1 ABDOMINAL POSITIONING SMALL ANIMAL SPECIAL PROCEDURES Chapters
1 ABDOMINAL POSITIONING & SMALL ANIMAL SPECIAL PROCEDURES Chapters 18 & 25
2 Learning Objectives: Abdomen & Soft Tissue • Understand radiographic concerns associated with the abdomen • Properly and safely position a small animal for two common radiographic views, with the ability to: • Measure accurately • Center the x-ray beam appropriately • Image with correct borders • Properly position the patient • Understand alternate views • Identify normal abdominal anatomy, including major differences between cats and dogs

3 Small Animal Abdomen: Anatomy
4 SA Abdomen: Radiographic Concerns • Less natural contrast than thorax • Similar densities & multiple organ systems • GI gas & fat provide contrast • Contrast media often required • Generally use a higher k. Vp and lower m. As • Try for higher m. A and lower time to shorten exposure • May need two views in deep-chested dogs • Can average measurements on smaller animals
5 SA Abdomen: Radiographic Concerns • Use nonmanual restraint whenever possible • Expose at end of expiration during pause • Allows maximum space for abdominal organs • Minimize intestinal artifacts by: • Fasting 12 hours • Cleansing enema 3 -4 hours prior • Abdominal compression can reduce thickness • Can use a compression paddle • Moves underlying organ to aid in visualization • Reduces thickness so lessens scatter
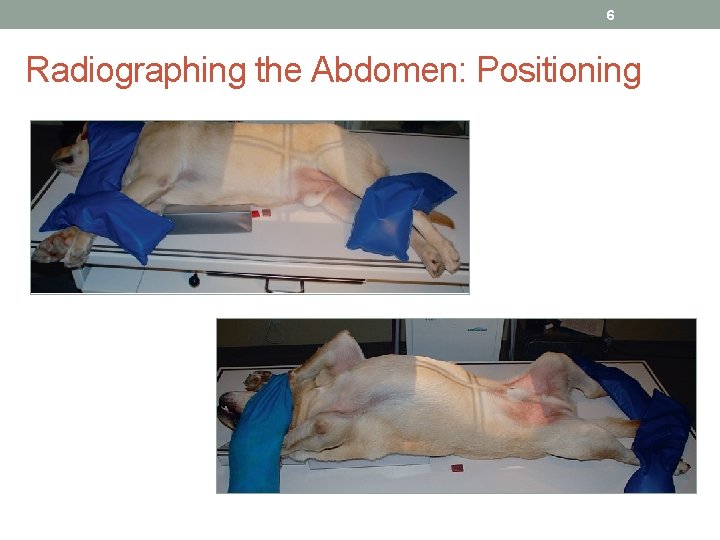
