1 BLOOD EXAMINATION 2 CHEST X RAY 3
1. BLOOD EXAMINATION 2. CHEST X- RAY 3. LIVER FUNCTION TESTS 4. IMAGING STUDIES q Non invasive q Invasive 5. LIVER BIOPSY
Blood Examination Routine examinations Infections C/c liver disease l Tumor markers l
Viral hepatitis Hepatitis A - Ig. M Anti. HAV antibodies Hepatitis B – HBs Ag – ‘Australia antigen’ HBe Ag – for replication &infectivity Anti HBS – immunity to HBV Hepatitis C – Anti. HCV antibody Hepatitis D – PCR HDV – RNA Hepatitis E – Anti HEV anti bodies
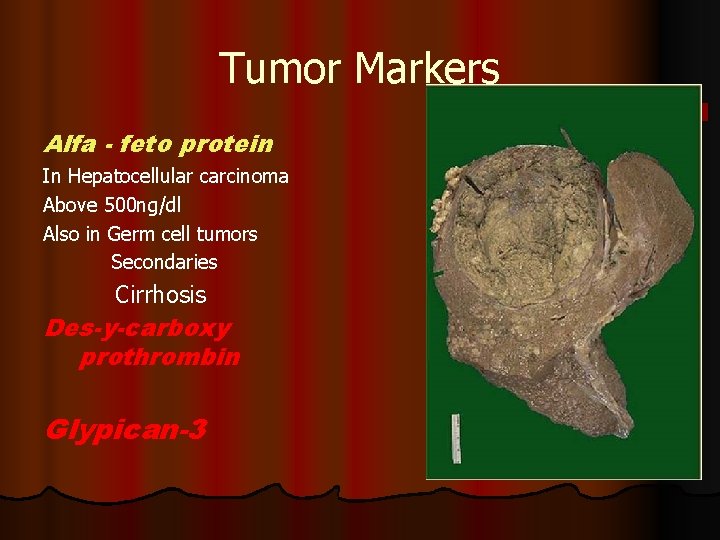
Tumor Markers Alfa - feto protein In Hepatocellular carcinoma Above 500 ng/dl Also in Germ cell tumors Secondaries Cirrhosis Des-y-carboxy prothrombin Glypican-3
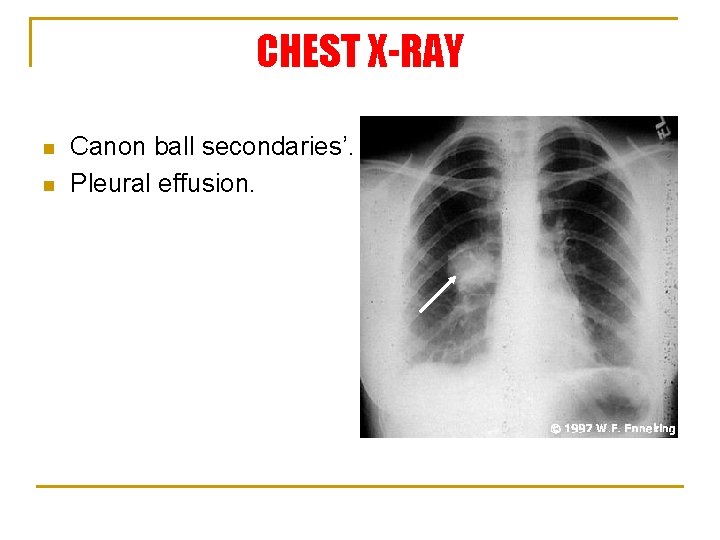
CHEST X-RAY n n Canon ball secondaries’. Pleural effusion.

Liver Function Tests based on the excretory function n Tests based on the metabolic capacity of the liver n Tests based on synthetic function of liver n Tests based on serum enzymes n
TESTS BASED ON EXCRETORY FUNCTIONS
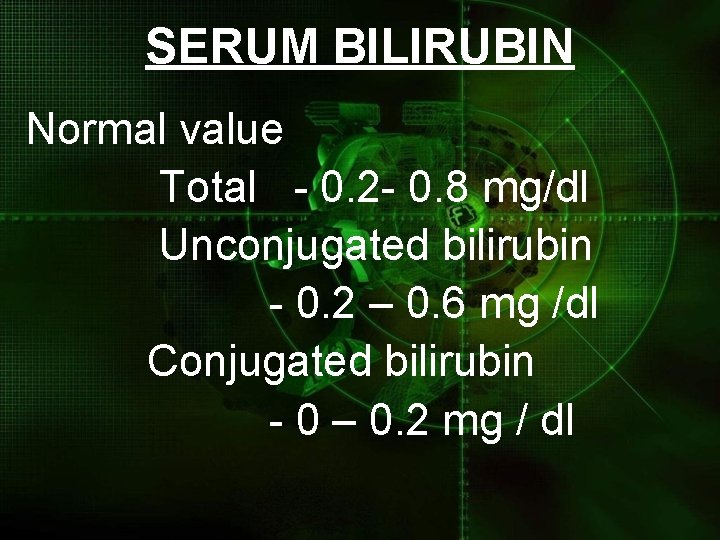
SERUM BILIRUBIN Normal value Total - 0. 2 - 0. 8 mg/dl Unconjugated bilirubin - 0. 2 – 0. 6 mg /dl Conjugated bilirubin - 0 – 0. 2 mg / dl
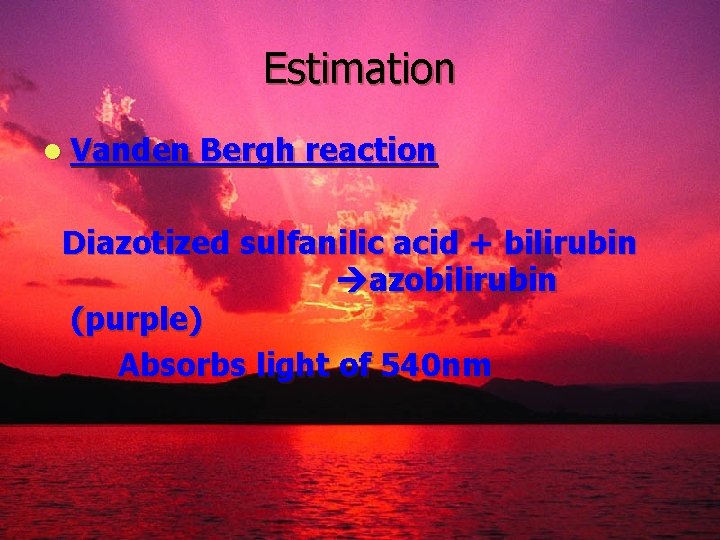
Estimation l Vanden Bergh reaction Diazotized sulfanilic acid + bilirubin azobilirubin (purple) Absorbs light of 540 nm
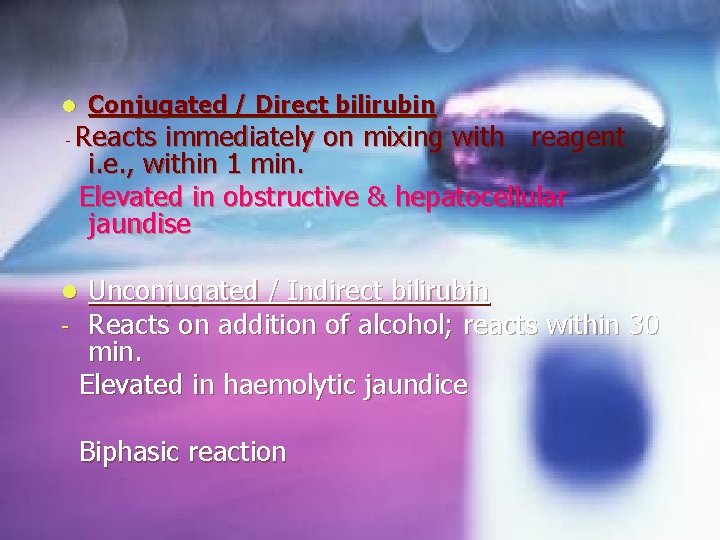
Conjugated / Direct bilirubin l - Reacts immediately on mixing with reagent i. e. , within 1 min. Elevated in obstructive & hepatocellular jaundise Unconjugated / Indirect bilirubin Reacts on addition of alcohol; reacts within 30 min. Elevated in haemolytic jaundice l - Biphasic reaction
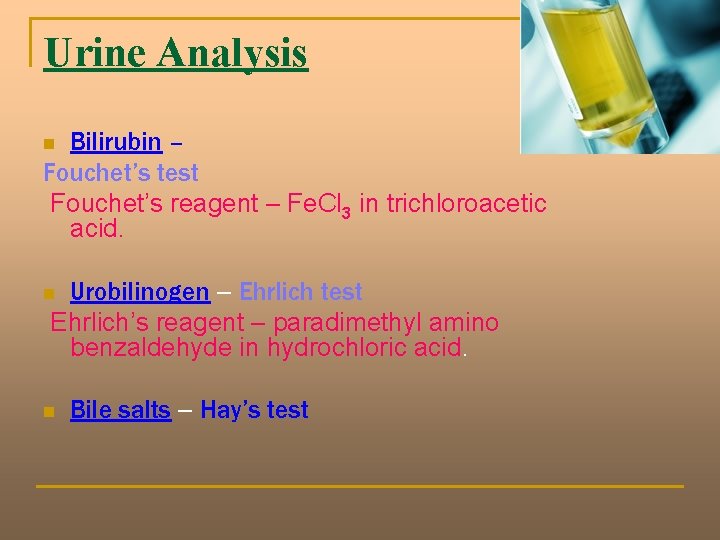
Urine Analysis Bilirubin – Fouchet’s test Fouchet’s reagent – Fe. Cl 3 in trichloroacetic acid. n Urobilinogen – Ehrlich test Ehrlich’s reagent – paradimethyl amino benzaldehyde in hydrochloric acid. n n Bile salts – Hay’s test
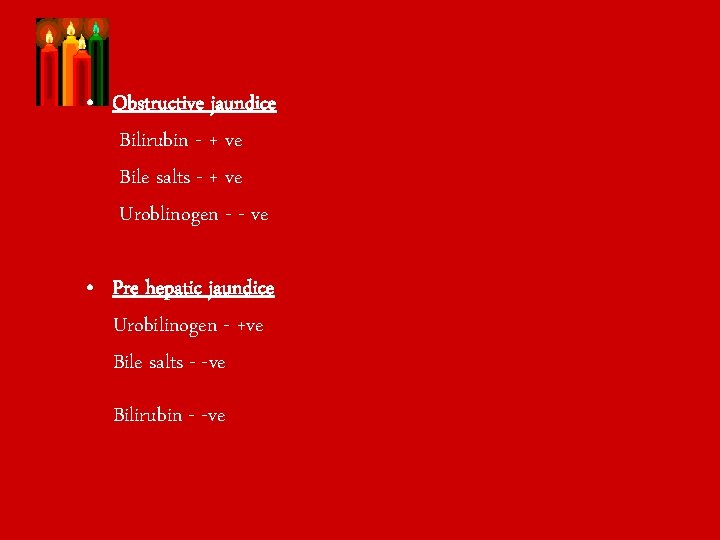
• Obstructive jaundice Bilirubin - + ve Bile salts - + ve Uroblinogen - - ve • Pre hepatic jaundice Urobilinogen - +ve Bile salts - -ve Bilirubin - -ve
o o o Dye excretion Dyes used - Indocyanin green - Sulfobromophthlein Done for - hepatic blood flow - portal blood flow - Porto systemic shunt - surgical shunt evaluation
Tests for metabolic capacity n Amino pyrine breath test – using C 14 labeled aminopyrine. De methylation Aminopyrine 14 CO liver • Normal 2 people expires – 6. 6 % +/- 1. 3 % Uses - assess residual functional liver cells. - prognosis of a disease. in 2 hrs.
