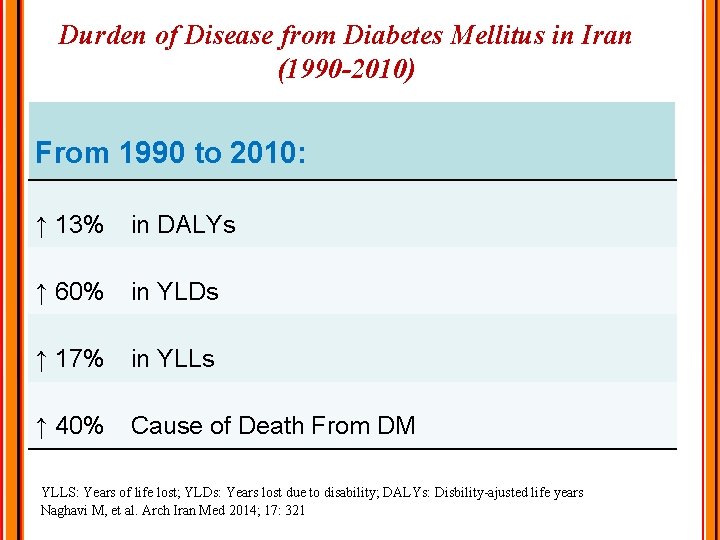
Durden of Disease from Diabetes Mellitus in Iran (1990 -2010) From 1990 to 2010: ↑ 13% in DALYs ↑ 60% in YLDs ↑ 17% in YLLs ↑ 40% Cause of Death From DM YLLS: Years of life lost; YLDs: Years lost due to disability; DALYs: Disbility-ajusted life years Naghavi M, et al. Arch Iran Med 2014; 17: 321
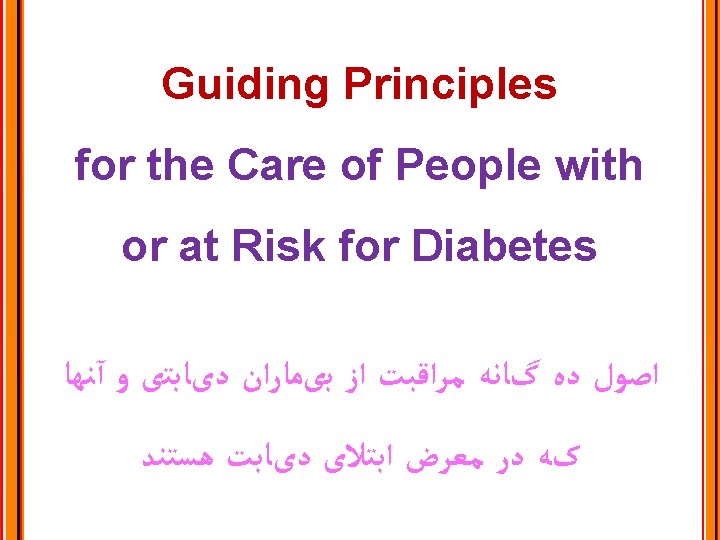
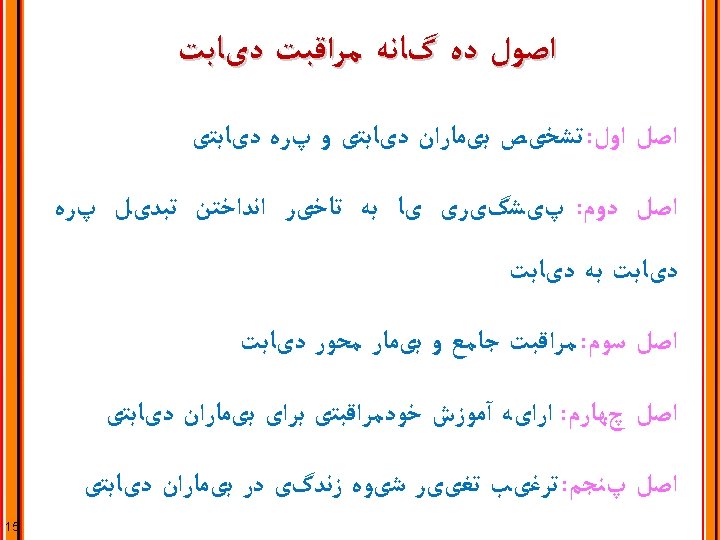
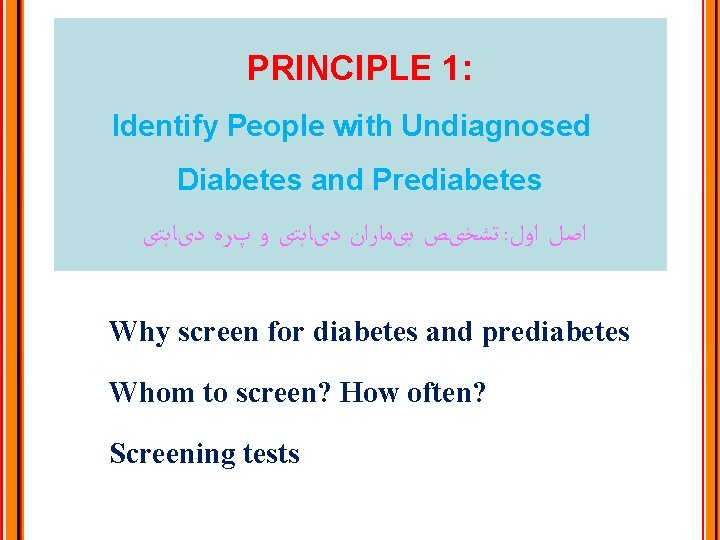
PRINCIPLE 1: Identify People with Undiagnosed Diabetes and Prediabetes ﺗﺸﺨیﺺ ﺑیﻤﺎﺭﺍﻥ ﺩیﺎﺑﺘی ﻭ پﺮﻩ ﺩیﺎﺑﺘی : ﺍﺻﻞ ﺍﻭﻝ Why screen for diabetes and prediabetes Whom to screen? How often? Screening tests
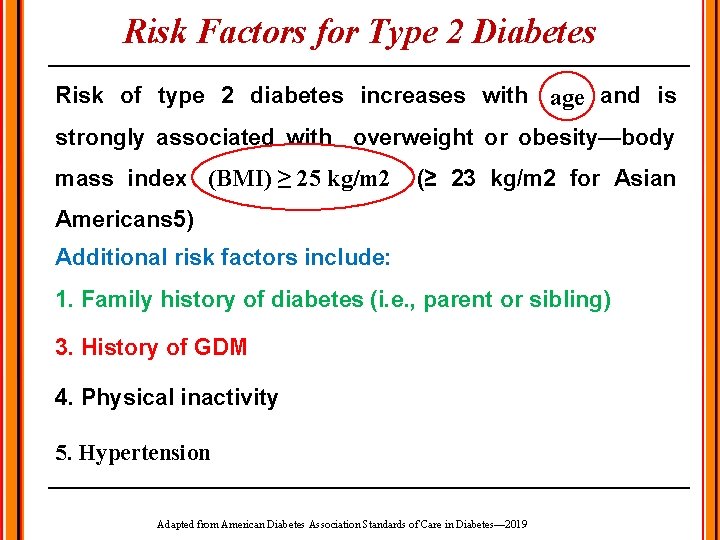
Risk Factors for Type 2 Diabetes Risk of type 2 diabetes increases with age and is strongly associated with overweight or obesity—body (BMI)≥ ≥ 25 mass index (BMI) 25 kg/m 2 (≥ 23 kg/m 2 for Asian Americans 5) Additional risk factors include: 1. Family history of diabetes (i. e. , parent or sibling) 3. History of GDM 4. Physical inactivity 5. Hypertension Adapted from American Diabetes Association Standards of Care in Diabetes— 2019
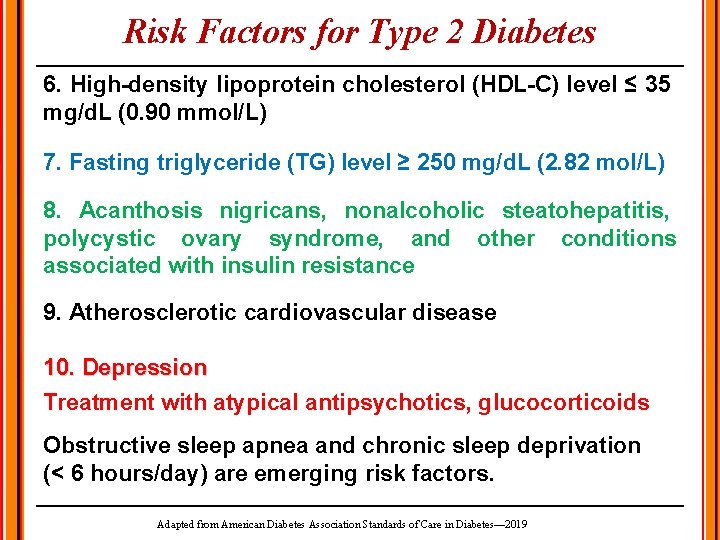
Risk Factors for Type 2 Diabetes 6. High-density lipoprotein cholesterol (HDL-C) level ≤ 35 mg/d. L (0. 90 mmol/L) 7. Fasting triglyceride (TG) level ≥ 250 mg/d. L (2. 82 mol/L) 8. Acanthosis nigricans, nonalcoholic steatohepatitis, polycystic ovary syndrome, and other conditions associated with insulin resistance 9. Atherosclerotic cardiovascular disease 10. Depression Treatment with atypical antipsychotics, glucocorticoids Obstructive sleep apnea and chronic sleep deprivation (< 6 hours/day) are emerging risk factors. Adapted from American Diabetes Association Standards of Care in Diabetes— 2019
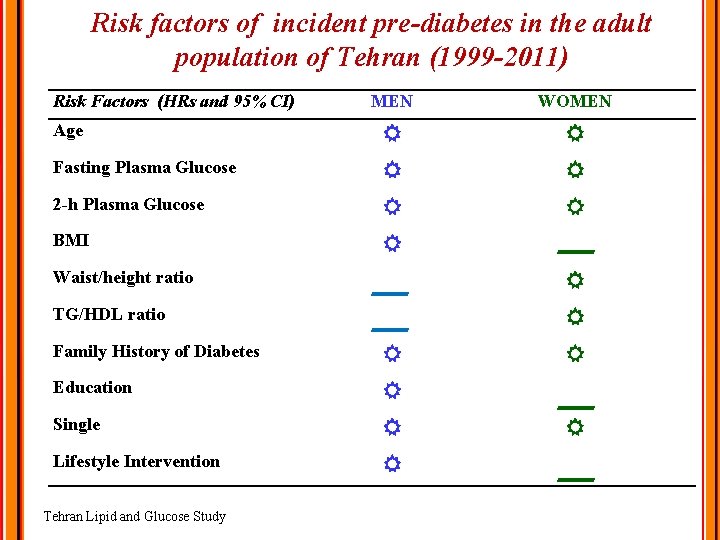
Risk factors of incident pre-diabetes in the adult population of Tehran (1999 -2011) Risk Factors (HRs and 95% CI) MEN WOMEN Age Fasting Plasma Glucose 2 -h Plasma Glucose BMI Waist/height ratio TG/HDL ratio Family History of Diabetes Education Single Lifestyle Intervention Tehran Lipid and Glucose Study
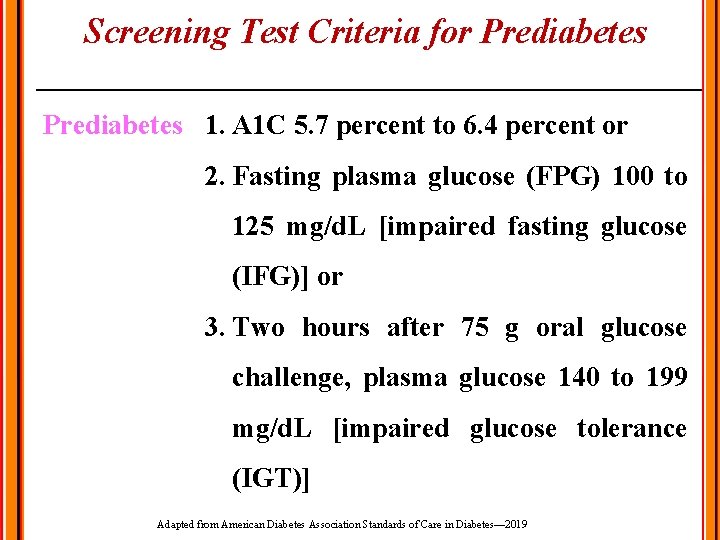
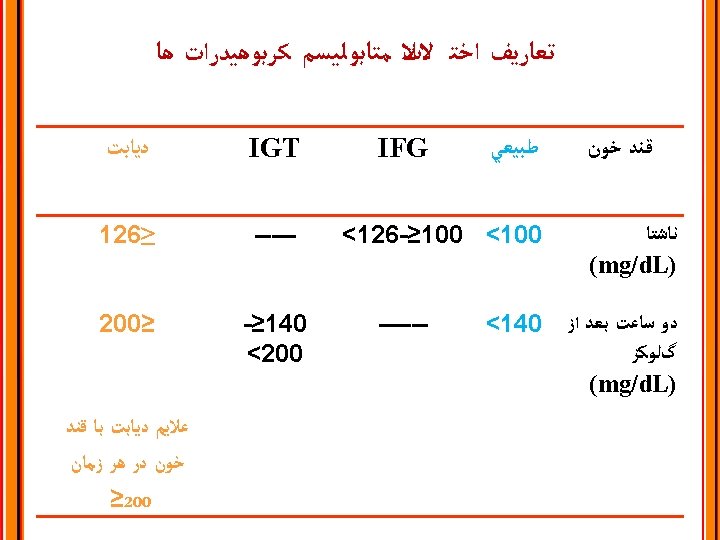