6 Radiographing the Abdomen: Positioning

7 Lateral Abdomen – Dog vs Cat
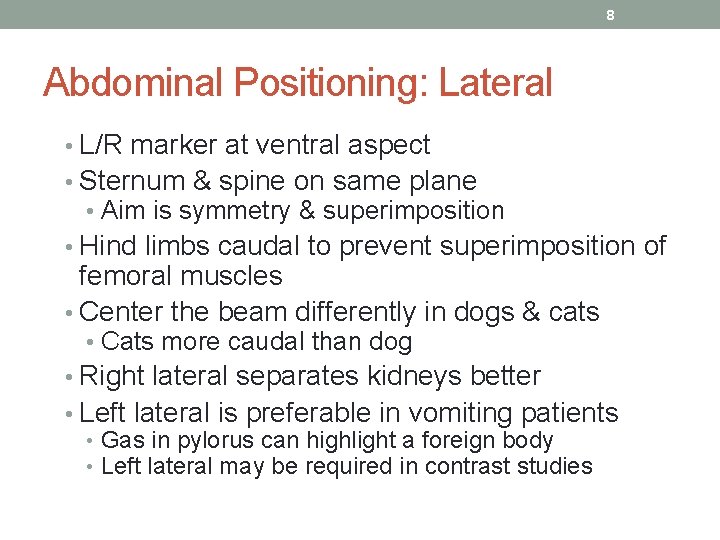
8 Abdominal Positioning: Lateral • L/R marker at ventral aspect • Sternum & spine on same plane • Aim is symmetry & superimposition • Hind limbs caudal to prevent superimposition of femoral muscles • Center the beam differently in dogs & cats • Cats more caudal than dog • Right lateral separates kidneys better • Left lateral is preferable in vomiting patients • Gas in pylorus can highlight a foreign body • Left lateral may be required in contrast studies
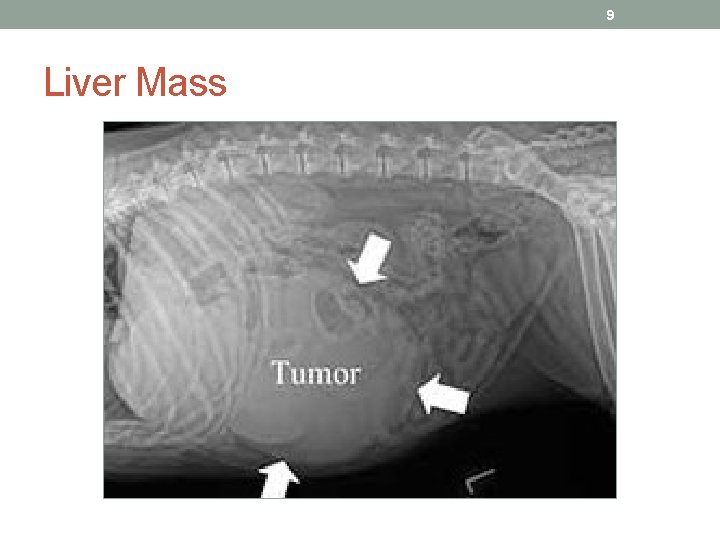
9 Liver Mass
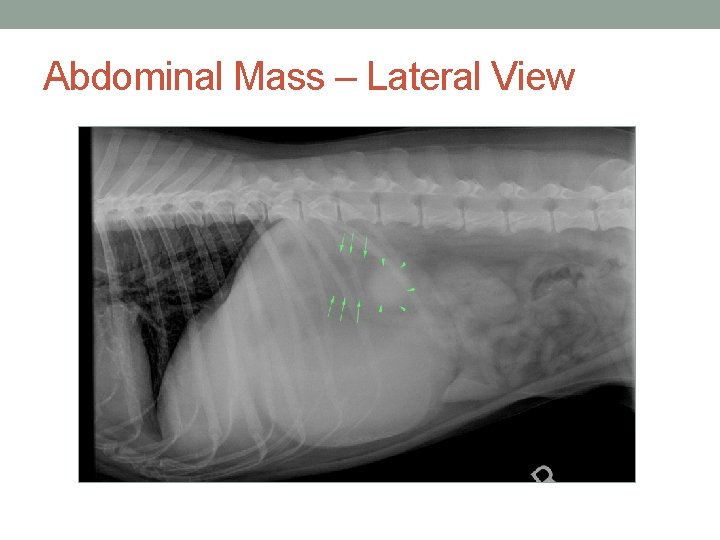
Abdominal Mass – Lateral View
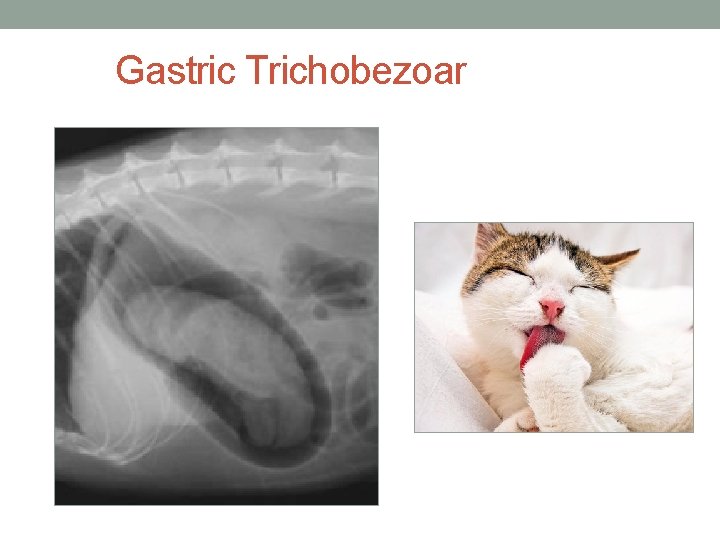
Gastric Trichobezoar
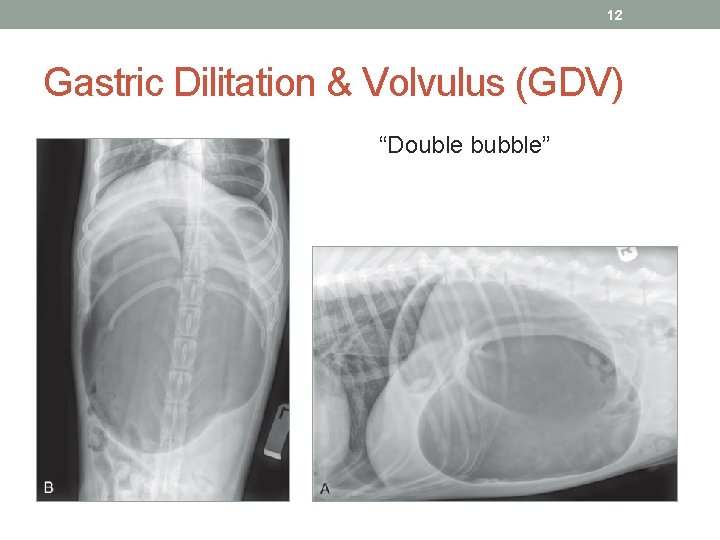
12 Gastric Dilitation & Volvulus (GDV) “Double bubble”

13 Uterine Inertia/Rupture
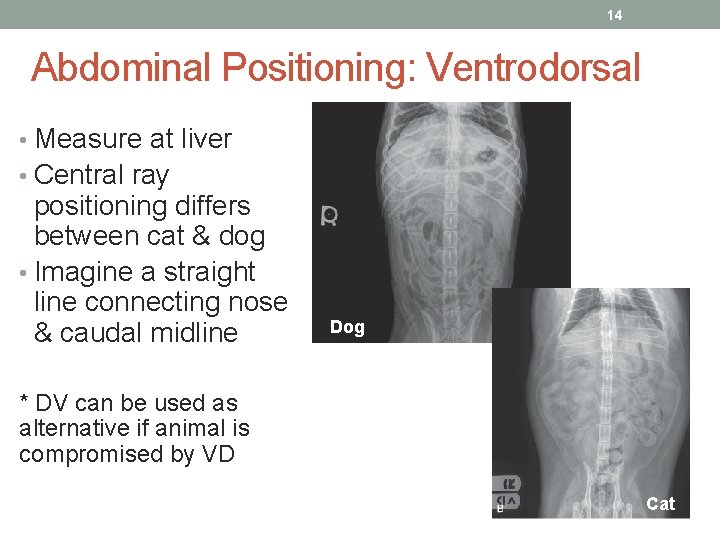
14 Abdominal Positioning: Ventrodorsal • Measure at liver • Central ray positioning differs between cat & dog • Imagine a straight line connecting nose & caudal midline Dog * DV can be used as alternative if animal is compromised by VD Cat

Abdominal Mass – VD View
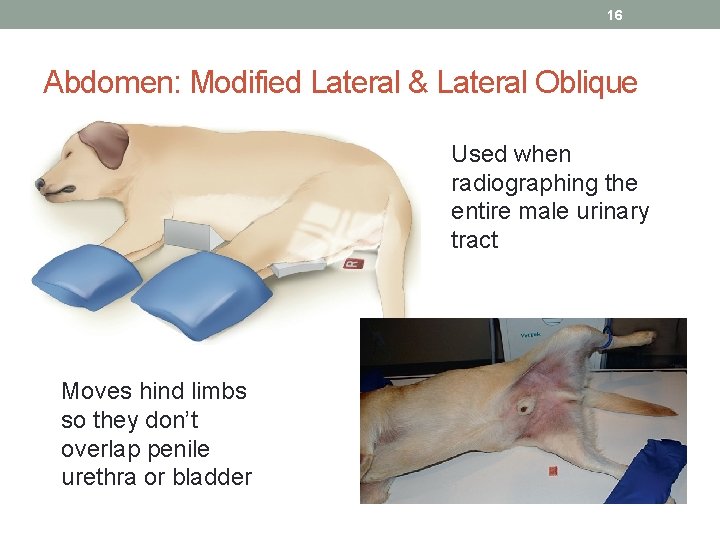
16 Abdomen: Modified Lateral & Lateral Oblique Used when radiographing the entire male urinary tract Moves hind limbs so they don’t overlap penile urethra or bladder