Galactose tolerance test Plasma Amino Acids Lidocain clearance test Metabolite tested is Monoethylglycinexlide
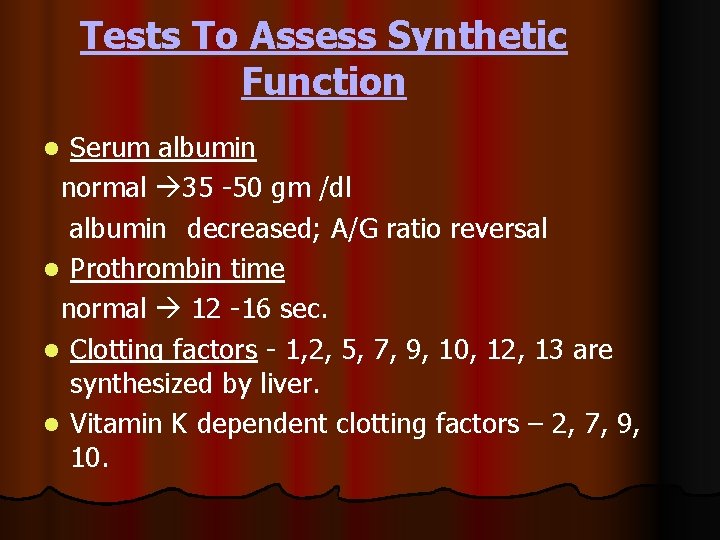
Tests To Assess Synthetic Function Serum albumin normal 35 -50 gm /dl albumin decreased; A/G ratio reversal l Prothrombin time normal 12 -16 sec. l Clotting factors - 1, 2, 5, 7, 9, 10, 12, 13 are synthesized by liver. l Vitamin K dependent clotting factors – 2, 7, 9, 10. l
Tests based on serum enzymes
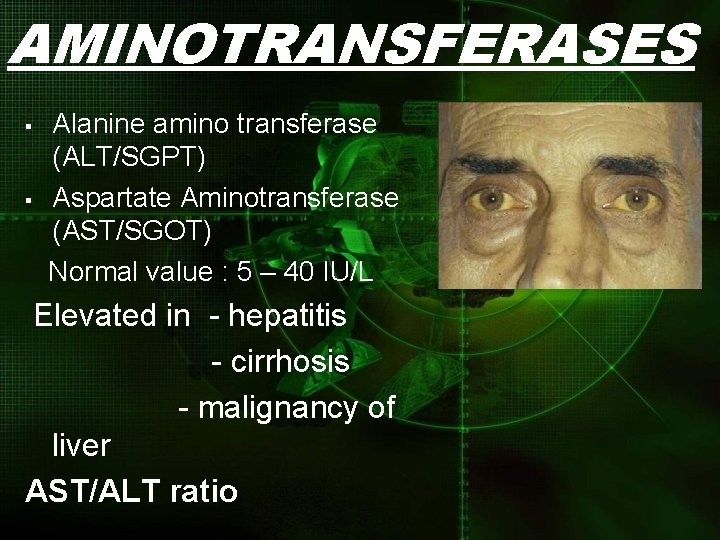
AMINOTRANSFERASES § § Alanine amino transferase (ALT/SGPT) Aspartate Aminotransferase (AST/SGOT) Normal value : 5 – 40 IU/L Elevated in - hepatitis - cirrhosis - malignancy of liver AST/ALT ratio
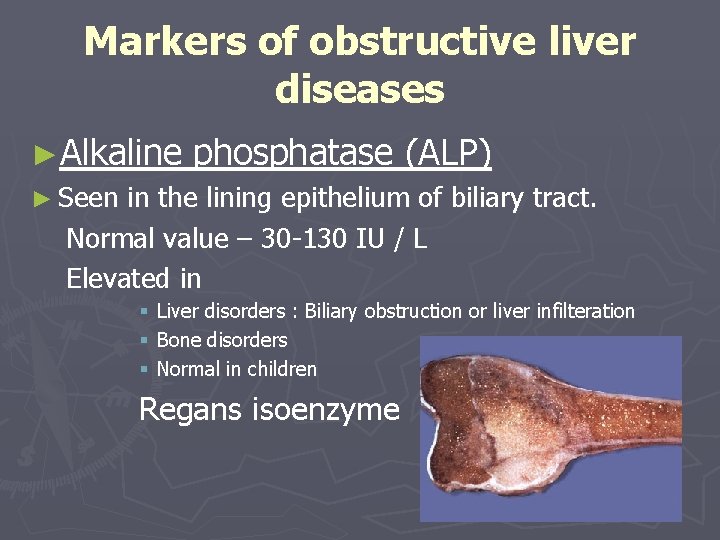
Markers of obstructive liver diseases ►Alkaline phosphatase (ALP) ► Seen in the lining epithelium of biliary tract. Normal value – 30 -130 IU / L Elevated in § § § Liver disorders : Biliary obstruction or liver infilteration Bone disorders Normal in children Regans isoenzyme
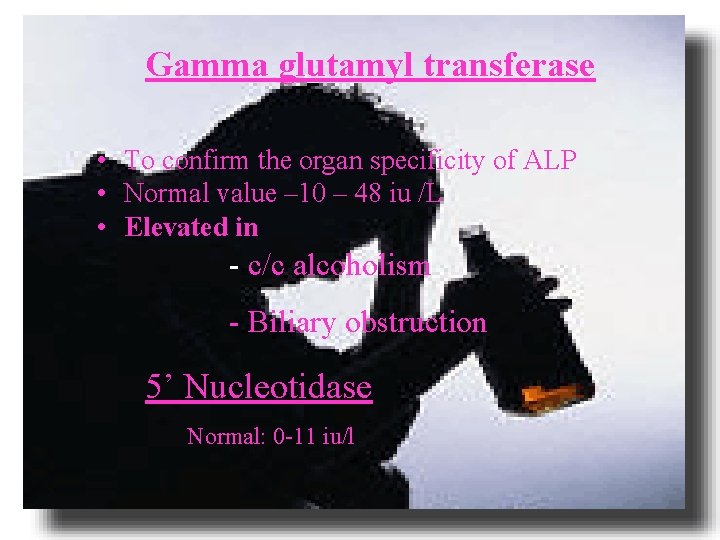
Gamma glutamyl transferase • To confirm the organ specificity of ALP • Normal value – 10 – 48 iu /L • Elevated in - c/c alcoholism - Biliary obstruction 5’ Nucleotidase Normal: 0 -11 iu/l
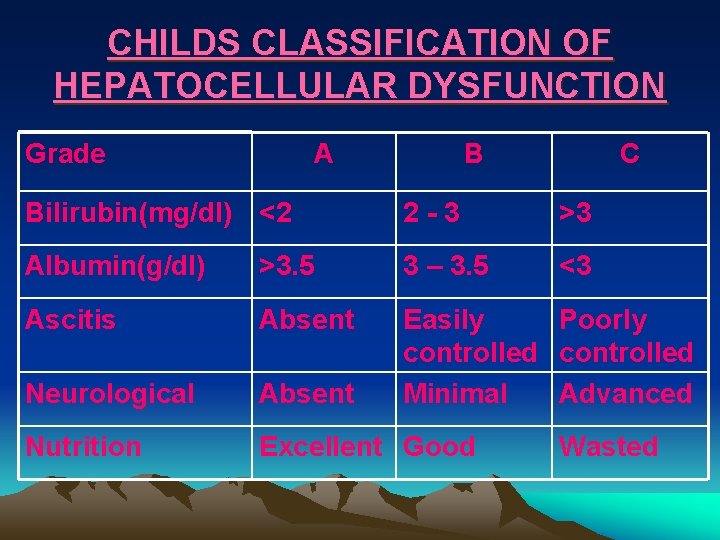
CHILDS CLASSIFICATION OF HEPATOCELLULAR DYSFUNCTION Grade A B C Bilirubin(mg/dl) <2 2 -3 >3 Albumin(g/dl) >3. 5 3 – 3. 5 <3 Ascitis Absent Neurological Absent Easily Poorly controlled Minimal Advanced Nutrition Excellent Good Wasted
Immunological markers • • Antinuclear antibodies Antimitochondrial antibodies LKM antibodies Liver membrane antibodies
LIVER BIOPSY
INDICATIONS FOR LIVER BIOPSY 1. Determine the cause of abnormal hepatic biochemical tests. 2. Diagnosis of multi system infiltrative, inflammatory or granulomatous diseases. 3. Diagnosis of neoplasms. 4. Grading and staging of c/c hepatitis. 5. Evaluation of cholestatic & alcoholic liver disease. 6. Evaluate the status of liver following transplantation; evaluate donor liver prior to harvesting.