Screening Test Criteria for Prediabetes 1. A 1 C 5. 7 percent to 6. 4 percent or 2. Fasting plasma glucose (FPG) 100 to 125 mg/d. L [impaired fasting glucose (IFG)] or 3. Two hours after 75 g oral glucose challenge, plasma glucose 140 to 199 mg/d. L [impaired glucose tolerance (IGT)] Adapted from American Diabetes Association Standards of Care in Diabetes— 2019
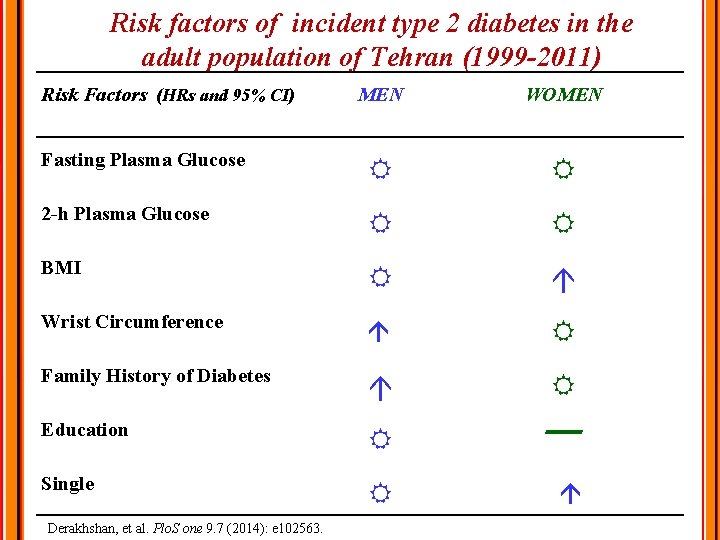
Risk factors of incident type 2 diabetes in the adult population of Tehran (1999 -2011) Risk Factors (HRs and 95% CI) MEN WOMEN Fasting Plasma Glucose 2 -h Plasma Glucose BMI Wrist Circumference Family History of Diabetes Education Single Derakhshan, et al. Plo. S one 9. 7 (2014): e 102563.
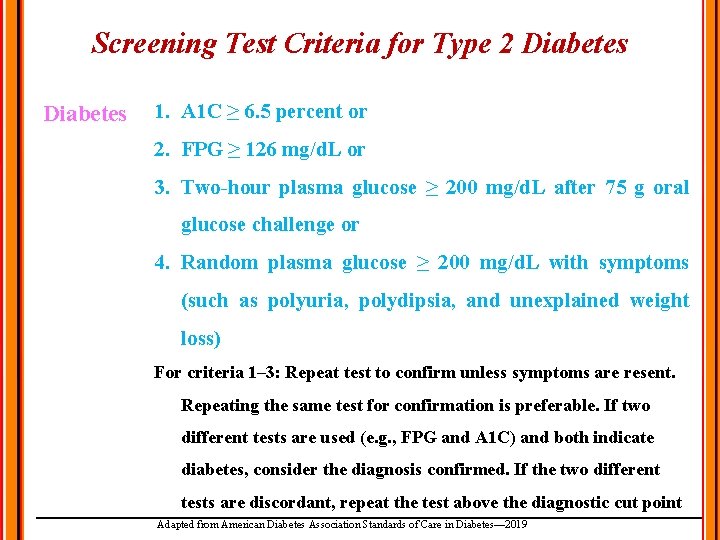
Screening Test Criteria for Type 2 Diabetes 1. A 1 C ≥ 6. 5 percent or 2. FPG ≥ 126 mg/d. L or 3. Two-hour plasma glucose ≥ 200 mg/d. L after 75 g oral glucose challenge or 4. Random plasma glucose ≥ 200 mg/d. L with symptoms (such as polyuria, polydipsia, and unexplained weight loss) For criteria 1– 3: Repeat test to confirm unless symptoms are resent. Repeating the same test for confirmation is preferable. If two different tests are used (e. g. , FPG and A 1 C) and both indicate diabetes, consider the diagnosis confirmed. If the two different tests are discordant, repeat the test above the diagnostic cut point Adapted from American Diabetes Association Standards of Care in Diabetes— 2019
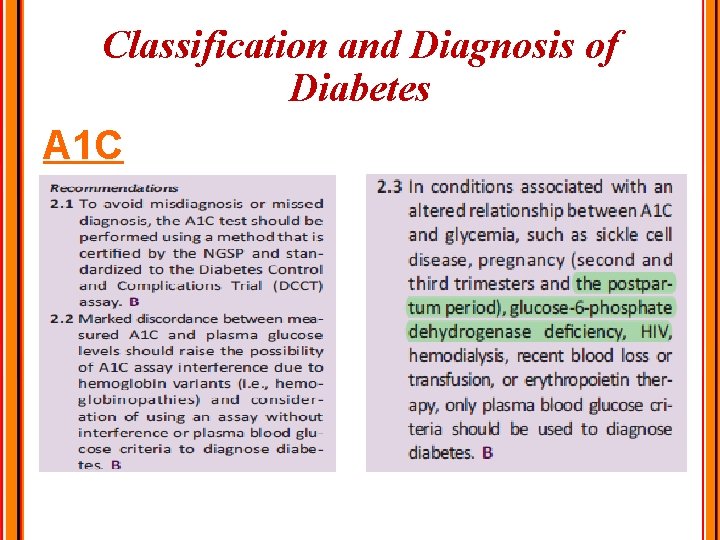
Classification and Diagnosis of Diabetes A 1 C
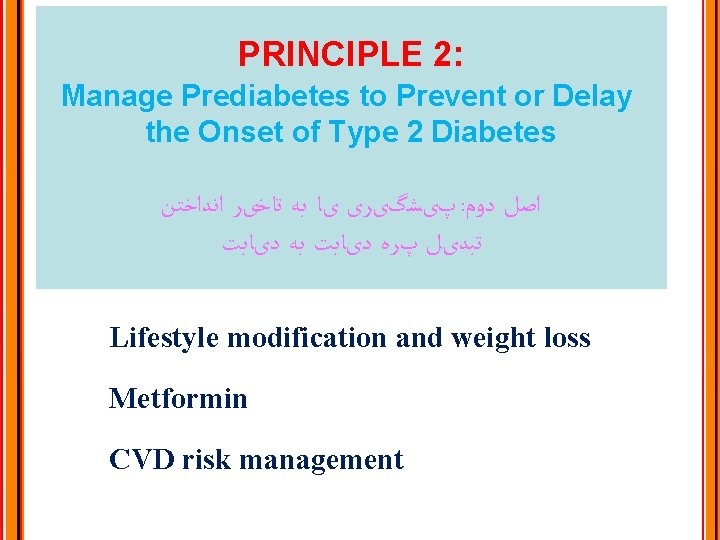
PRINCIPLE 2: Manage Prediabetes to Prevent or Delay the Onset of Type 2 Diabetes پیﺸگیﺮی یﺎ ﺑﻪ ﺗﺎﺧیﺮ ﺍﻧﺪﺍﺧﺘﻦ : ﺍﺻﻞ ﺩﻭﻡ ﺗﺒﺪیﻞ پﺮﻩ ﺩیﺎﺑﺖ ﺑﻪ ﺩیﺎﺑﺖ Lifestyle modification and weight loss Metformin CVD risk management
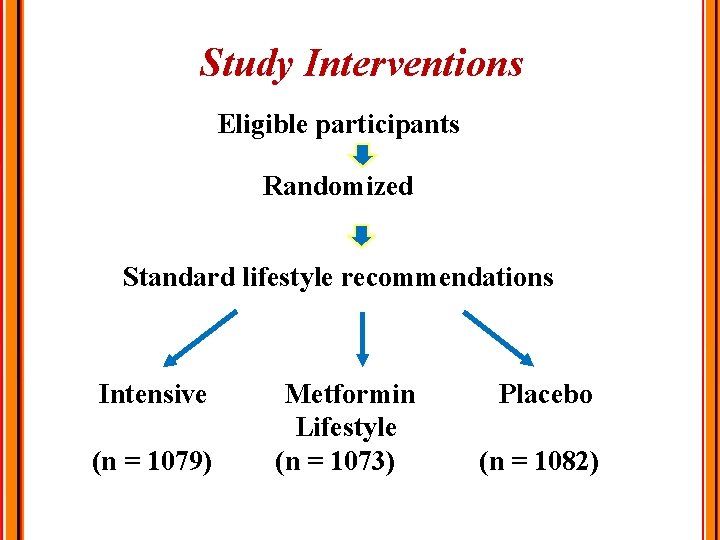
Study Interventions Eligible participants Randomized Standard lifestyle recommendations Intensive (n = 1079) Metformin Lifestyle (n = 1073) Placebo (n = 1082)
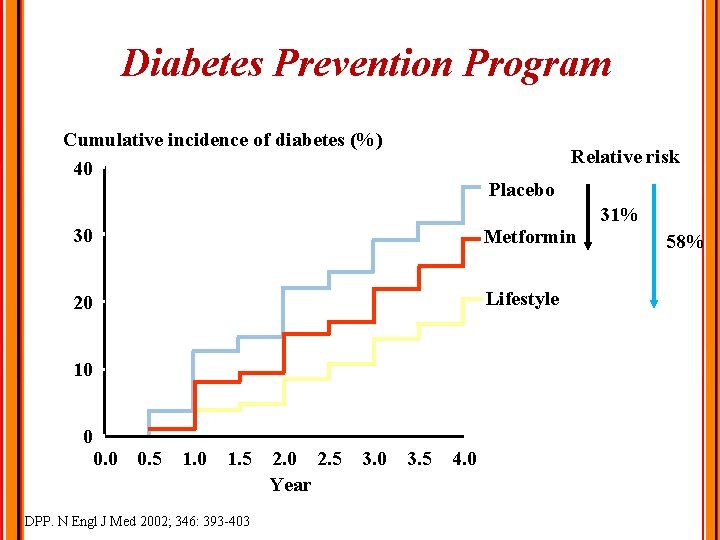
Diabetes Prevention Program Cumulative incidence of diabetes (%) 40 Relative risk Placebo 30 Metformin 20 Lifestyle 10 0 0. 5 1. 0 1. 5 2. 0 2. 5 3. 0 3. 5 4. 0 Year DPP. N Engl J Med 2002; 346: 393 -403 31% 58%
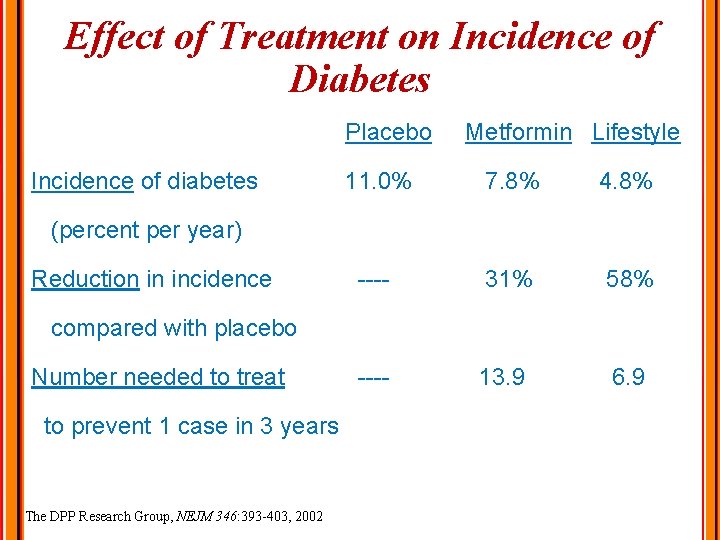
Effect of Treatment on Incidence of Diabetes Placebo Incidence of diabetes Metformin Lifestyle 11. 0% 7. 8% 4. 8% ---- 31% 58% ---- 13. 9 6. 9 (percent per year) Reduction in incidence compared with placebo Number needed to treat to prevent 1 case in 3 years The DPP Research Group, NEJM 346: 393 -403, 2002