17 Abdominal Anatomy: Notes • Fat animals image better than emaciated ones • Fat serves as a contrasting opacity • Many normal structures hidden radiographically • Ureters, urethra, adrenals, pancreas, etc. • Abnormalities can make them visible • Liver – • Normally lies beneath ribs • Best evaluated via lateral radiograph • Stomach – • Normally within rib cage – include caudal ribs in radiograph • Food images as granular material of mixed opacity • Can be 2 -3 times larger after a meal • Gas rises and fluid moves with gravity
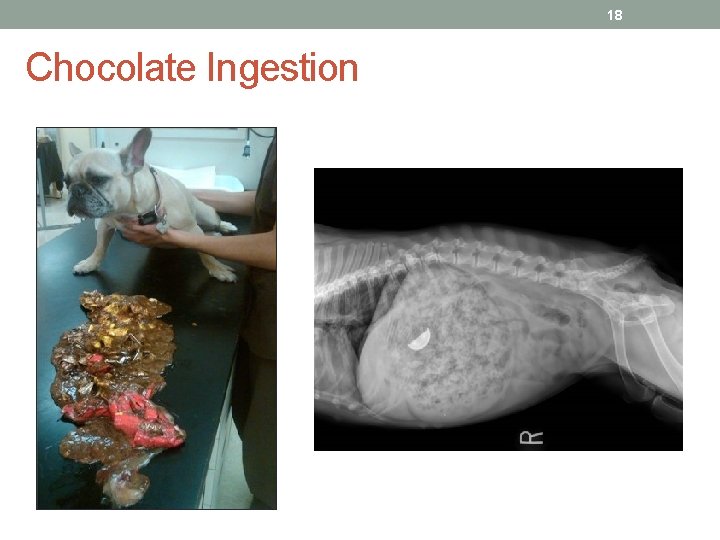
18 Chocolate Ingestion
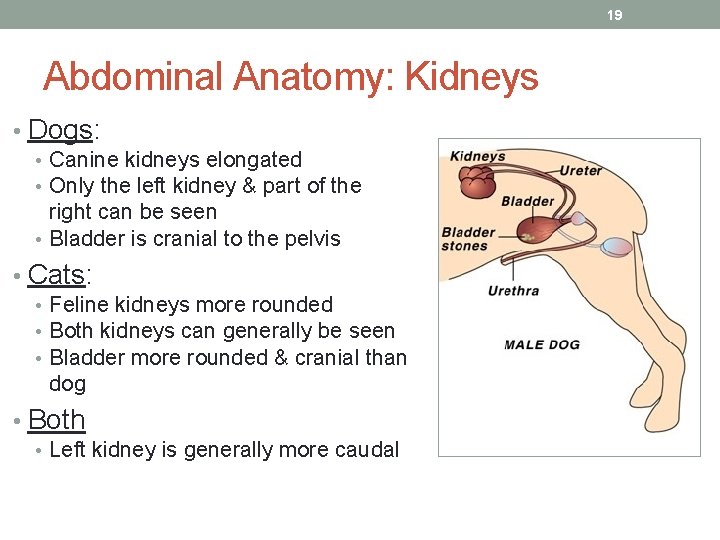
19 Abdominal Anatomy: Kidneys • Dogs: • Canine kidneys elongated • Only the left kidney & part of the right can be seen • Bladder is cranial to the pelvis • Cats: • Feline kidneys more rounded • Both kidneys can generally be seen • Bladder more rounded & cranial than dog • Both • Left kidney is generally more caudal
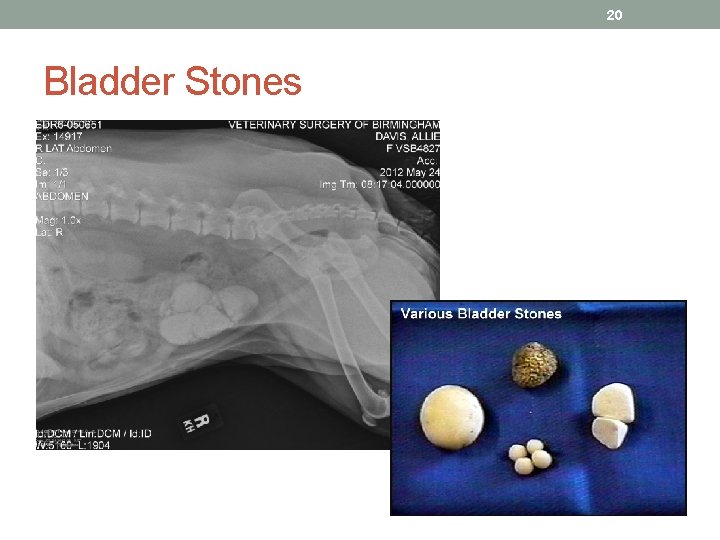
20 Bladder Stones

21 Switching gears now to… Small Animal Special Procedures
22 Special Procedures: Learning Objectives • Understand the differences between types of contrast media • Understand the appropriate patient preparation for contrast studies • Know procedures & protocols for various studies • Understand the additional modalities that can be used in addition to contrast studies • ID normal contrast anatomy