TYPES Ø Trans cutaneous Ø Ultra sound or CT guided Ø Laparoscopic Ø Trans jugular approach
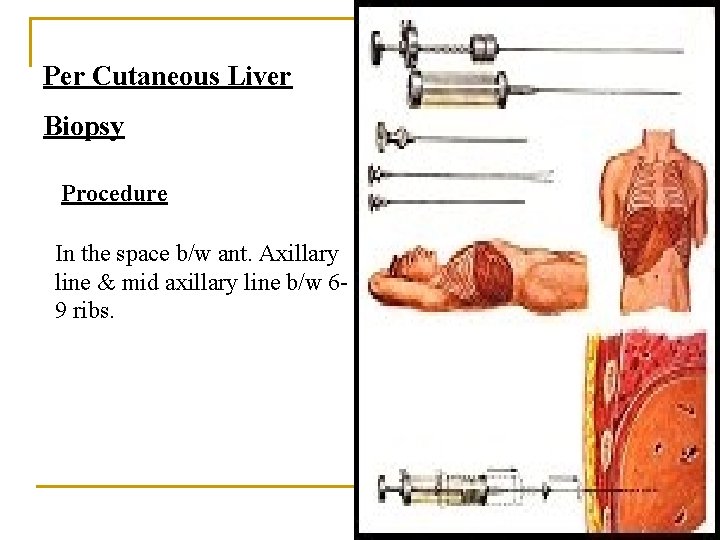
Per Cutaneous Liver Biopsy Procedure In the space b/w ant. Axillary line & mid axillary line b/w 69 ribs.
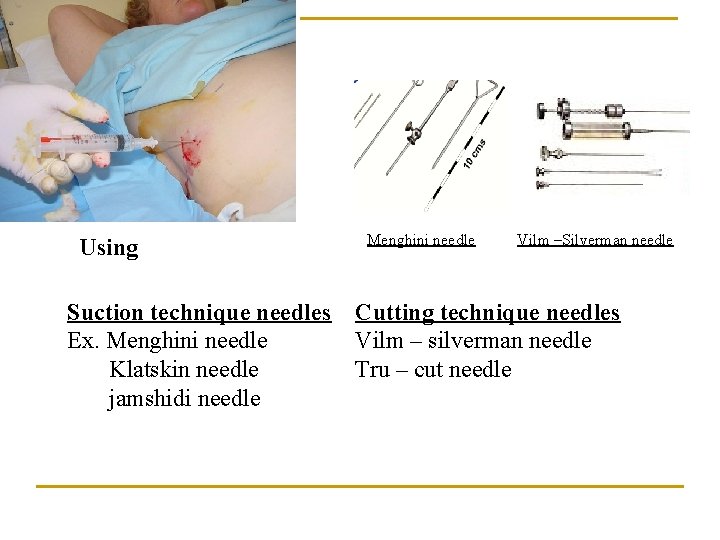
Using Suction technique needles Ex. Menghini needle Klatskin needle jamshidi needle Menghini needle Vilm –Silverman needle Cutting technique needles Vilm – silverman needle Tru – cut needle
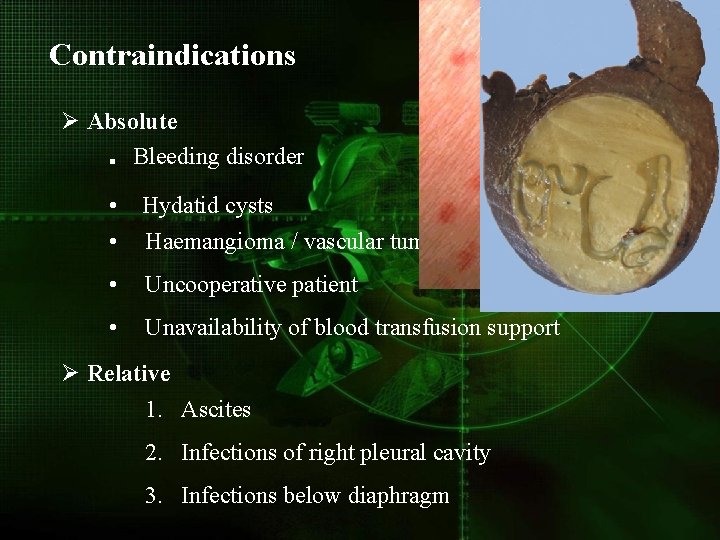
Contraindications Ø Absolute. Bleeding disorder • Hydatid cysts • Haemangioma / vascular tumors • Uncooperative patient • Unavailability of blood transfusion support Ø Relative 1. Ascites 2. Infections of right pleural cavity 3. Infections below diaphragm
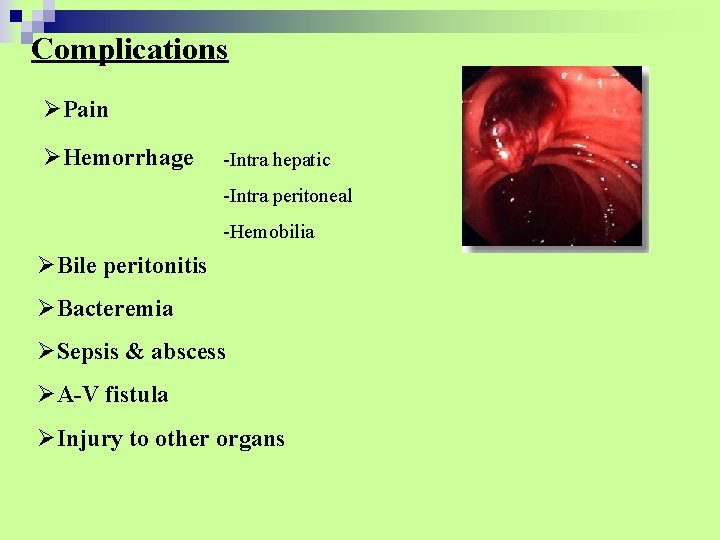
Complications ØPain ØHemorrhage -Intra hepatic -Intra peritoneal -Hemobilia ØBile peritonitis ØBacteremia ØSepsis & abscess ØA-V fistula ØInjury to other organs
Trans Jugular Liver Biopsy Indications 1. Significant coagulopathy 2. Moderate to severe ascites 3. Fulminant hepatic failure 4. Failed per cutaneous attempt
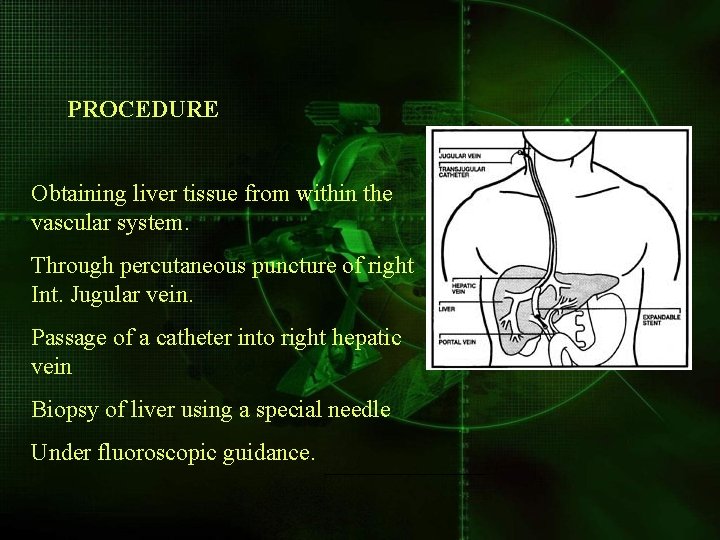
PROCEDURE Obtaining liver tissue from within the vascular system. Through percutaneous puncture of right Int. Jugular vein. Passage of a catheter into right hepatic vein Biopsy of liver using a special needle Under fluoroscopic guidance.