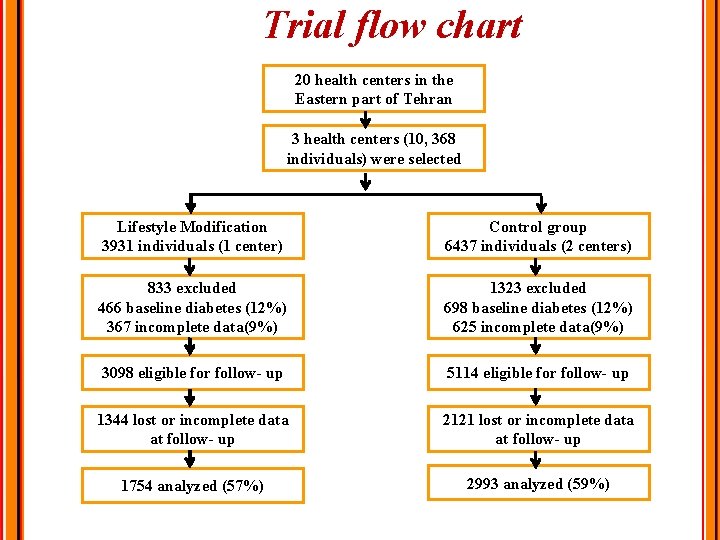
Trial flow chart 20 health centers in the Eastern part of Tehran 3 health centers (10, 368 individuals) were selected Lifestyle Modification 3931 individuals (1 center) Control group 6437 individuals (2 centers) 833 excluded 466 baseline diabetes (12%) 367 incomplete data(9%) 1323 excluded 698 baseline diabetes (12%) 625 incomplete data(9%) 3098 eligible for follow- up 5114 eligible for follow- up 1344 lost or incomplete data at follow- up 2121 lost or incomplete data at follow- up 1754 analyzed (57%) 2993 analyzed (59%)
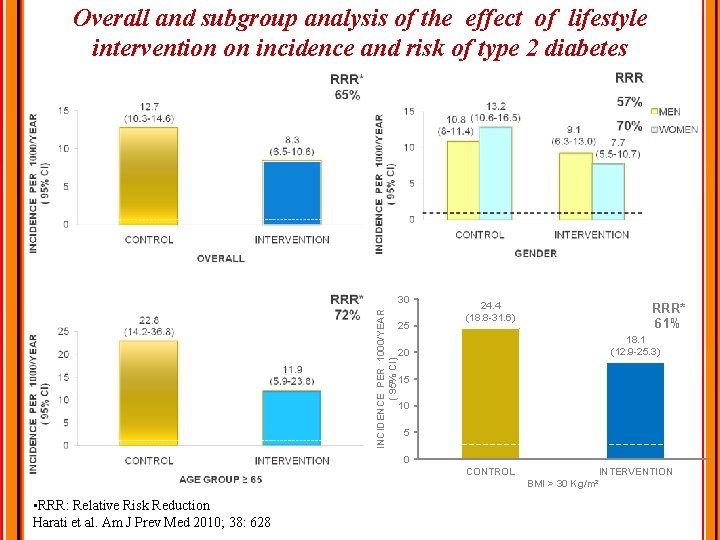
Overall and subgroup analysis of the effect of lifestyle intervention on incidence and risk of type 2 diabetes INCIDENCE PER 1000/YEAR ( 95% CI) 30 25 24. 4 (18. 8 -31. 6) RRR* 61% 18. 1 (12. 9 -25. 3) 20 15 10 5 0 CONTROL • RRR: Relative Risk Reduction Harati et al. Am J Prev Med 2010; 38: 628 INTERVENTION BMI > 30 Kg/m²
Synopsis of recommendations to prevent or delay diabetes: • Individuals at high risk for DM need modest weight loss and a regular physical activity. • Screening: Persons >45 yrs, particularly those with a BMI >25 kg/m 2, are screened to detect pre-diabetes (IFG or IGT). Screening should be considered in younger individuals with a BMI >25 kg/m 2 who have additional risk factors. • In individuals with normoglycemia, rescreening is at 3 -year intervals.
PRINCIPLE 3: Provide Comprehensive, Patient-centered Diabetes Care ﻣﺮﺍﻗﺒﺖ ﺟﺎﻣﻊ ﻭ ﺑیﻤﺎﺭ ﻣﺤﻮﺭ ﺩیﺎﺑﺖ : ﺍﺻﻞ ﺳﻮﻡ Consideration of health literacy and numeracy Consideration of patient-self-management resources Comprehensive management of comorbid conditions: Depression, congnitive impairment, cancer, periodontal disease, liver disease, hearing loss, obstructive sleep apnea, osteoarthritis, infectious diseases
Diabetes mellitus Primary goals of treatment Prevention of morbidity and mortality associated with diabetes • Microvascular complications • Macrovascular complications Improvement of quality of life and self-perceived health status (well being)
PRINCIPLE 4: Provide Ongoing Self-management Education and Support for People with Diabetes ﺍﺭﺍیﻪ آﻤﻮﺯﺵ ﺧﻮﺩﻣﺮﺍﻗﺒﺘی ﺑﺮﺍی ﺑیﻤﺎﺭﺍﻥ ﺩیﺎﺑﺘی : ﺍﺻﻞ چﻬﺎﺭﻡ Definition and purpose of diabetes self management education & support (DSMES) to understand, implement and sustain self management How to provide DSMES? Community based and other resources.