23 Special Procedures: General Principles • Contrast media attenuates the x-ray beam & can show previously unseen differences in abdominal structures. • 2 types of contrast media: • Positive-contrast: Appears white or radio-opaque • Negative-contrast: Appears dark or radiolucent • Contrast agents are used in 2 ways: • Demonstrate anatomy by outlining or filling • Demonstrate physiology via excretion through an organ
24 Special Procedures: General Principles • Contrast studies are used to: • Provide information to make a diagnosis • Evaluate a suspected lesion • Determine proper treatment • Injected contrast substance: Used to cause a difference in density & organ visibility yet still be harmless to patient • Higher k. Vps typically needed in contrast studies • Should never replace a simple survey radiograph • Ultrasound & other imaging has replaced contrast radiography in many evaluations
25 Positive-Contrast Media: Barium Sulfate • Used to radiograph the GI tract • Administer orally or rectally • Low cost & palatable • Does not alter normal physiologic function • Delineates mucosal walls well • Not absorbed in intestines • Cautions: • Cannot be used if a gastric perforation is suspected • Aspiration in lung can be fatal
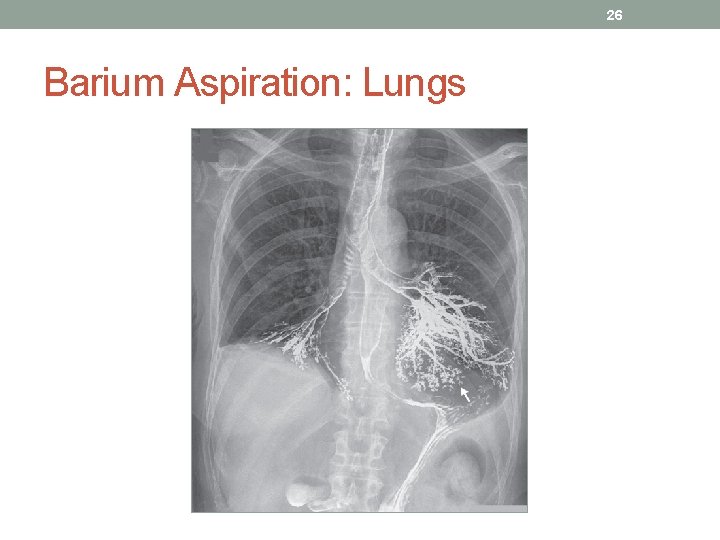
26 Barium Aspiration: Lungs
27 Positive-Contrast Media: Iodine • Use for suspected gastric perforation or obstructions • Instead of barium • Used for functional studies • Oral or injectable forms • Has a bitter taste • Nonirritating if aspirated or leaked into body cavities • Mixes with blood or body fluids & is excreted via the kidneys • More expensive than barium