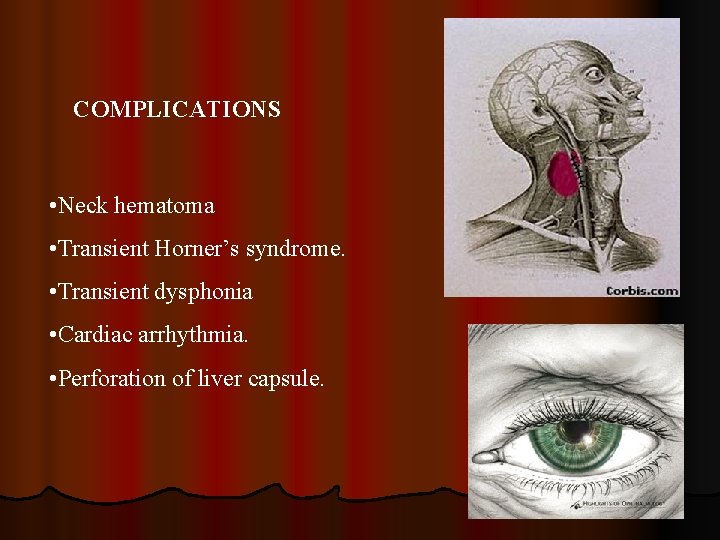
COMPLICATIONS • Neck hematoma • Transient Horner’s syndrome. • Transient dysphonia • Cardiac arrhythmia. • Perforation of liver capsule.
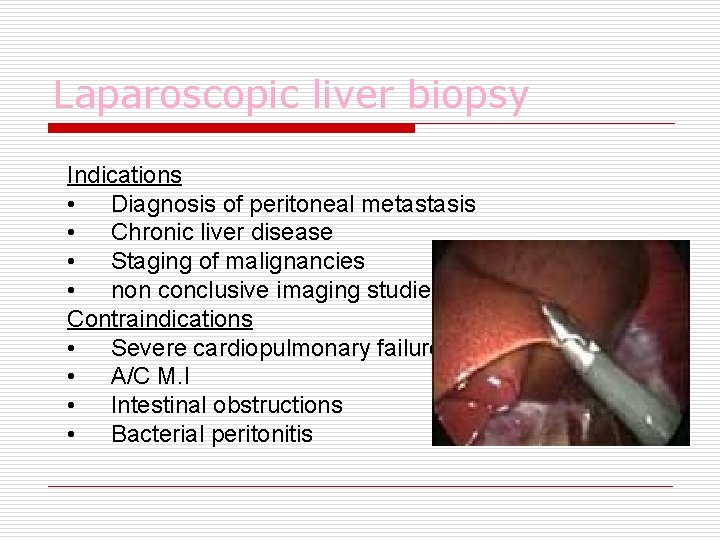
Laparoscopic liver biopsy Indications • Diagnosis of peritoneal metastasis • Chronic liver disease • Staging of malignancies • non conclusive imaging studies Contraindications • Severe cardiopulmonary failure • A/C M. I • Intestinal obstructions • Bacterial peritonitis
COMPLICATIONS ØMAJOR -Abdominal viscus perforation - Bleeding from liver biopsy site - Hemobilia - Spleen lacerations ØMINOR -Ascitic fluid leakage - Abdominal wall hematoma - Post laparoscopic fever
NON INVASIVE IMAGING OF LIVER v. X ray v. Ultrasonography v. Hepatic Doppler sonography v. CT /MRI v. MRCP
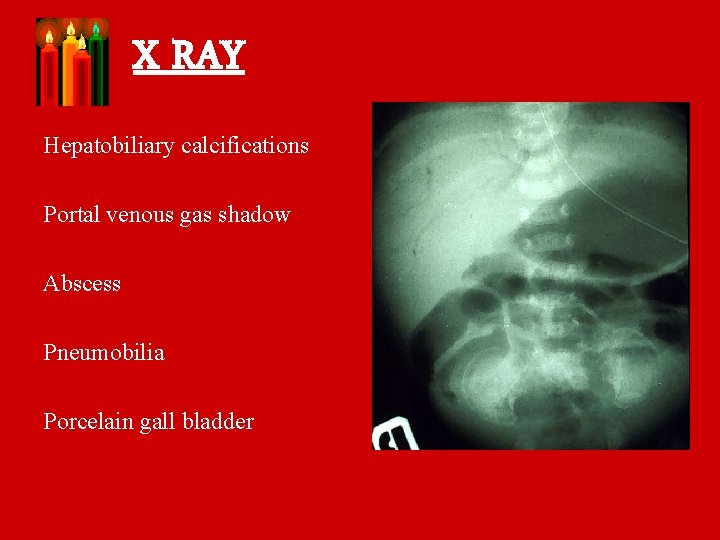
X RAY Hepatobiliary calcifications Portal venous gas shadow Abscess Pneumobilia Porcelain gall bladder

Porcelian gallbladder pneumobilia