Aim of self-management To understand diabetes pathophysiology and treatment options, and to understand, implement, and sustain: vhealthy eating vphysical activity vmedication usage vmonitoring and using patient-generated health data vpreventing, detecting, and treating acute and chronic complications vhealthy coping with psychosocial issues and concerns vproblem solving vnavigating the health care system vpracticing self-advocacy ve-health education Based on 2017 American Diabetes Association/American Association of Diabetes Educators National Standards
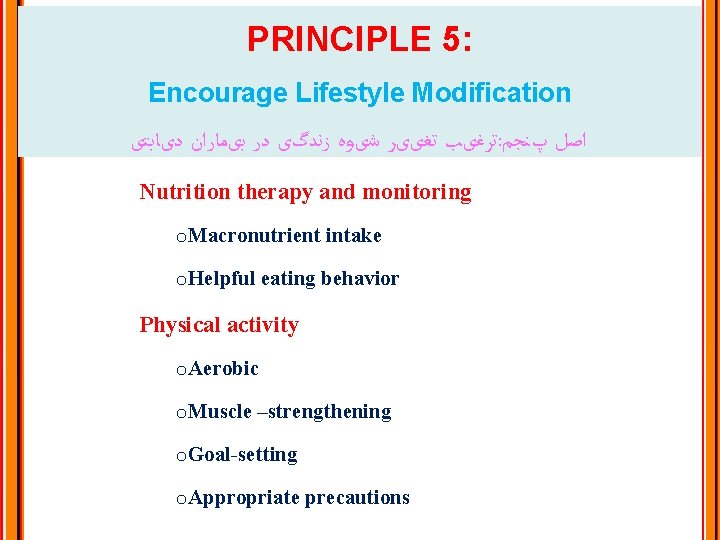
PRINCIPLE 5: Encourage Lifestyle Modification ﺗﺮﻏیﺐ ﺗﻐییﺮ ﺷیﻮﻩ ﺯﻧﺪگی ﺩﺭ ﺑیﻤﺎﺭﺍﻥ ﺩیﺎﺑﺘی : ﺍﺻﻞ پﻨﺠﻢ Nutrition therapy and monitoring o. Macronutrient intake o. Helpful eating behavior Physical activity o. Aerobic o. Muscle –strengthening o. Goal-setting o. Appropriate precautions
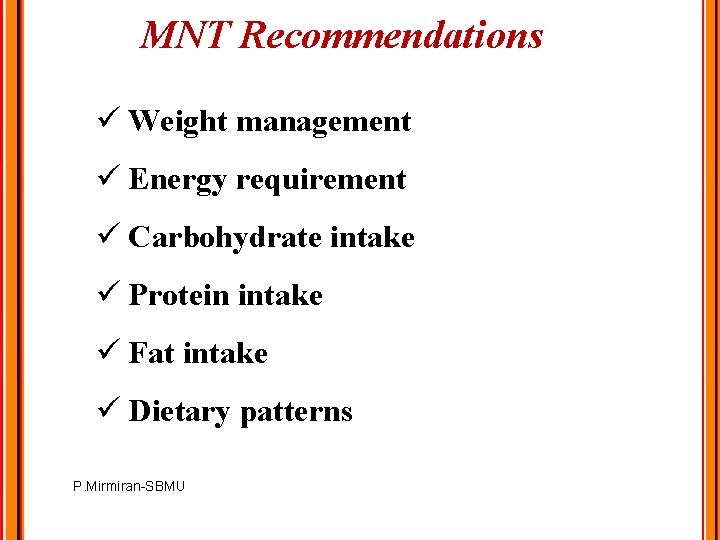
MNT Recommendations ü Weight management ü Energy requirement ü Carbohydrate intake ü Protein intake ü Fat intake ü Dietary patterns P. Mirmiran-SBMU
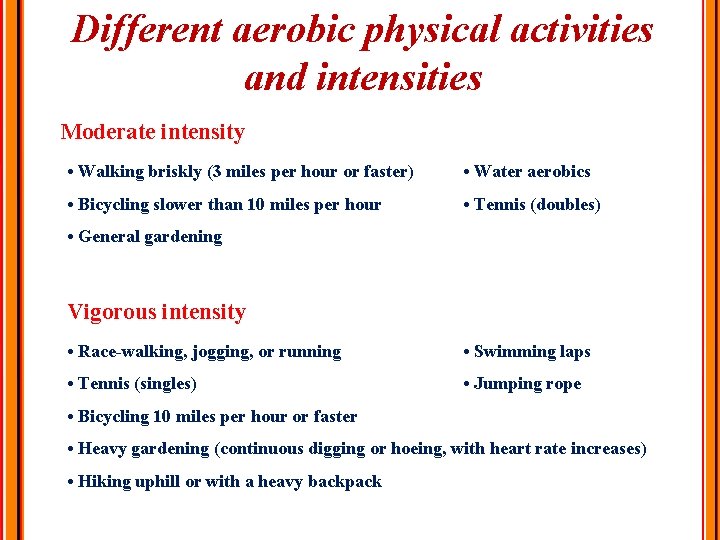
Different aerobic physical activities and intensities Moderate intensity • Walking briskly (3 miles per hour or faster) • Water aerobics • Bicycling slower than 10 miles per hour • Tennis (doubles) • General gardening Vigorous intensity • Race-walking, jogging, or running • Swimming laps • Tennis (singles) • Jumping rope • Bicycling 10 miles per hour or faster • Heavy gardening (continuous digging or hoeing, with heart rate increases) • Hiking uphill or with a heavy backpack
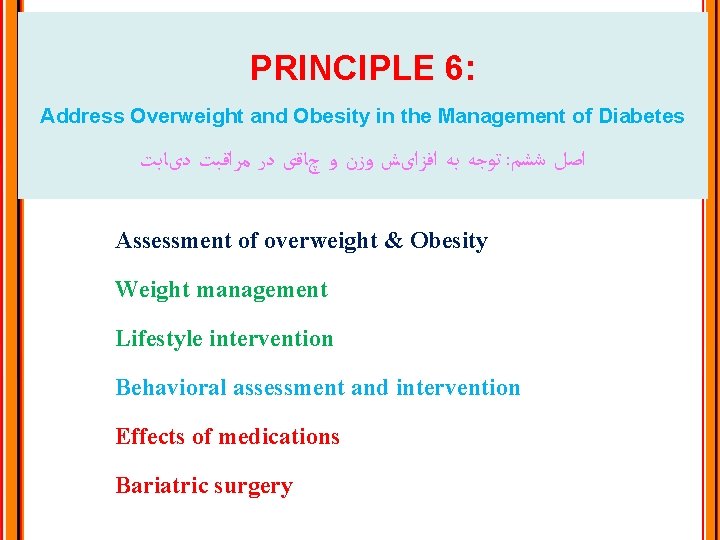
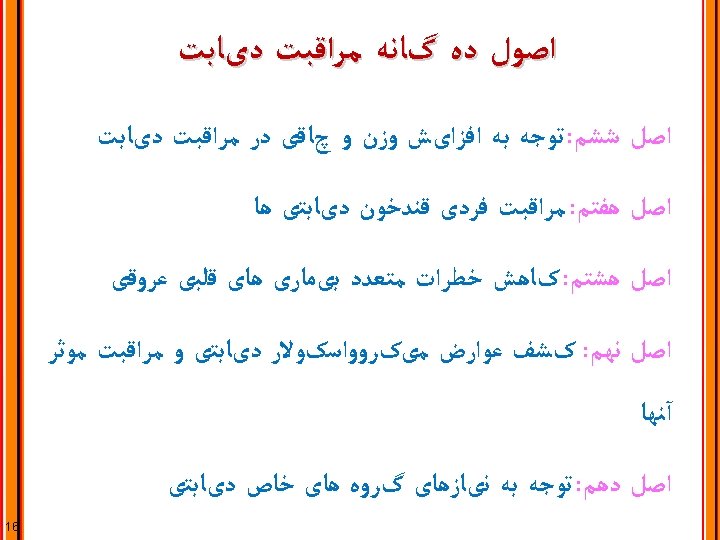
PRINCIPLE 6: Address Overweight and Obesity in the Management of Diabetes ﺗﻮﺟﻪ ﺑﻪ ﺍﻓﺰﺍیﺶ ﻭﺯﻥ ﻭ چﺎﻗی ﺩﺭ ﻣﺮﺍﻗﺒﺖ ﺩیﺎﺑﺖ : ﺍﺻﻞ ﺷﺸﻢ Assessment of overweight & Obesity Weight management Lifestyle intervention Behavioral assessment and intervention Effects of medications Bariatric surgery
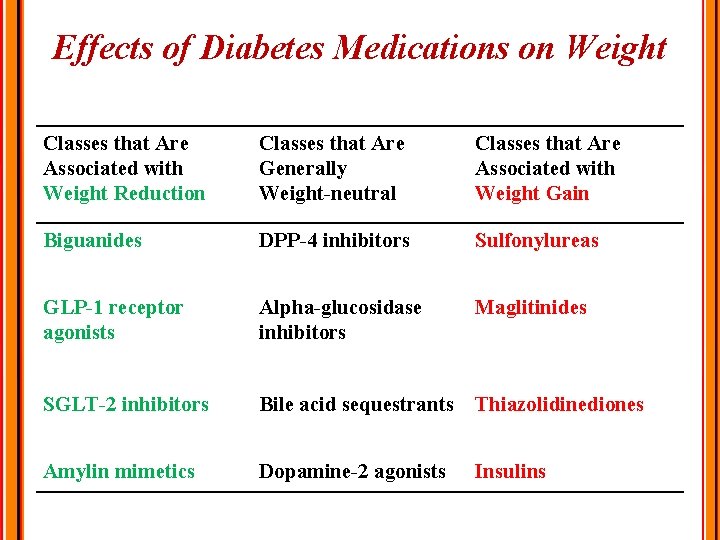
Effects of Diabetes Medications on Weight Classes that Are Associated with Weight Reduction Classes that Are Generally Weight-neutral Classes that Are Associated with Weight Gain Biguanides DPP-4 inhibitors Sulfonylureas GLP-1 receptor agonists Alpha-glucosidase inhibitors Maglitinides SGLT-2 inhibitors Bile acid sequestrants Thiazolidinediones Amylin mimetics Dopamine-2 agonists Insulins