28 Negative & Double-Contrast Media • Negative-contrast media: • Low atomic number or low-density agents • Air, nitrous oxide, oxygen, and carbon dioxide • Absorb fewer x-rays & appear dark on radiographs • Less mucosal detail with negative vs positive-contrast • Be careful not to over-inflate organs (bladder, etc. ) • Air embolism can lead to cardiac arrest • Double-contrast procedures: • Use both positive & negative agents • Normally used to image the urinary bladder, stomach, or colon • Negative-contrast administered first to avoid air bubbles

Negative Contrast
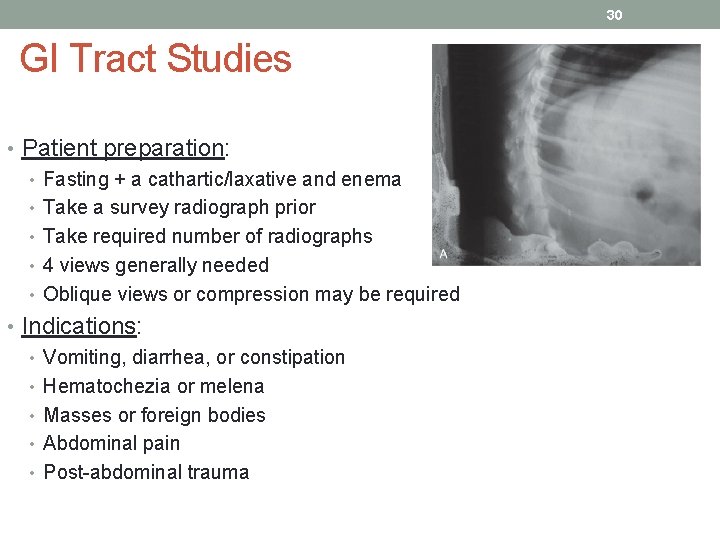
30 GI Tract Studies • Patient preparation: • Fasting + a cathartic/laxative and enema • Take a survey radiograph prior • Take required number of radiographs • 4 views generally needed • Oblique views or compression may be required • Indications: • Vomiting, diarrhea, or constipation • Hematochezia or melena • Masses or foreign bodies • Abdominal pain • Post-abdominal trauma
31 GI Tract Studies • Contraindications: • Fluid-filled esophagus or stomach • Atonic bowel • Gastric torsion • Gastric perforation • Contrast agents: • Barium is typically used because it doesn’t separate • Shake prior to use • Chilling barium for upper GI series speeds up transit time • Possibility for contamination once opened • Spilling barium on the coat will cause a radiographic artifact