Ultrasonography ► Most commonly used imaging modality for liver pathologies. ► Best evaluated with a 3 – 5 MHz transducer.

Normal liver
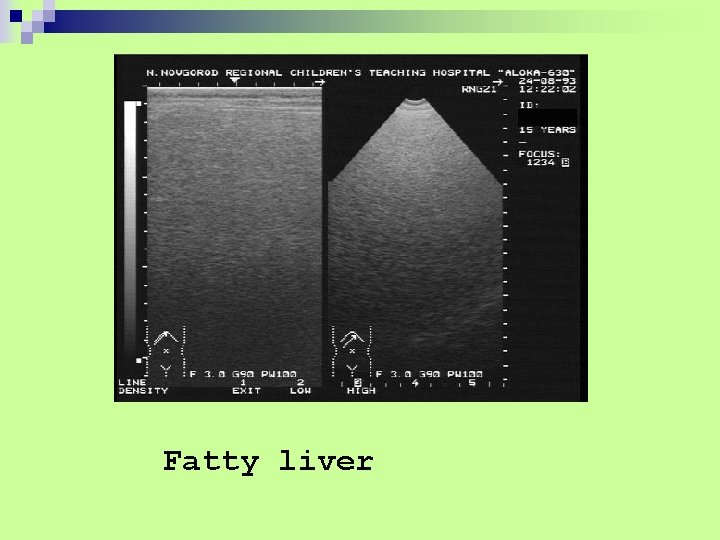
Fatty liver
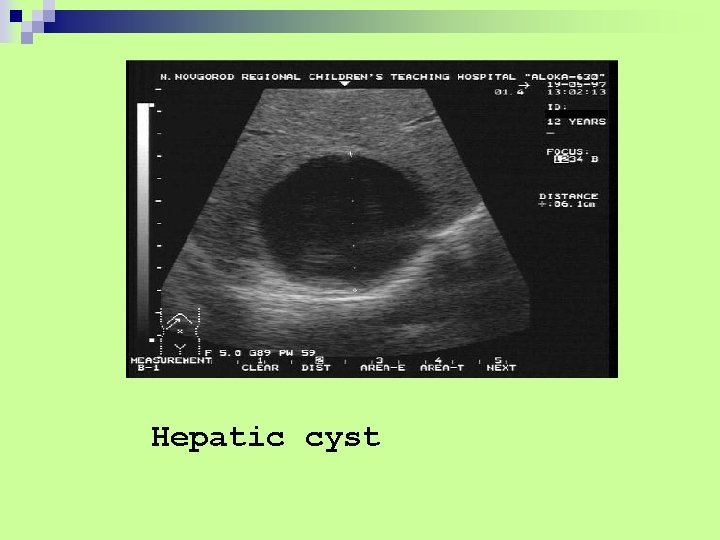
Hepatic cyst
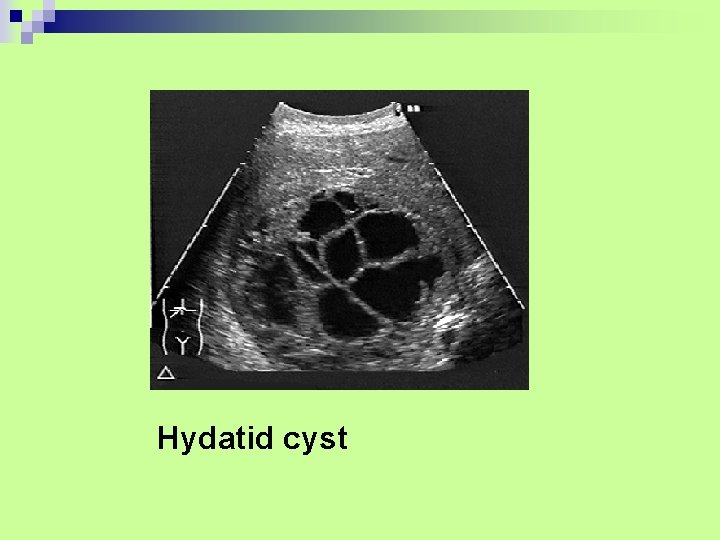
Hydatid cyst
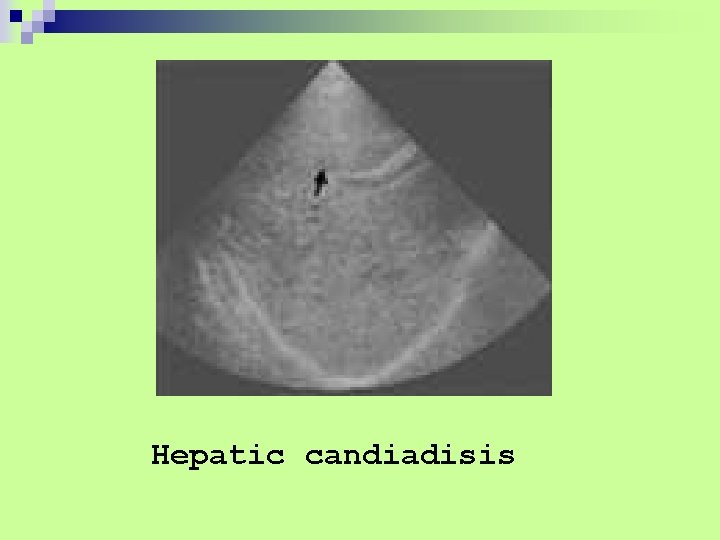
Hepatic candiadisis
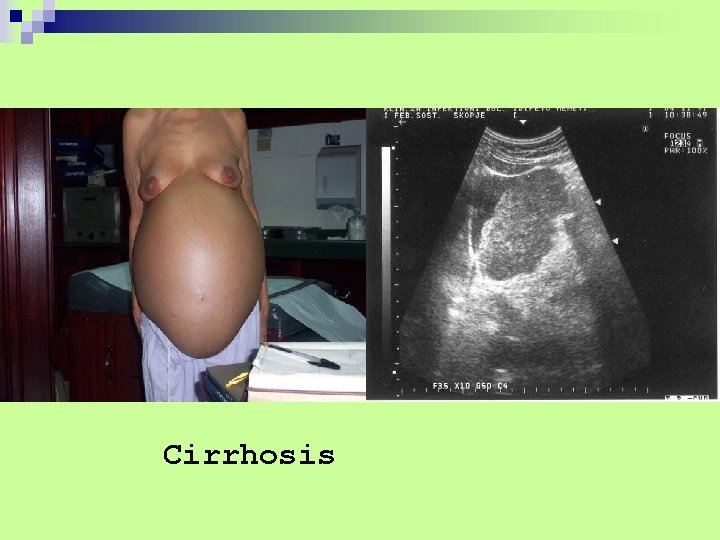
Cirrhosis
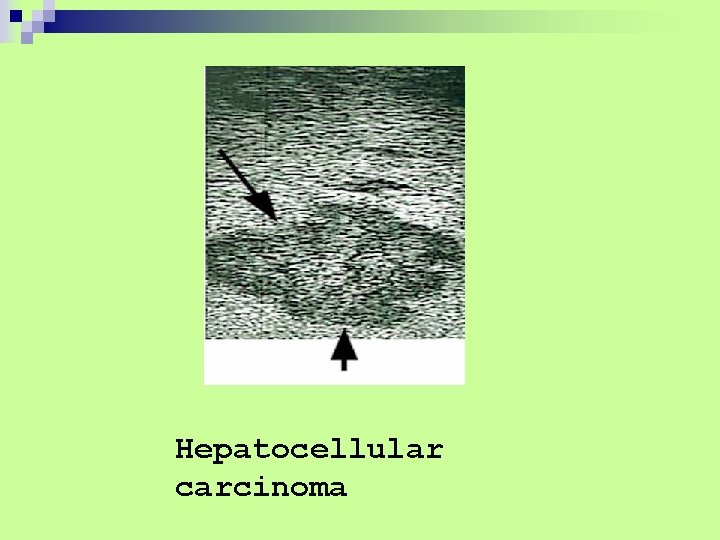
Hepatocellular carcinoma

Metastasis
Normal Gallbladder
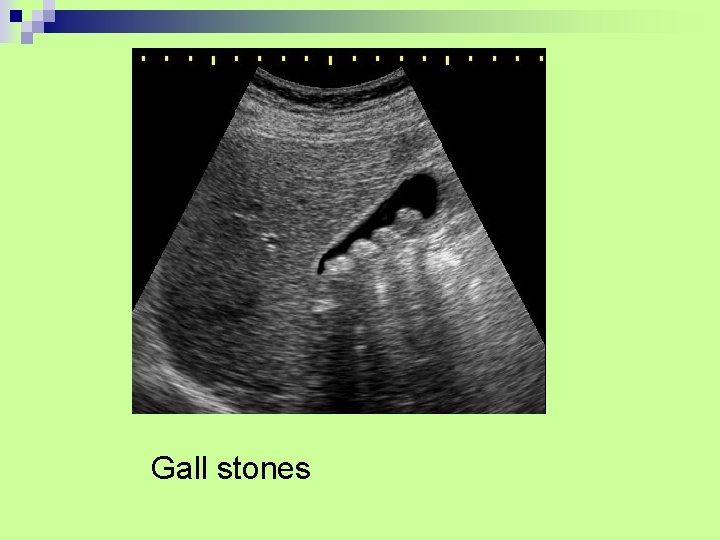
Gall stones
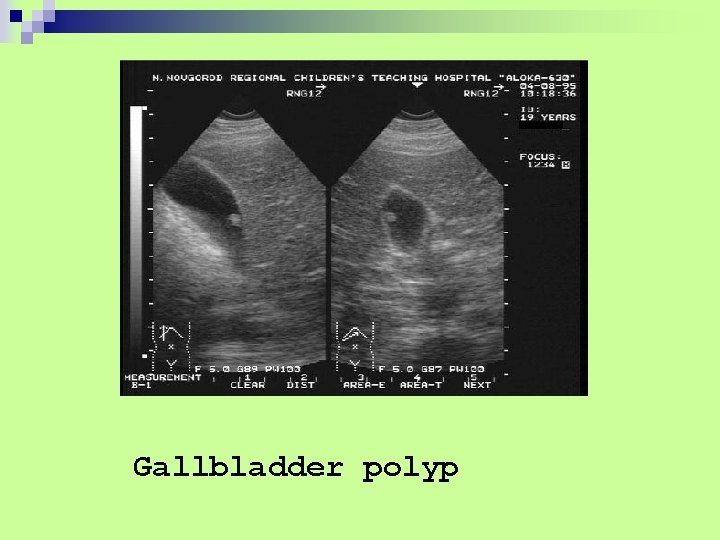
Gallbladder polyp
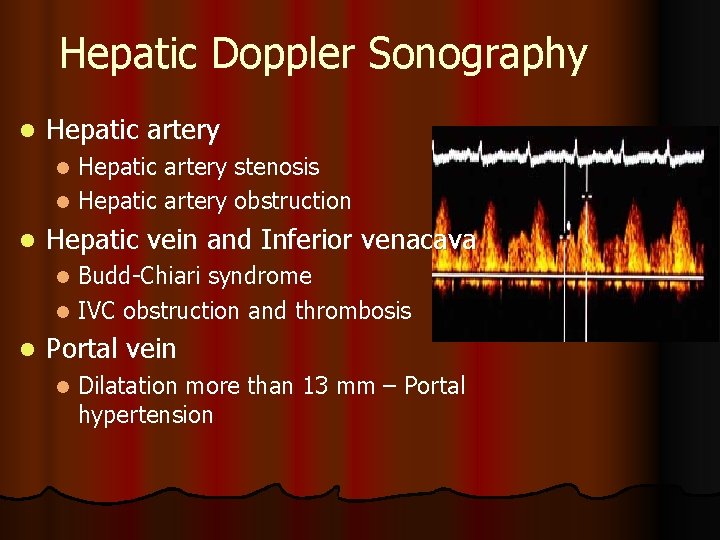
Hepatic Doppler Sonography l Hepatic artery stenosis l Hepatic artery obstruction l l Hepatic vein and Inferior venacava Budd-Chiari syndrome l IVC obstruction and thrombosis l l Portal vein l Dilatation more than 13 mm – Portal hypertension
CT Types l Single phase contrast l Dual phase contrast l Triple phase contrast
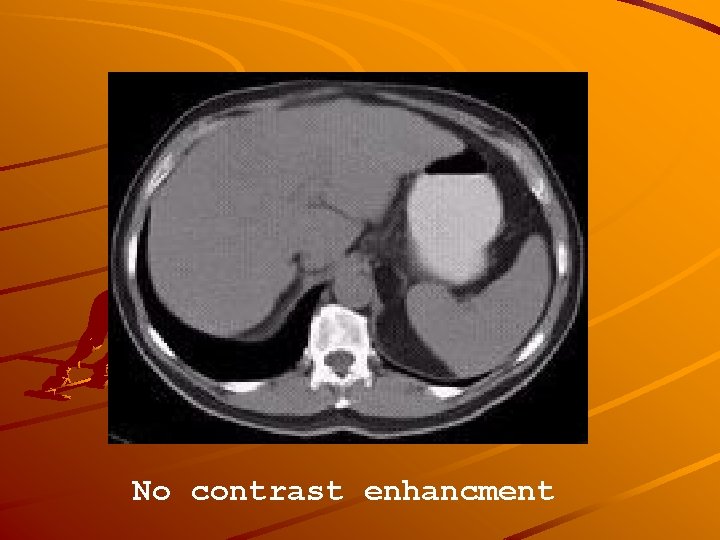