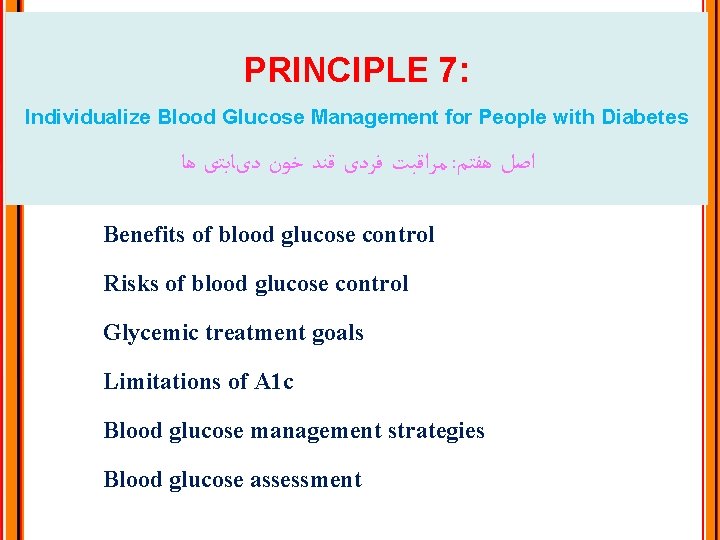
PRINCIPLE 7: Individualize Blood Glucose Management for People with Diabetes ﻣﺮﺍﻗﺒﺖ ﻓﺮﺩی ﻗﻨﺪ ﺧﻮﻥ ﺩیﺎﺑﺘی ﻫﺎ : ﺍﺻﻞ ﻫﻔﺘﻢ Benefits of blood glucose control Risks of blood glucose control Glycemic treatment goals Limitations of A 1 c Blood glucose management strategies Blood glucose assessment
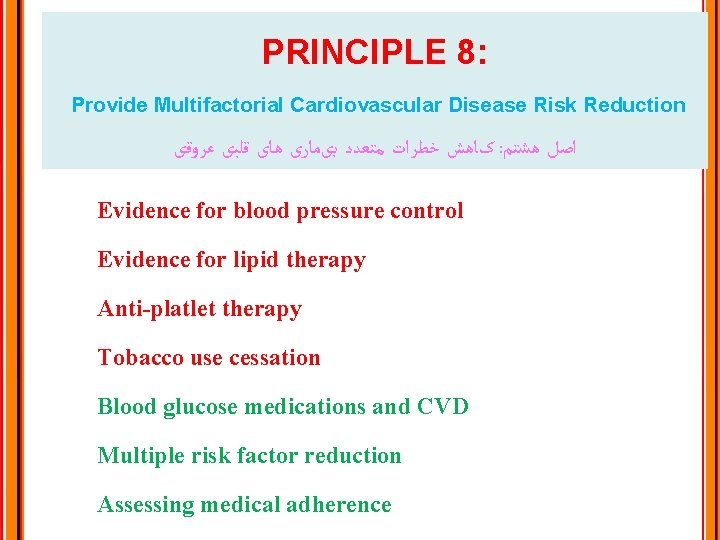
PRINCIPLE 8: Provide Multifactorial Cardiovascular Disease Risk Reduction کﺎﻫﺶ ﺧﻄﺮﺍﺕ ﻣﺘﻌﺪﺩ ﺑیﻤﺎﺭی ﻫﺎی ﻗﻠﺒی ﻋﺮﻭﻗی : ﺍﺻﻞ ﻫﺸﺘﻢ Evidence for blood pressure control Evidence for lipid therapy Anti-platlet therapy Tobacco use cessation Blood glucose medications and CVD Multiple risk factor reduction Assessing medical adherence
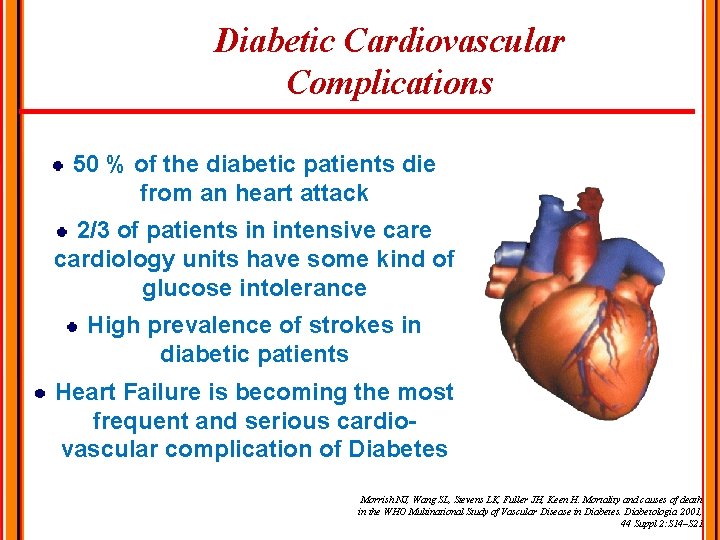
Diabetic Cardiovascular Complications 50 % of the diabetic patients die from an heart attack 2/3 of patients in intensive cardiology units have some kind of glucose intolerance High prevalence of strokes in diabetic patients Heart Failure is becoming the most frequent and serious cardiovascular complication of Diabetes Morrish NJ, Wang SL, Stevens LK, Fuller JH, Keen H. Mortality and causes of death in the WHO Multinational Study of Vascular Disease in Diabetes. Diabetologia 2001, 44 Suppl 2: S 14–S 21.
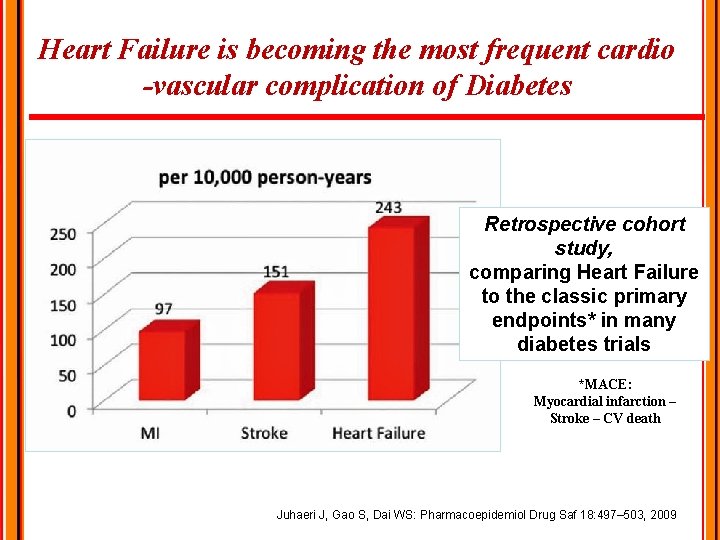
Heart Failure is becoming the most frequent cardio -vascular complication of Diabetes Retrospective cohort study, comparing Heart Failure to the classic primary endpoints* in many diabetes trials *MACE: Myocardial infarction – Stroke – CV death Juhaeri J, Gao S, Dai WS: Pharmacoepidemiol Drug Saf 18: 497– 503, 2009
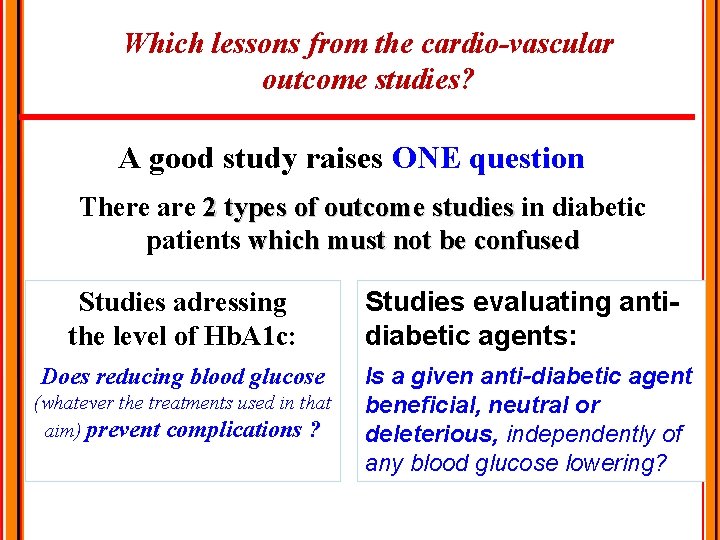
Which lessons from the cardio-vascular outcome studies? A good study raises ONE question There are 2 types of outcome studies in diabetic patients which must not be confused Studies adressing the level of Hb. A 1 c: Studies evaluating antidiabetic agents: Does reducing blood glucose Is a given anti-diabetic agent beneficial, neutral or deleterious, independently of any blood glucose lowering? (whatever the treatments used in that aim) prevent complications ?
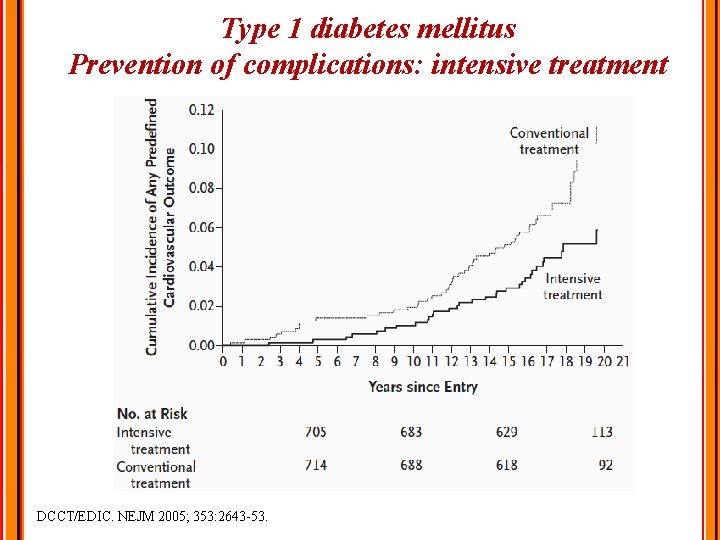
Type 1 diabetes mellitus Prevention of complications: intensive treatment DCCT/EDIC. NEJM 2005; 353: 2643 -53.