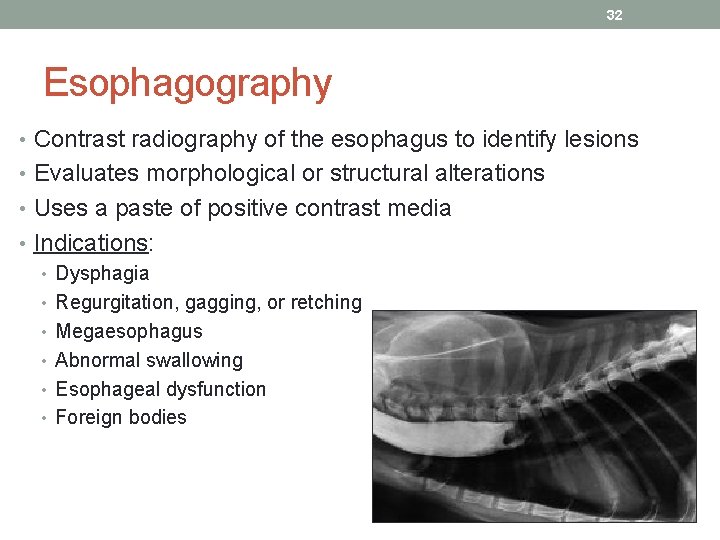
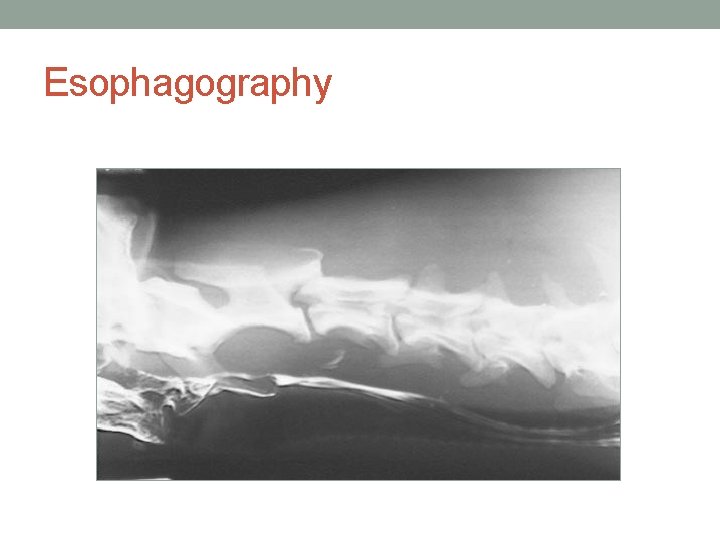
32 Esophagography • Contrast radiography of the esophagus to identify lesions • Evaluates morphological or structural alterations • Uses a paste of positive contrast media • Indications: • Dysphagia • Regurgitation, gagging, or retching • Megaesophagus • Abnormal swallowing • Esophageal dysfunction • Foreign bodies
33 Esophagography • Precautions: • Patients with dysphagia are at risk for aspiration • Contrast may not be needed if esophagus is fluid or food-filled • Patient preparation: • If evaluating megaesophagus – empty prior to administration • Fast if further GI studies are planned • Comments & tips: • Avoid barium artifacts • Pharyngeal issues are best evaluated mid-swallow
Esophagography
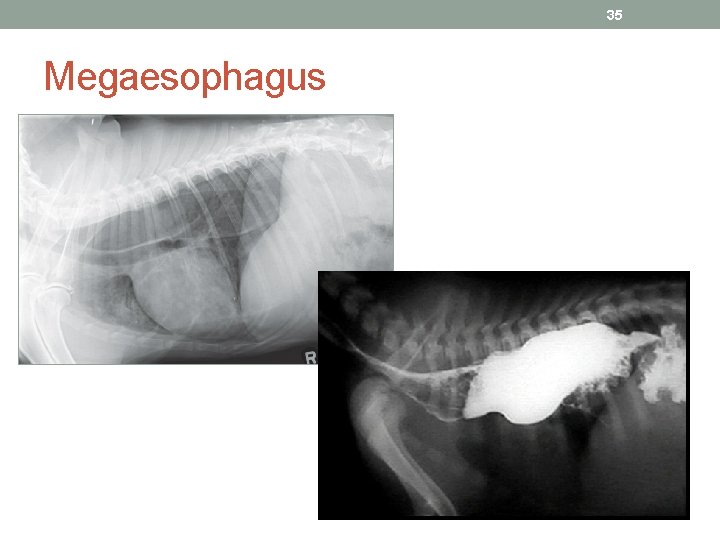
35 Megaesophagus
36 Upper GI Study • Barium is given orally, then images are taken during transit through stomach and small bowel • Studies can be done for: • Morphology – Form & structure of organs • Size, shape, and position or organs • Character of stomach wall & contents • Lesions in the GI tract • Function – How organ works • Gastric motility • Intestinal function • Indications: • Any GI irregularities (vomiting, diarrhea, anorexia, weight loss, etc. ) • Inconclusive results of survey radiograph