No contrast enhancment

Arterial contrast

Portal vein contrast

Fatty liver
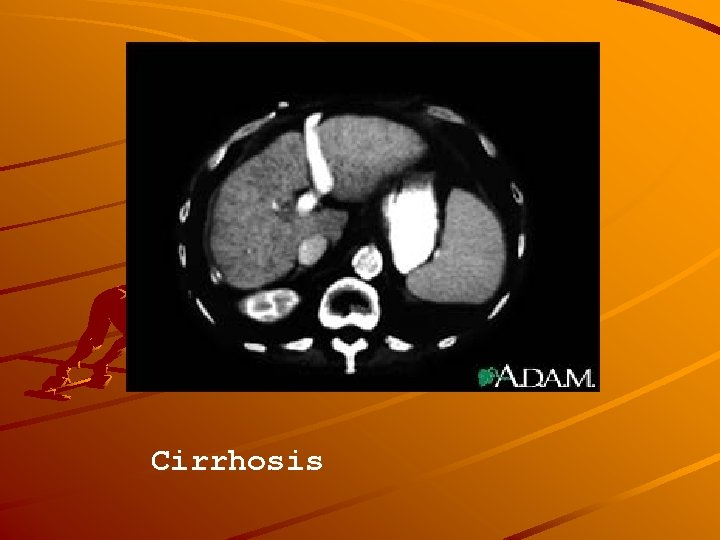
Cirrhosis

Haemochromatosis
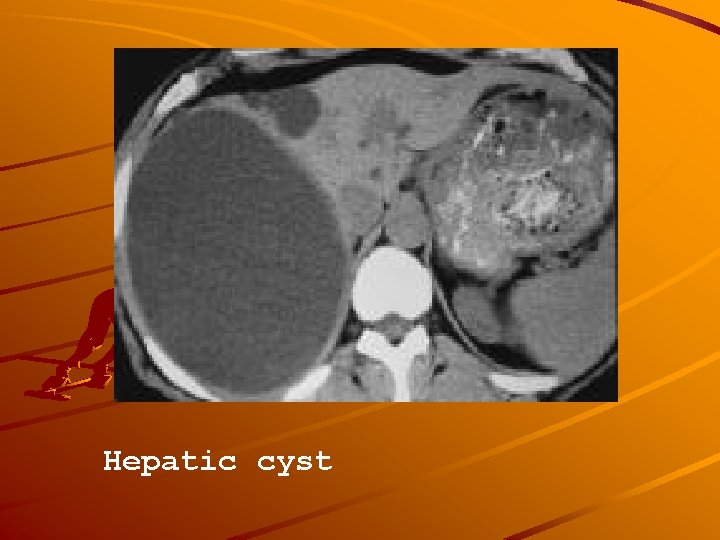
Hepatic cyst
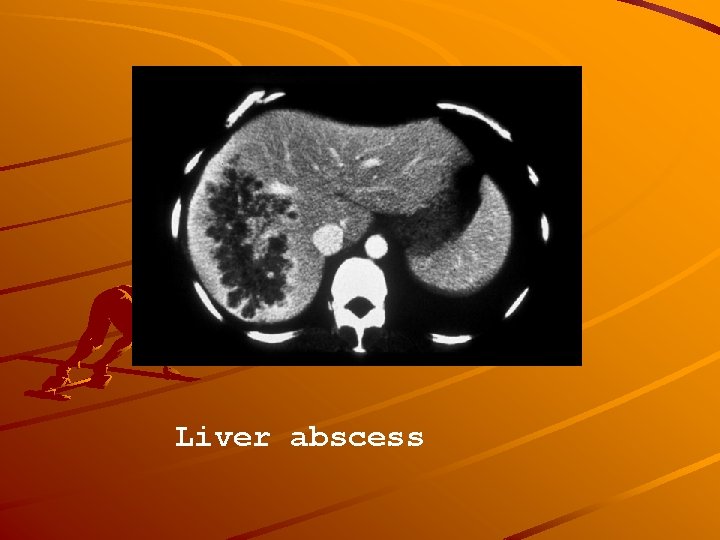
Liver abscess
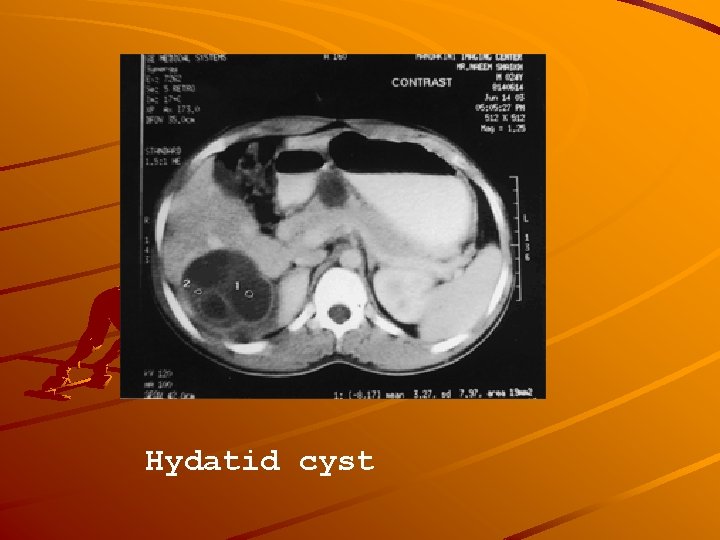
Hydatid cyst
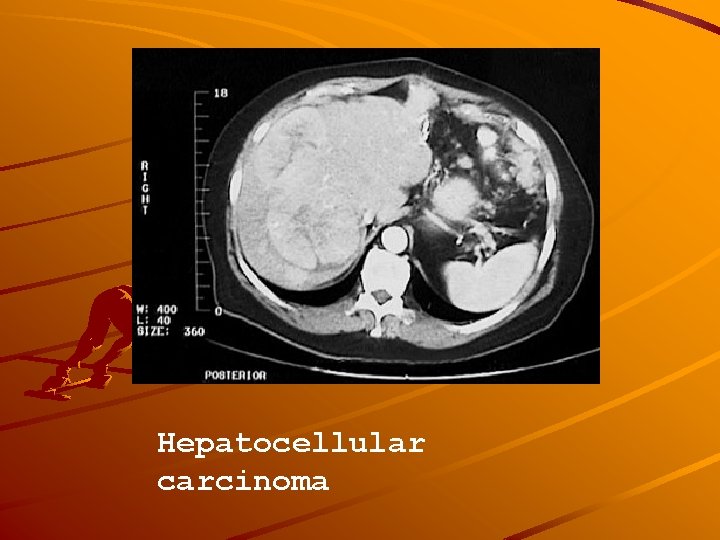
Hepatocellular carcinoma
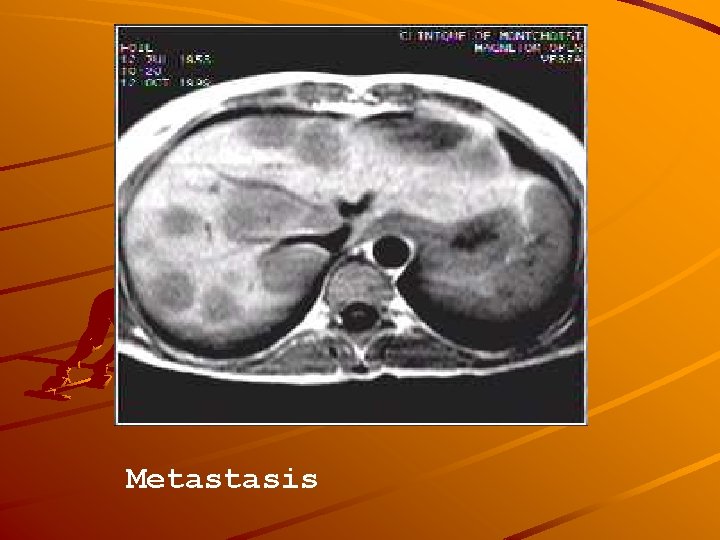
Metastasis
l Vascular abnormalities l Biliary abnormalities l Liver transplantation
MRI Not the primary modality T 1 and T 2 weighted images Fat suppression Contrast agents : Gadolinium,
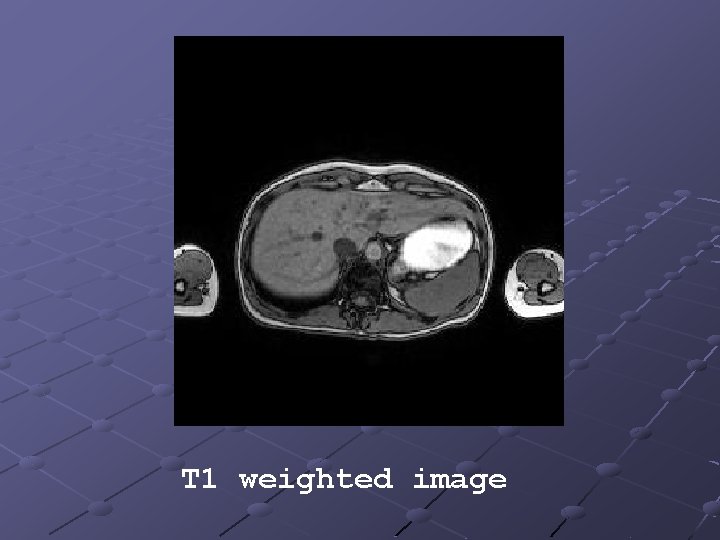
T 1 weighted image
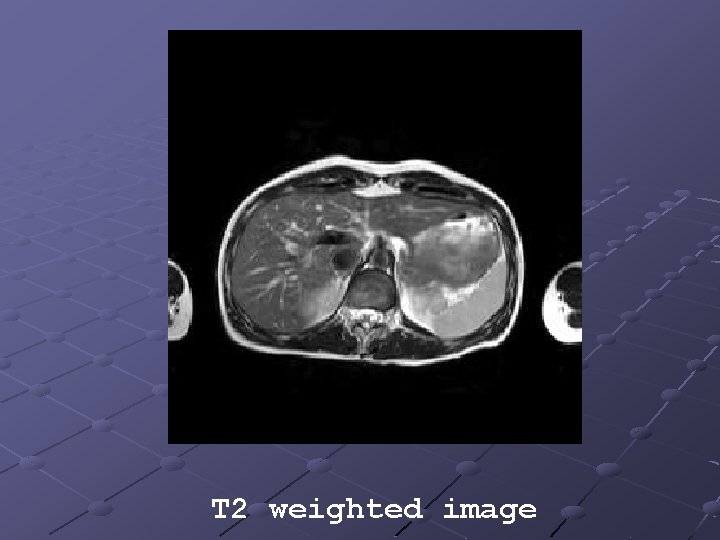
T 2 weighted image
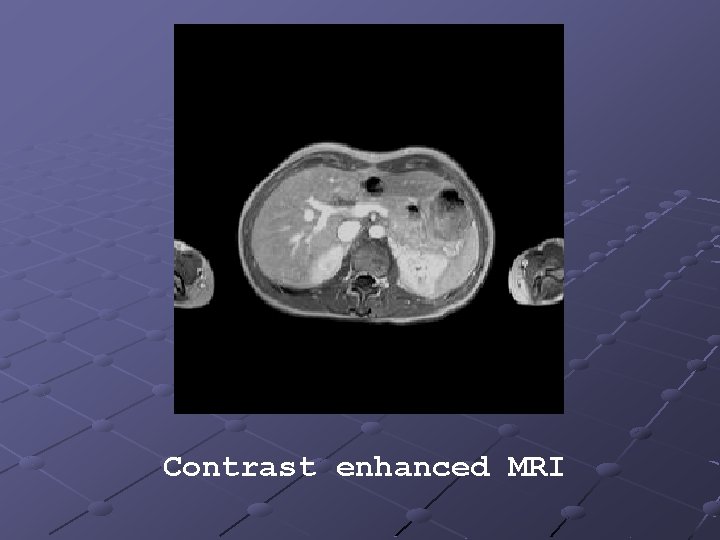
Contrast enhanced MRI
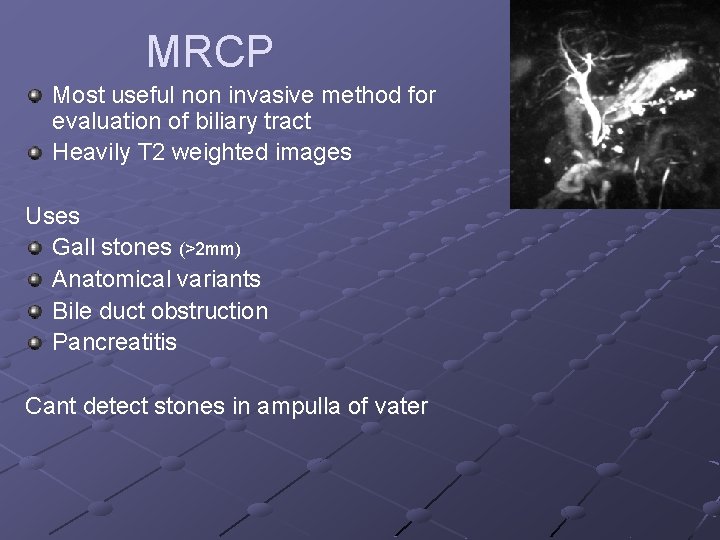
MRCP Most useful non invasive method for evaluation of biliary tract Heavily T 2 weighted images Uses Gall stones (>2 mm) Anatomical variants Bile duct obstruction Pancreatitis Cant detect stones in ampulla of vater