Control of diabetes mellitus Prevention of CVD and glycemic control: Reduction of non-fatal MI No clear effect on other vascular territories No effect on total or CV mortality Increased risk of severe hypoglycemia
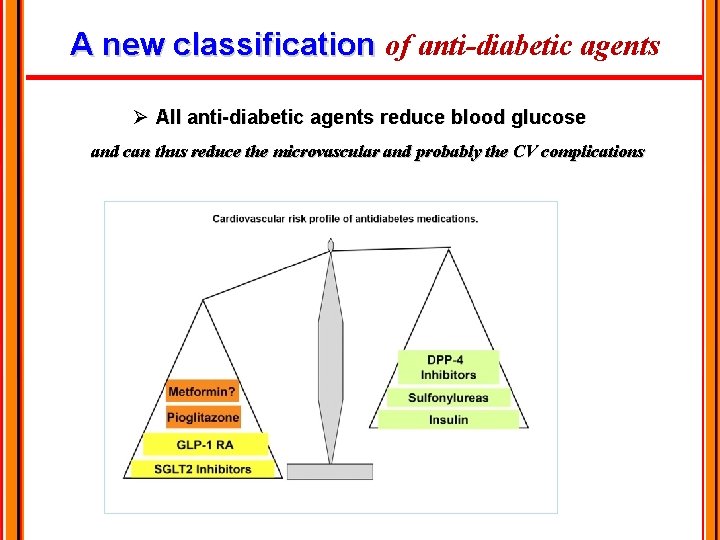
A new classification of anti-diabetic agents Ø All anti-diabetic agents reduce blood glucose and can thus reduce the microvascular and probably the CV complications
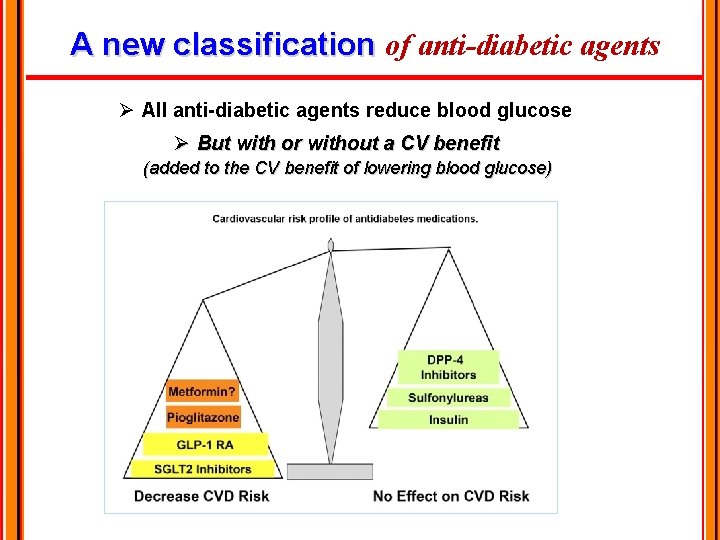
A new classification of anti-diabetic agents Ø All anti-diabetic agents reduce blood glucose Ø But with or without a CV benefit (added to the CV benefit of lowering blood glucose)
PRINCIPLE 9: Detect and Monitor Diabetes Microvascular Complications and Provide Treatment to Slow Their Progression کﺸﻒ ﻋﻮﺍﺭﺽ ﻣیکﺮﻭﻭﺍﺳکﻮﻻﺭ ﺩیﺎﺑﺘی ﻭ ﻣﺮﺍﻗﺒﺖ ﻣﻮﺛﺮ آﻨﻬﺎ : ﺍﺻﻞ ﻧﻬﻢ 54 Nephropathy Neuropathy Retinopathy Foot care
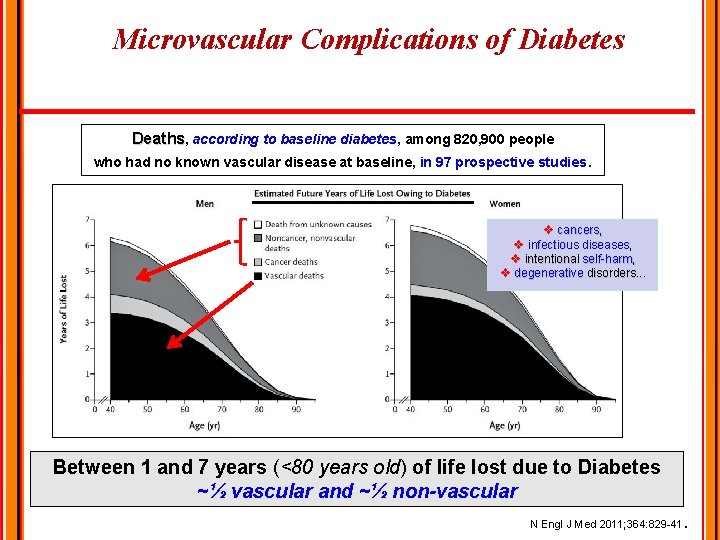
Microvascular Complications of Diabetes Deaths, according to baseline diabetes, among 820, 900 people who had no known vascular disease at baseline, in 97 prospective studies. v cancers, v infectious diseases, v intentional self-harm, v degenerative disorders. . . Between 1 and 7 years (<80 years old) of life lost due to Diabetes ~½ vascular and ~½ non-vascular. N Engl J Med 2011; 364: 829 -41
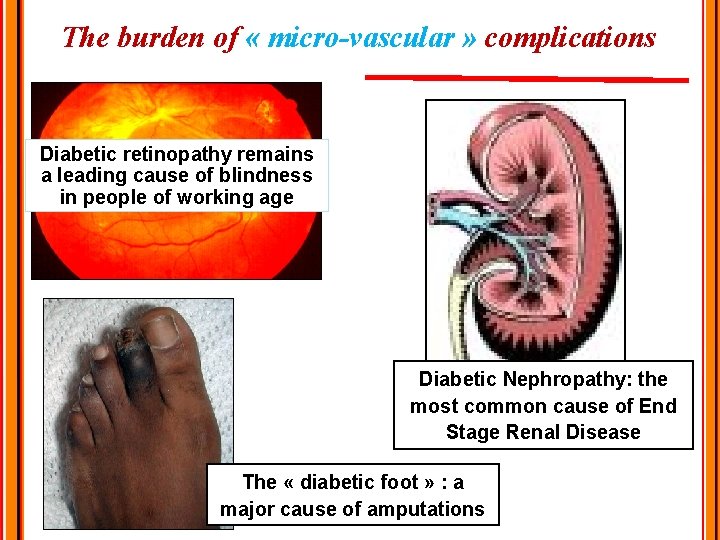
The burden of « micro-vascular » complications Diabetic retinopathy remains a leading cause of blindness in people of working age Diabetic Nephropathy: the most common cause of End Stage Renal Disease The « diabetic foot » : a major cause of amputations
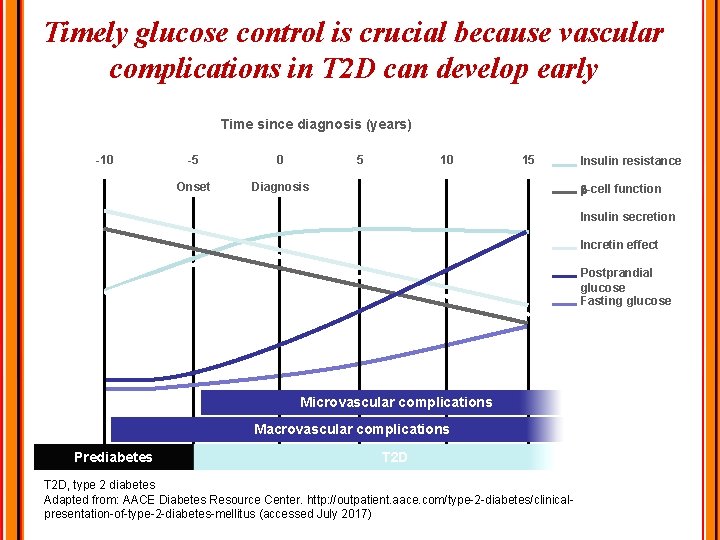
Timely glucose control is crucial because vascular complications in T 2 D can develop early Time since diagnosis (years) -10 -5 0 5 Onset Diagnosis 10 15 Insulin resistance -cell function Insulin secretion Incretin effect Postprandial glucose Fasting glucose Microvascular complications Macrovascular complications Prediabetes T 2 D, type 2 diabetes Adapted from: AACE Diabetes Resource Center. http: //outpatient. aace. com/type-2 -diabetes/clinicalpresentation-of-type-2 -diabetes-mellitus (accessed July 2017)
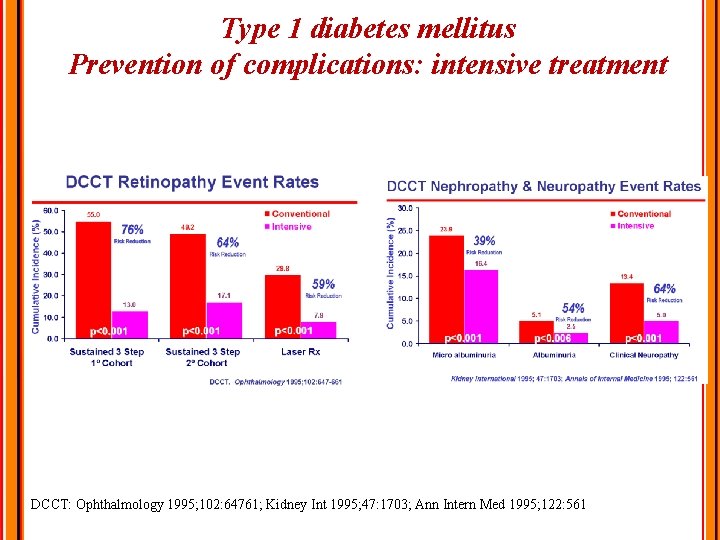
Type 1 diabetes mellitus Prevention of complications: intensive treatment DCCT: Ophthalmology 1995; 102: 64761; Kidney Int 1995; 47: 1703; Ann Intern Med 1995; 122: 561
PRINCIPLE 10: Consider the Needs of Special Populations with Diabetes ﺗﻮﺟﻪ ﺑﻪ ﻧیﺎﺯﻫﺎی گﺮﻭﻩ ﻫﺎی ﺧﺎﺹ ﺩیﺎﺑﺘی : ﺍﺻﻞ ﺩﻫﻢ Children and adolescents Women of childbearing age High risk racial & ethnic groups
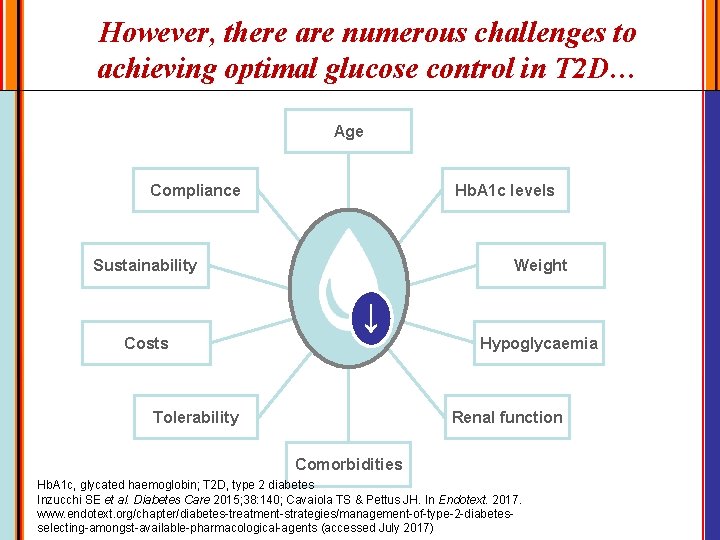
However, there are numerous challenges to achieving optimal glucose control in T 2 D… Age Compliance Hb. A 1 c levels Sustainability Weight ↓ Costs Hypoglycaemia Tolerability Renal function Comorbidities Hb. A 1 c, glycated haemoglobin; T 2 D, type 2 diabetes Inzucchi SE et al. Diabetes Care 2015; 38: 140; Cavaiola TS & Pettus JH. In Endotext. 2017. www. endotext. org/chapter/diabetes-treatment-strategies/management-of-type-2 -diabetesselecting-amongst-available-pharmacological-agents (accessed July 2017)