37 Upper GI Study • Precautions: • For suspected perforation or rupture, use iodides • Unless dehydrated or compromised – ultrasonography preferred • Delay study if full stomach • Gastric distention is not recommended immediately after gastric surgery • Patient preparation: • GI tract should be empty – fast at least 12 hours prior • Administer enema 2 -4 hours prior • If using orogastric tube - verify placement in esophagus • Before removing, clear with small amount of air and kink to prevent aspiration
38 Upper GI Study • Procedure: • Administer barium (slowly) • Take 4 radiographs centering over cranial abdomen • Both VD and lateral views at 15, 30, and 60 minutes post • Hourly radiographs until study is completed • Label films carefully • Comments & tips: • If slow GI emptying is suspected, start study early in the day • Give a sufficient volume of barium • Gastrogram is finished when the majority of barium is no longer visible in the stomach • Upper GI is complete when the barium is in the colon • Ultrasound is safer in compromised patients
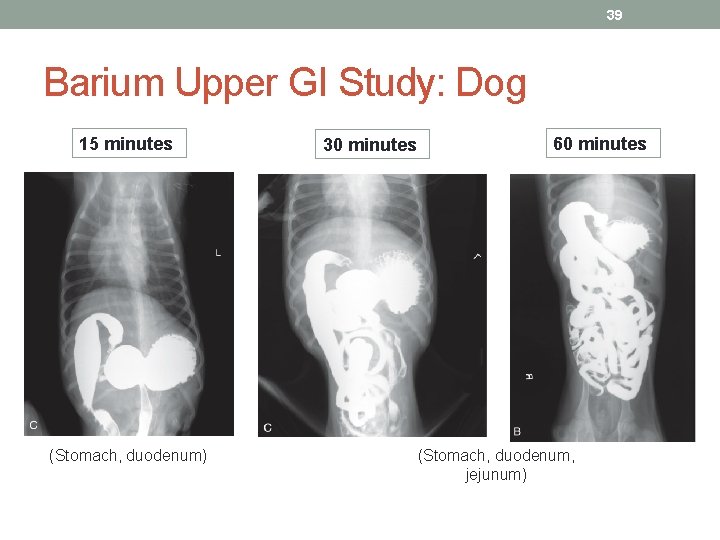
39 Barium Upper GI Study: Dog 15 minutes (Stomach, duodenum) 30 minutes 60 minutes (Stomach, duodenum, jejunum)

40 Lower GI Study • Used for examination of the cecum, colon, and rectum • Evaluates for masses and lesions • Full distention with removal of feces is required • Rectal administration of barium may be required • Sedation is usually warranted • Used when lumen narrowing prevents passing an endoscope • Indications (examples): • Abnormal defecation • Excessive mucus or bright red stool • Strictures or obstructions • Neoplasia • Colitis