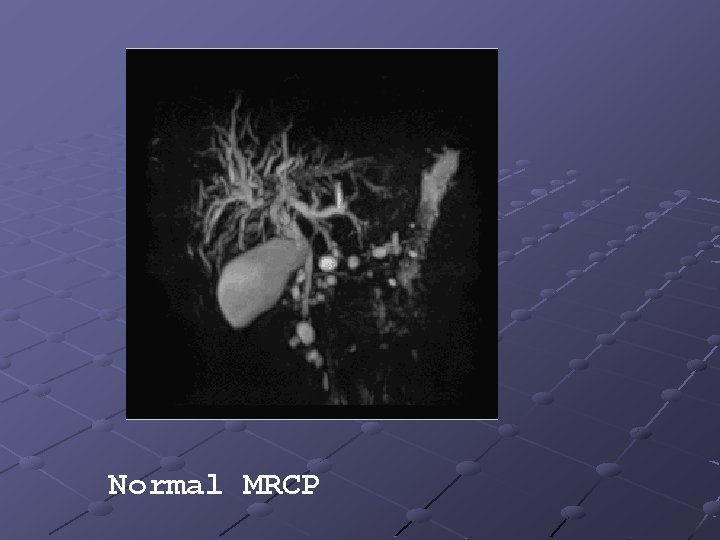
Normal MRCP
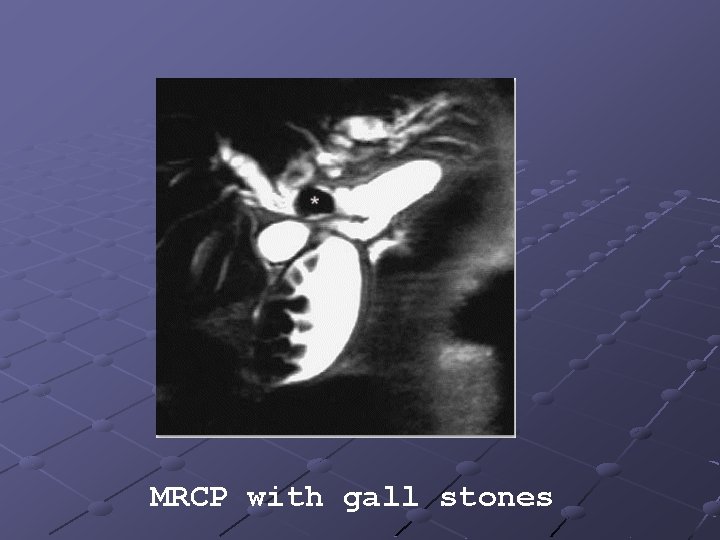
MRCP with gall stones

MRCP showing filling defect
Nuclear medicine scanning q IODIDA (Tc 99 ) scan: it is taken up by the liver and excreted in bile. Used to detect bile leak and obstruction. q Sulphur colloid scan: detects liver Kupffer cell activity. Helpful in detecting adenomas and haemangiomas which lack activity. q Fluorodeoxyglucose PET: detects malignant lesions which selectively takes up glucose.
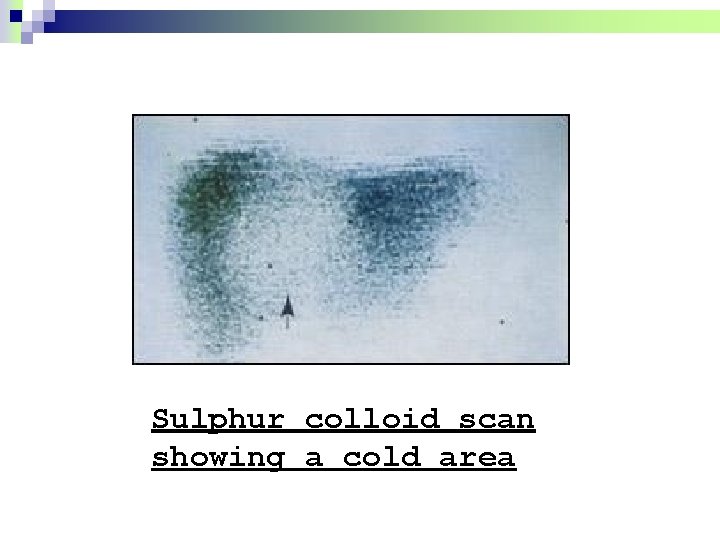
Sulphur colloid scan showing a cold area
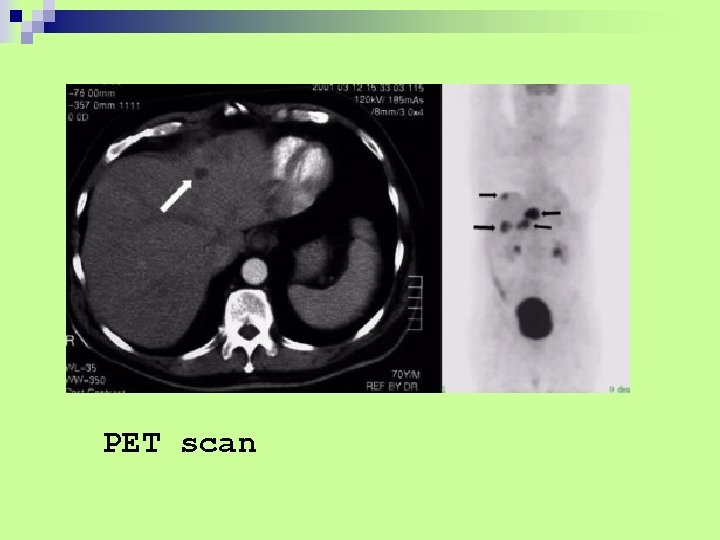
PET scan
Invasive imaging techniques l ERCP l PTC l Angiography l Laparoscopy ultrasound / laparoscopic
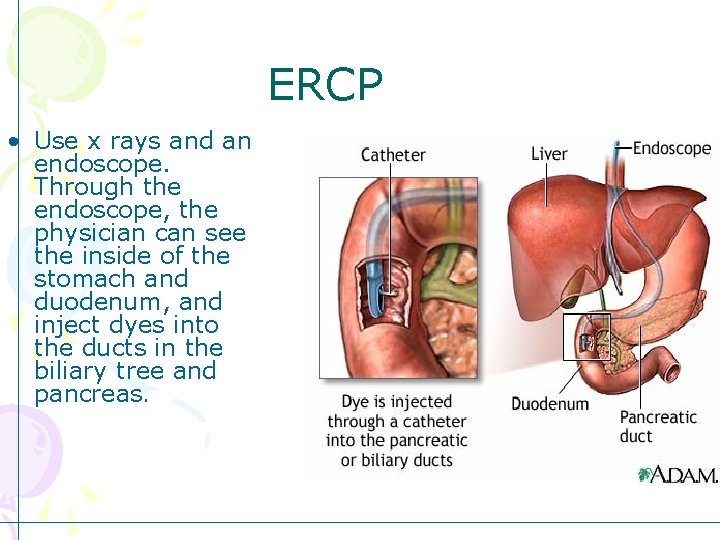
ERCP • Use x rays and an endoscope. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject dyes into the ducts in the biliary tree and pancreas.