DIABETES MANAGEMENT: OBSTACLES THE PATIENT Ø Therapeutic interventions are complex Ø Real-life treatment adherence is really lower than expected Ø Treatment adherence • Self-awareness of the disease state • Knowledge of potential disease complications • Beliefs on treatment benefits • Beliefs on the impact of the disease in own’s daily life Ø Individual circumstances: multiple factors
DIABETES MANAGEMENT: OBSTACLES HEALTH CARE PROFESSIONALS Professional education, especially among physicians, centered mainly on biomedical aspects of the disease The patient is not a passive player Lack of training on patient education, communication and psychological skills and The model of acute versus chronic disease Low tolerance to frustration The need to work on a team basis: multiple types of expertise are necessary for proper treatment
Difficulties in Achieving Target A 1 c values Challenges - Late diagnosis and initiation of therapy - Therapeutic inertia - Lack of effective lifestyle intervention - Secondary failure - Role of posparandial glucose in failure - Adverse events of antihyperglycemic therapies - Complexity of care
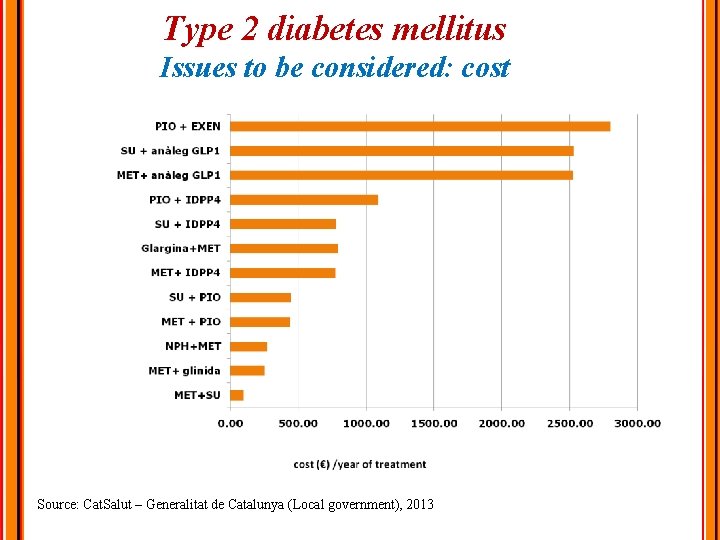
Type 2 diabetes mellitus Issues to be considered: cost Source: Cat. Salut – Generalitat de Catalunya (Local government), 2013
WHO Guidelines on Diabetes Management in Low-Resource Settings • Prescribe sulfonylurea agents to patients with type 2 diabetes who do not achieve glycemic control with metformin alone. • Prescribe regular human insulin to patients with type 2 diabetes who do not achieve glycemic control with metformin plus a sulfonylurea. • Prescribe a dipeptidyl peptidase-4 (DPP-4) inhibitor, a sodium-glucose cotransporter-2 (SGLT-2) inhibitor, or a thiazolidinedione (TZD) if insulin is unsuitable (e. g. , if a patient or surrogate is unable to administer insulin at home). • Prescribe regular human insulin, neutral protamine Hagedorn (NPH) insulin, or both to achieve glycemic control in patients with type 1 diabetes and in adults with type 2 diabetes for whom insulin is indicated. • Prescribe long-acting insulin analogues (e. g. , glargine, detemir) when patients with type 1 or type 2 diabetes experience frequent, severe hypoglycemia with regular or NPH insulin alone. Ann Intern Med 2018 Sep 4; 169: 394. (https: //doi. org/10. 7326/M 18 -1149)
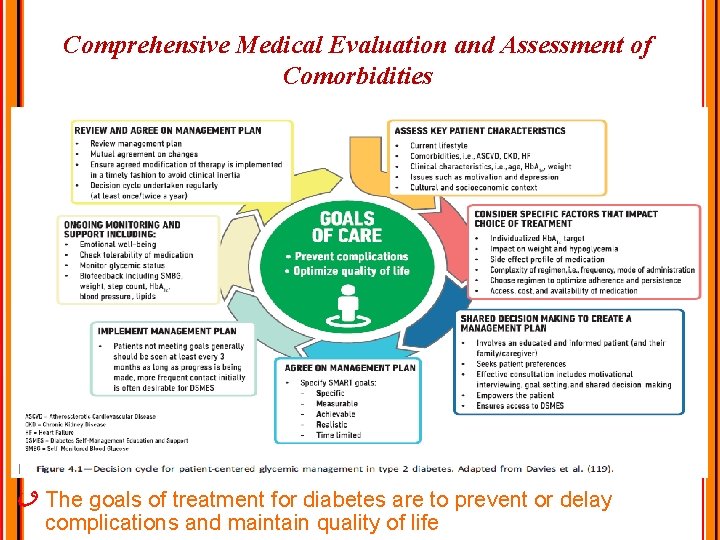
Comprehensive Medical Evaluation and Assessment of Comorbidities The goals of treatment for diabetes are to prevent or delay complications and maintain quality of life
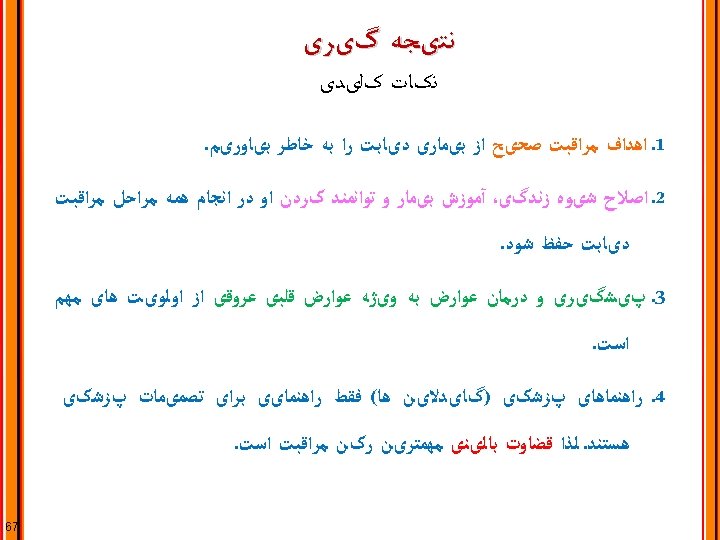

69
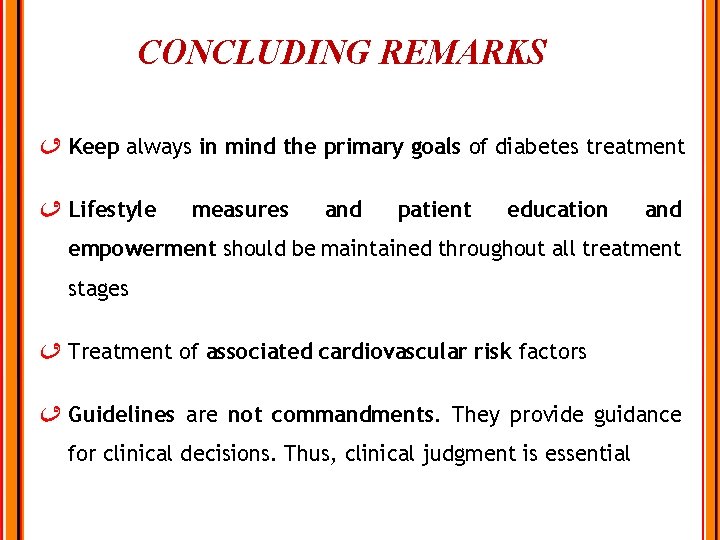
CONCLUDING REMARKS Keep always in mind the primary goals of diabetes treatment Lifestyle measures and patient education and empowerment should be maintained throughout all treatment stages Treatment of associated cardiovascular risk factors Guidelines are not commandments. They provide guidance for clinical decisions. Thus, clinical judgment is essential
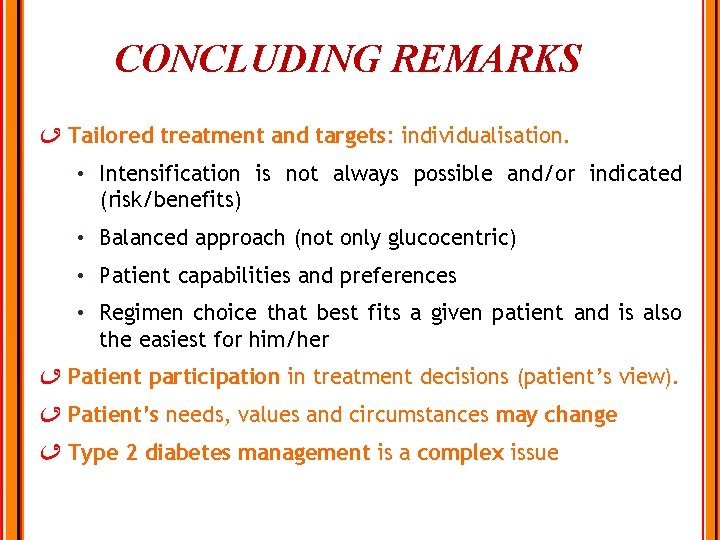
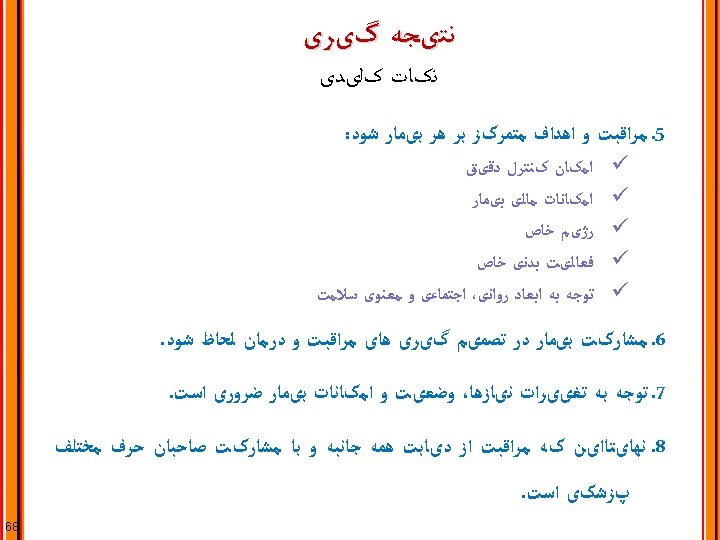