41 Lower GI Study • Precautions: • No barium if a perforation is suspected • Transient spasms may occur • Patient preparation: • Fast for 24 -36 hours (water allowed until 4 hours prior) • Colon should be free of fecal matter • Cathartic & warm water enemas the night before • Avoid soapy-water enemas • Sedate or anesthetize • Take survey lateral & VD radiographs
42 Lower GI Study • Procedure: • Exposure factors may need to be increased • Have chemically restrained patient on the table • Insert catheter rectally & inflate cuff • Stop infusion if any resistance • Take 3 -view radiographs • Oblique view may be required in males • Process the films, then remove as much contrast medium as possible before removing catheter • Comments & tips: • Remove catheter away from x-ray table • Give barium in small increments
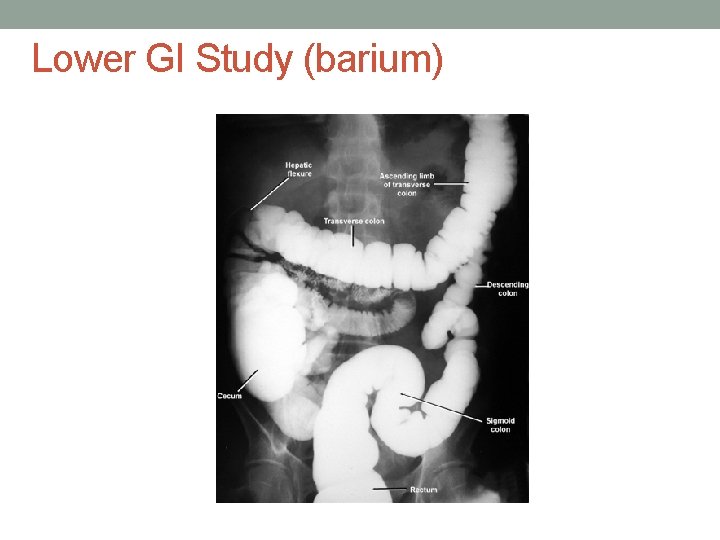
Lower GI Study (barium)
Links to Case Studies • Barium Study in a Dog (Virtuavet)- http: //virtuavet. wordpress. com/2010/ 10/26/barium-study-in-a-dog/ • 8 -Year Old Curly-Coat Retriever Takes a Long Road to a Simple Answer (Virtuavet)- http: //virtuavet. wordpress. com/2010/ 03/28/8 -year-old-curly-coat-retrievertakes-a-long-road-to-a-simpleanswer/ “Titus”
- Slides: 44