Preparation • NOP for 8 hours • Sedation • Antibiotics
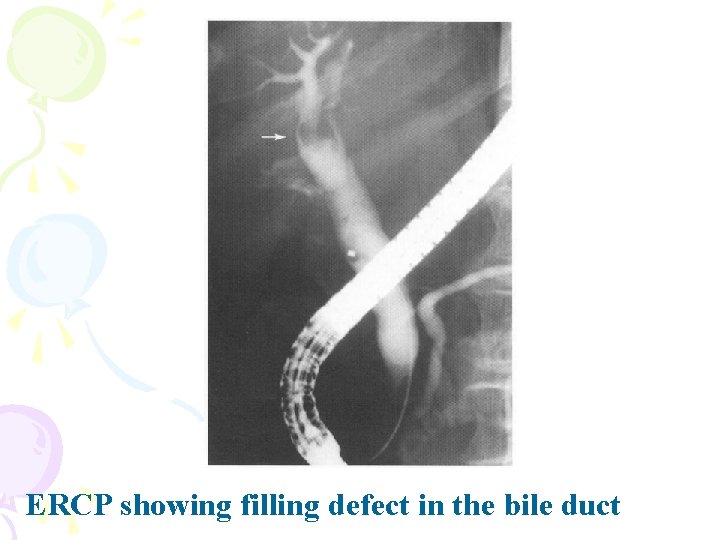
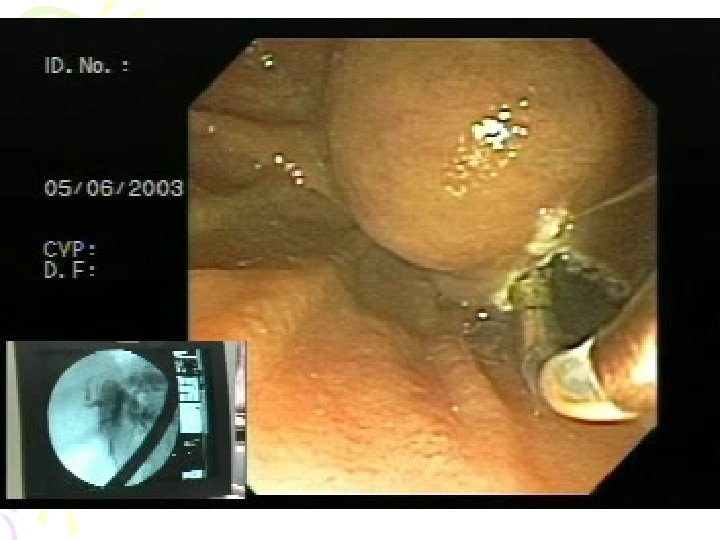
ERCP showing filling defect in the bile duct
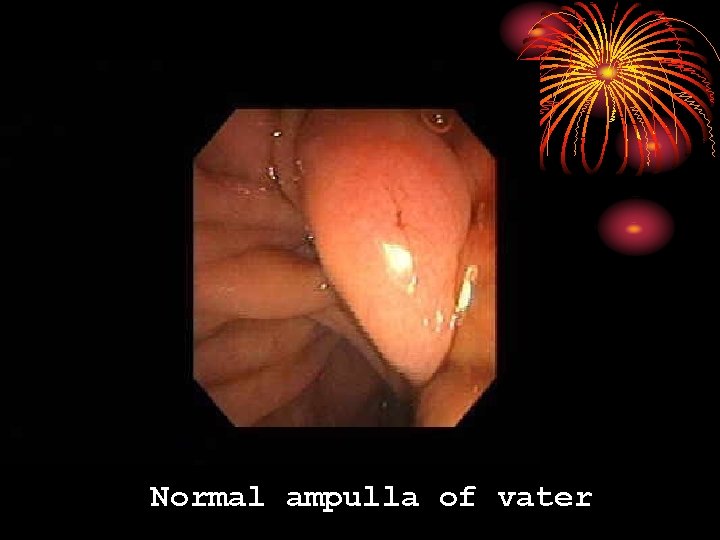
Normal ampulla of vater
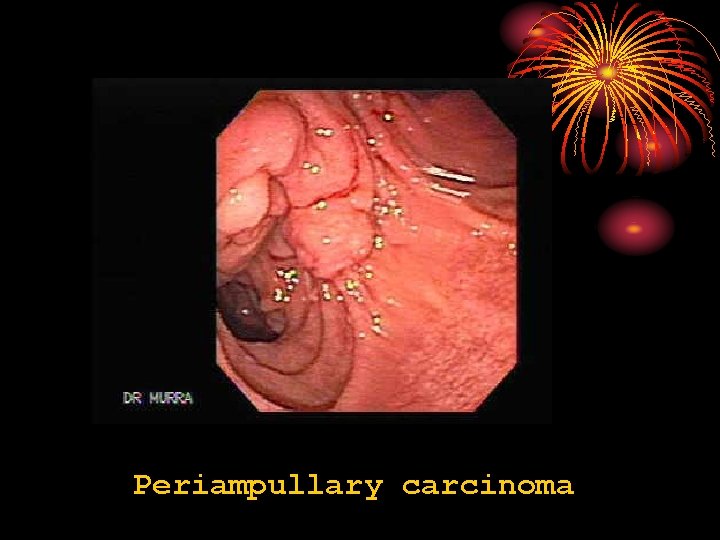
Periampullary carcinoma
Complications • • Acute pancreatitis Bleeding Colangitis Others Contraindications • Distorted bowel anatomy • Allergy to contrast agents • Coagulopathy
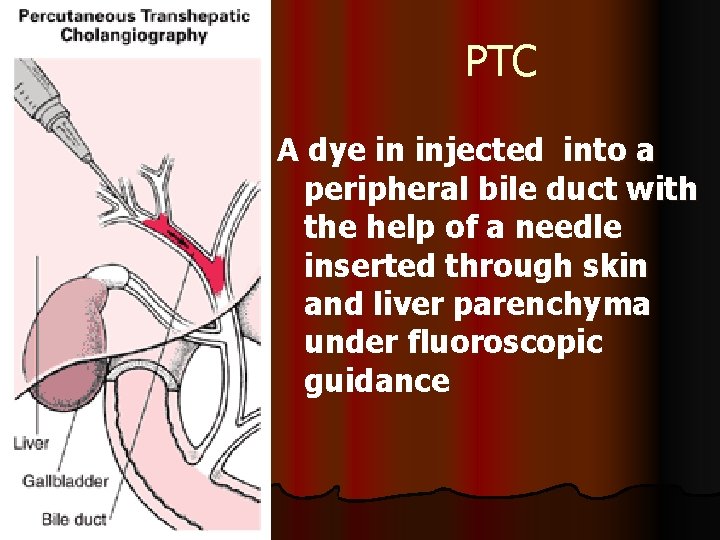
PTC A dye in injected into a peripheral bile duct with the help of a needle inserted through skin and liver parenchyma under fluoroscopic guidance
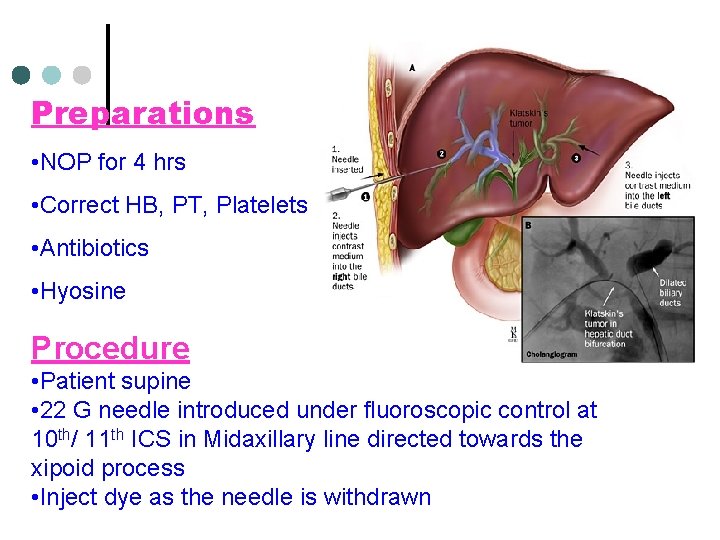
Preparations • NOP for 4 hrs • Correct HB, PT, Platelets • Antibiotics • Hyosine Procedure • Patient supine • 22 G needle introduced under fluoroscopic control at 10 th/ 11 th ICS in Midaxillary line directed towards the xipoid process • Inject dye as the needle is withdrawn

Complications • Colangitis • Bleeding • Subphrenic abscess CONTRAINDICATIONS • Bleeding disorders • Biliary tract sepsis • Hydatid disease
Angiography Diagnostic uses l Anatomy of hepatic artery prior to hepatic resection. l Confirm the patency of portal vein. l Detect nature &blood supply of tumors. Therapeutic uses l Embolisation of bleeding sites of liver. l Chemo embolisation of liver tumors
Laparoscopy & laparoscopic ultrasound Ultra sound laparoscope n n n For lesions in peritoneum, liver & blood vessels. Uses 7. 5 MHz probe with flexible tip. Helps to obtain targeted biopsies.
SUMMARY l l l l Ultrasonography: Standard first line investigation CT/MRI : Preoperative anatomical planning MRCP : 1 st line non invasive colangiography ERCP : When endoscopic intervention is anticepated PTC : Failed or impossible ERCP Angiography : Vascular involvement in tumor Laparoscopy: Peritoneal deposits, Superficial liver mets
Always treat the patient and not the results

THANK YOU
- Slides: 91