CONCLUDING REMARKS Tailored treatment and targets: individualisation. • Intensification is not always possible and/or indicated (risk/benefits) • Balanced approach (not only glucocentric) • Patient capabilities and preferences • Regimen choice that best fits a given patient and is also the easiest for him/her Patient participation in treatment decisions (patient’s view). Patient’s needs, values and circumstances may change Type 2 diabetes management is a complex issue
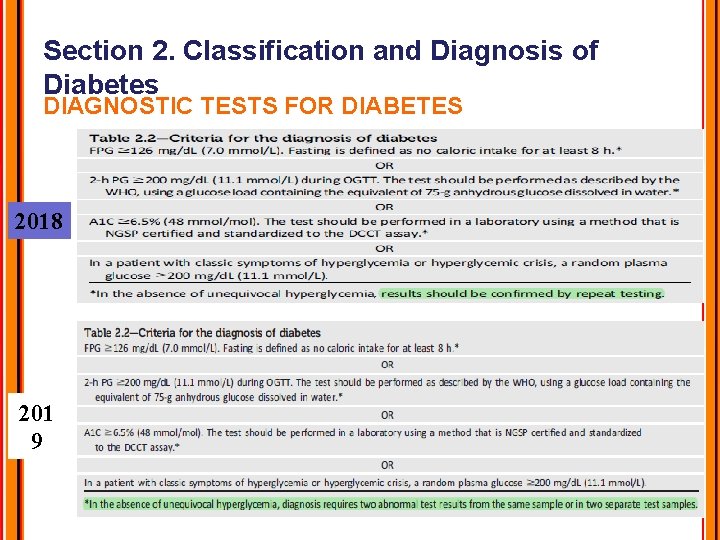
Section 2. Classification and Diagnosis of Diabetes DIAGNOSTIC TESTS FOR DIABETES 2018 201 9
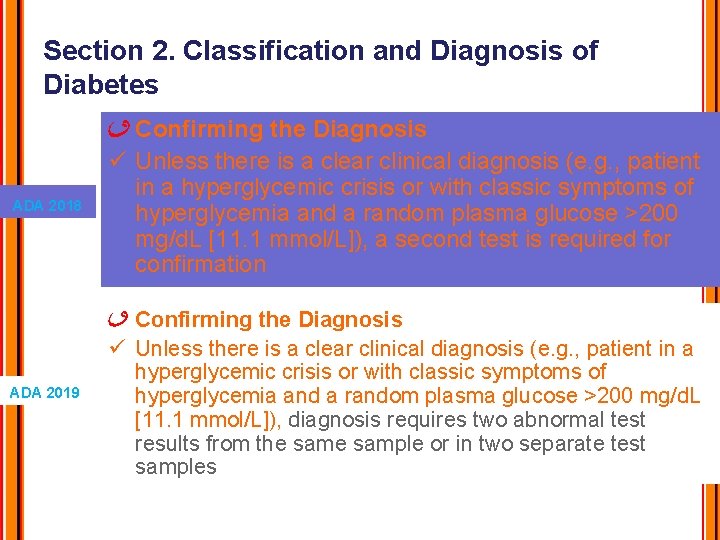
Section 2. Classification and Diagnosis of Diabetes ADA 2018 ADA 2019 Confirming the Diagnosis ü Unless there is a clear clinical diagnosis (e. g. , patient in a hyperglycemic crisis or with classic symptoms of hyperglycemia and a random plasma glucose >200 mg/d. L [11. 1 mmol/L]), a second test is required for confirmation Confirming the Diagnosis ü Unless there is a clear clinical diagnosis (e. g. , patient in a hyperglycemic crisis or with classic symptoms of hyperglycemia and a random plasma glucose >200 mg/d. L [11. 1 mmol/L]), diagnosis requires two abnormal test results from the sample or in two separate test samples
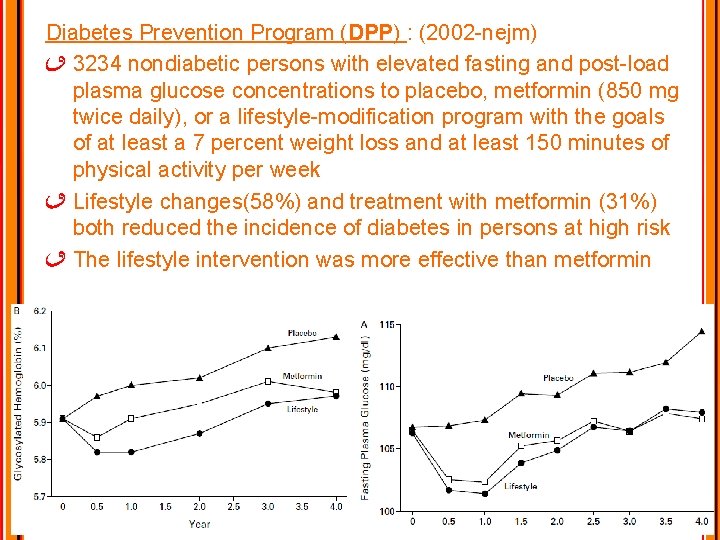
Diabetes Prevention Program (DPP) : (2002 -nejm) 3234 nondiabetic persons with elevated fasting and post-load plasma glucose concentrations to placebo, metformin (850 mg twice daily), or a lifestyle-modification program with the goals of at least a 7 percent weight loss and at least 150 minutes of physical activity per week Lifestyle changes(58%) and treatment with metformin (31%) both reduced the incidence of diabetes in persons at high risk The lifestyle intervention was more effective than metformin

in the period 2004– 2014 for guidelines, meta-analyses, and randomized trials assessing the outcomes Hb. A 1 c, BMI, weight, LDL cholesterol, quality of life (Qo. L), and attrition 1376 participants in total [comparing carbohydrate restriction (below 45%) to diet of 45– 60% carbohydrate] Low to moderate carbohydrate diets have greater effect on glycemic control in type 2 diabetes compared with highcarbohydrate diets in the first year of intervention The greater the carbohydrate restriction, the greater glucose lowering Apart from improvements in Hb. A 1 c over the short term, there is no superiority of low-carbohydrate diets in terms of glycemic control, weight, or LDL cholesterol
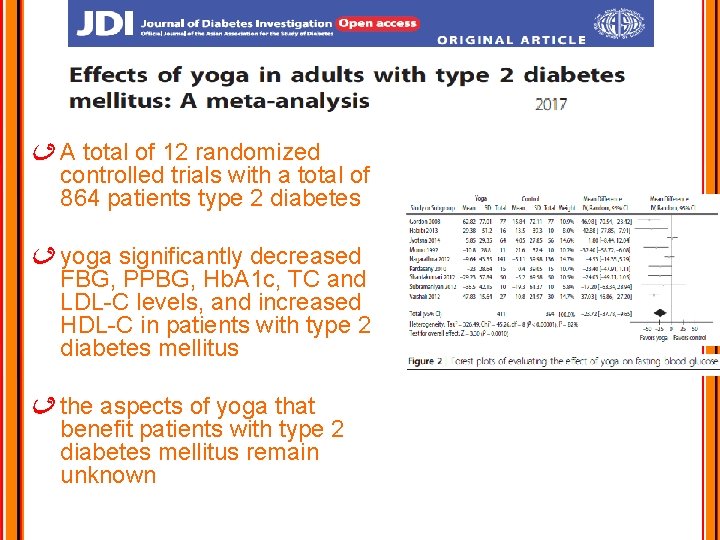
A total of 12 randomized controlled trials with a total of 864 patients type 2 diabetes yoga significantly decreased FBG, PPBG, Hb. A 1 c, TC and LDL-C levels, and increased HDL-C in patients with type 2 diabetes mellitus the aspects of yoga that benefit patients with type 2 diabetes mellitus remain unknown
Section 5. Lifestyle Management SMOKING CESSATION: TOBACCO AND ECIGARETTES ü Recent data show tobacco use is higher among adults with chronic conditions as well as in adolescents and young adults with diabetes ü Smokers with diabetes (and people with diabetes exposed to second-hand smoke) have a heightened risk of CVD, premature death, microvascular complications, and worse glycemic control when compared with nonsmokers
- Slides: 77